Chapter 14. Problems with endodontic treatment
P.J.C. Mitchell
SUMMARY
Problems may be encountered when carrying out endodontic treatment. A patient in pain will require emergency treatment. Achieving adequate anaesthesia allows endodontic treatment to be carried out painlessly. However, failure of anaesthesia may occur in acute inflammation; alternative techniques and supplementary anaesthesia may then be required. There may be problems during primary root canal treatment and non-surgical retreatment. These include gaining access to the root canal system, which may entail the removal of natural obstructions, previous restorations, root filling material and broken instruments; there may also be problems with preparation and filling of the root canal system. Complex problems such as instrument removal and perforation repair are often better attempted by specialists. Less complex problems are more easily approached by general dental practitioners. In this chapter, some of the common problems encountered are outlined, the decision-making process explained and the techniques of management described.
EMERGENCY TREATMENT
It is important that a patient who is in pain is rendered comfortable as soon as possible. The practice of treating the patient with antibiotics and analgesics without attempting to make a correct diagnosis and treat effectively the cause of the pain is not to be recommended. Even in an emergency situation, where the cause of the problem appears to be obvious, an accurate diagnosis must be established before any treatment is provided. This can only be achieved by taking a careful history and conducting a thorough clinical examination, followed by appropriate radiographic examination and special tests. If the clinician has no idea precisely the cause of the pain after the initial examination, active treatment should be delayed, as it might be incorrect and may cause the patient harm. 1 This should be explained to the patient, and analgesics prescribed until symptoms change and the diagnosis becomes clearer. The subject of diagnosis is covered in Chapter 3.
Although the following three conditions: acute pulpitis, acute apical periodontitis and acute periapical abscess, cause patients to present as an emergency, it must be remembered that other non-endodontic conditions can cause pain, e.g. food-packing, sinusitis, parafunction, neuropathic pain and temporomandibular joint syndrome. The differential diagnosis of dental pain in general is covered in Chapter 2.
Where the diagnosis is clear, the emergency treatment consists of applying one or more of these basic surgical principles:
• remove the cause of pain
• provide drainage if fluid exudate is present
• prescribe analgesics if required
• adjust the occlusion if indicated.
Acute pulpitis
The causes of pulp injury, its prevention and treatment have been discussed in Chapter 5. The question is often asked: at what stage should palliative treatment cease and be replaced by pulp extirpation? Ideally, the treatment should be related to the state of the pulp, but this can only be determined indirectly. The clinician thus relies on the history given by the patient and a thorough examination. As a rule of thumb, if the pulp of a mature permanent tooth causes severe and prolonged pain even after exciting factors such as thermal stimuli are removed or the patient is woken at night with pain, then it is likely that the pulp has been irreversibly damaged and pulp extirpation is indicated. The pulp may die even when the symptoms are, apparently those of reversible pulpitis. In a survey of cracked teeth, 20% of teeth without spontaneous pain or short-term response to cold eventually became necrotic. 2 Emergency pulpotomy can usually achieve pain relief, if the clinician does not have time to extirpate the entire pulp. 3 It may be difficult to anaesthetize an acutely inflamed pulp and this problem is covered later in this chapter. Antibiotics have no role in treating irreversible pulpitis. 4
Acute apical periodontitis
This may be defined as acute inflammation of the periodontium. It is often a direct result of irritation through infection of the root canal system, 5 and may be associated with acute pulpitis. A purulent exudate is not present periapically, and treatment consists of removing any pulp remnants from the root canals, irrigation of the canal system with sodium hypochlorite, drying the canals, sealing in an antibacterial dressing such as calcium hydroxide, and closure of the access cavity. The importance of cleaning the root canal system thoroughly cannot be overemphasized, and the use of ultrasonic instruments that have an internal irrigating facility helps considerably. This approach to treatment has been widely adopted by practising endodontists. 6,7
Care must be taken not to irritate the periapical tissues by extruding infected intracanal material through the apical foramen. Likewise, over-medicating the canal with an irritant drug may cause it to diffuse periapically and cause inflammation or damage to apical tissues; this is covered later in the chapter. An intracanal medicament is only placed as an empty canal can become rapidly recolonized with bacteria. 8 When a medicament is used, there is little evidence to show that the choice of medicament has any influence on postoperative pain. 9,10
The tooth may be slightly extruded and the occlusion can be relieved by grinding either the tooth itself or, in exceptional circumstances, the opposing tooth. The guiding principle on occlusal reduction should be to do no permanent harm. However, it was suggested that occlusal reduction is more effective when treating teeth with irreversible pulpitis rather than apical periodontitis. 11 Clinically, heavily worn or heavily restored teeth that require root canal treatment may need to be protected against fracture by placement of an orthodontic band; in these cases the occlusion should be adjusted. The importance of preventing a tooth from fracturing by placing a band, to act as a splint cannot be overemphasized.
Acute periapical abscess
This condition may develop as a sequel to acute apical periodontitis or present as an acute phase of chronic apical periodontitis. Accurate diagnosis may sometimes be difficult. It is common for adjacent teeth to be tender to pressure. It is essential to carry out sensitivity testing of the adjacent teeth so that the correct tooth is treated. Radiography may not be helpful as acute lesions do not become radiologically visible until bone, including the cortical plates, has been resorbed. It is often useful to take a bitewing radiograph as well as a periapical radiograph for diagnostic purposes; coronal leakage or caries may be more evident.
Where a soft tissue swelling exists, the diagnosis is generally easier, but it is important to verify the tooth that is related to the swelling. Relief of pain can be obtained speedily by obtaining drainage and adjusting the occlusion of the causative tooth. The practice of prescribing antibiotics without obtaining drainage is incorrect, and unnecessarily prolongs the patient’s misery. Opening into the pulp chamber may cause considerable discomfort because of vibration, but this can be minimized by stabilizing the tooth with fingers, and obtaining access with a small round bur in a high-speed turbine handpiece.
Ideally, the tooth should be allowed to drain until the discharge stops and then the canals irrigated gently with sodium hypochlorite, cleaned of debris and prepared fully, dressed and sealed as normal. Such a regime rarely leads to complications. 12 However, this is not always possible either because of lack of time, the tooth is exceedingly tender or there is copious discharge of exudate. In that case, it is permissible to leave the tooth on open drainage for no longer than 24 hours. At the end of this period the patient should be seen again and the root canal system cleaned of debris, irrigated with sodium hypochlorite and instrumented prior to closure. It is important that the root canal is cleaned and sealed as soon as possible so that food does not pack into the canal and invading microorganisms do not cause a further acute flare-up. The practice of leaving the canal open for weeks, if not months, has nothing to commend it13 and usually leads to periodic ‘flare-ups’ due to reinfection from the oral cavity by microorganisms that may be more difficult to eliminate. Leaving the access cavity open for a long period may also lead to caries in the pulp chamber and may make subsequent restoration of the tooth very difficult, if not impossible.
If a tooth is symptom-free while on open drainage but flares up as soon as it is sealed, then the thoroughness of debridement must be questioned. This is probably the commonest cause of postoperative flare-up, for no tooth will settle until the root canal system is thoroughly cleaned. The coronal seal must be effective so if the clinical crown contains caries or inadequate restorations, these must be removed. Sometimes because of anatomical difficulties, or the presence of an immovable obstruction in the root canal, it may not be possible to obtain drainage through the canal. In such instances emergency treatment will depend on the presence or absence of swelling. If a swelling is present and fluctuant, incision and drainage, or aspiration through a large bore needle into a syringe are advisable and this generally relieves acute pain. If there is no swelling, supportive antibiotic therapy may be appropriate, followed by non-surgical or surgical endodontic treatment (see Chapter 10) when the acute symptoms have subsided.
Acute flare-up
Following instrumentation of a symptom-free tooth, in the majority of cases, the patient can expect little pain. If the patient has severe pain, or an established periapical lesion prior to treatment, the likelihood of severe postoperative pain is higher. 9,14 The intensity of pain will reduce with time and is substantially helped by prescribing analgesics so that the pain intensity is reduced after 24 to 48 hours. Patients who present with pain and swelling during a flare-up are best managed by prescribing analgesics and antibiotics. 9 If tolerated, ibuprofen prescribed in 600–800 mg doses is one of the most effective non-steriodal anti-inflammatory drugs for acute dental pain. 15 If the patient is unable to tolerate ibuprofen or aspirin, then paracetamol (acetaminophen) is the analgesic of choice. Flare-ups are more likely to occur in teeth with necrotic pulps,16.17. and 18. and with atopic patients, for example, those who suffer from allergies. 17 The incidence of flare-ups has been reported to be as low as 2.5% in teeth undergoing root canal treatment; 18 this is a reflection of the high standard of treatment. A much higher incidence of pain could be expected where treatment is inadequate, or infected debris is extruded through the apical foramen. The incidence of extrusion of debris through the apical foramen is lower when the root canal is prepared using a Crown-down approach and with a Balanced-force technique, than with a Step-back approach and a filing technique. 19
FAILURE OF ANAESTHESIA IN ACUTE INFLAMMATION
Profound analgesia is essential for pulpotomy or vital pulp extirpation, yet there are occasions where, in spite of normally sufficient dosage and satisfactory technique, adequate analgesia is not obtained. Such occasions are distressing for the patient and embarrassing for the dentist. The main reasons for failure are given below and the subject has been reviewed. 20
The term ‘hot tooth’ has been used to describe such a situation. The tooth may be excessively stimulated by heat or cold, and may be tender to bite; it may be difficult, if not impossible, to achieve analgesia of sufficient depth despite repeated local anaesthetic injections. The reasons for this failure are not entirely clear although various explanations have been proposed:
• Pulpal inflammation in the affected tooth produces chemical mediators which cause hyperexcitability of the nerve fibres, particularly C-fibres. The local anaesthetic solution is, therefore, unable to block the conduction of all these impulses. 21
• There is usually increased vascularity of the tissues in the region of the inflamed tooth and hence the local anaesthetic may be more rapidly removed by the bloodstream, shortening its period of duration. 22
• It has been shown that there is a tendency for inflammation to increase sensory nerve transmission so countering the effects of anaesthetics. 23
• There is a possible spread of inflammatory mediators along the myelin sheaths of nerves, which restrict the absorption of the local anaesthetic; this is likely to contribute only a small part. 24
• The pH of inflammatory products in the region of the tooth may be more acidic, thus making the local anaesthetic solution potentially less effective; however, this is considered unlikely. 22
Alternative anaesthetic techniques
In endodontic practice, the failure to obtain analgesia ultimately is an infrequent occurrence, and when it does occur it is likely to be with a mandibular molar tooth. 25 It must be noted that an acutely inflamed pulp can remain very painful, in spite of what appears to be an otherwise satisfactory inferior dental nerve block injection. In such instances, several alternative techniques are available:
• application of a sedative dressing to the pulp
• intrapulpal anaesthesia
• intraosseous anaesthesia
• sedation.
Application of a sedative dressing to the pulp
Occasionally, the kindest management of the patient is to accept failure of local anaesthesia, dress the tooth to reduce pulpal inflammation and attempt pulpal extirpation on a subsequent occasion. The pulp may be sedated with a zinc oxide–eugenol dressing, 26 or with a corticosteroid-antibiotic dressing. 27,28
If the pulp has been exposed and is inflamed, it bleeds copiously and should be allowed to do so for 2–3 minutes to wash out inflammatory mediators. The exposure is then covered with a pledget of cotton wool damped with a medicament such as Ledermix (Haupt Pharma GmbH, Wolfratshausen, Germany). The cotton wool is covered by a fortified zinc oxide–eugenol cement. On the subsequent visit, a local anaesthetic should again be given, and when it appears effective the pulp should be extirpated. It is usually possible to achieve effective anaesthesia, when it had not been on the previous occasion.
Intrapulpal anaesthesia
This may be used to supplement existing inadequate anaesthesia. The technique consists of injecting local anaesthetic solution into the pulp. The needle is advanced into the pulp chamber and the solution injected under pressure; initial pain may be reduced by placing topical anaesthetic gel on the exposed pulp prior to injection. Most topical anaesthetic gels contain either benzocaine or lidocaine (lignocaine) at concentrations of 20–30%. Intracanal use of a topical anaesthetic is also helpful when ‘hot’ vital pulp tissue is encountered apically.
Intraosseous anaesthesia
Intraosseous injections of anaesthetic may be delivered either via the periodontal ligament or through the cortical plate. They may be used to supplement existing inadequate anaesthesia. 25 In the case of periodontal ligament injections, special syringes allow small, preset increments of anaesthetic solution to be injected intraosseously through the periodontal ligament. The anaesthetic capsule is inserted into an autoclavable protective sleeve to guard against breakage and a 30-gauge ultra-short needle is used to inject the solution into the ligament. Prior to injection, the gingival sulcus must be disinfected and the soft tissues anaesthetized to reduce discomfort during injection. The primary injection is given on the distal aspect of the tooth, and the needle with the bevel towards the root face is slid into the periodontal ligament space until it is stopped by alveolar bone. The lever is squeezed extremely slowly and about 0.2 ml of anaesthetic solution deposited. The procedure may be repeated on the mesial aspect of the tooth, and in the case of molars on other surfaces.
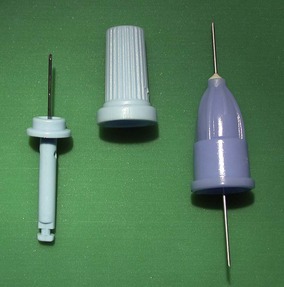
Intraosseous anaesthetic techniques such as the Stabident system (Fairfax Dental, Miami, FL, USA) use a small disposable ‘perforator’ to create a hole in the cortical plate of bone through the attached gingiva (Fig 14.1). The soft tissues must be adequately anaesthetized first. Anaesthetic is then delivered into the cancellous bone, within the mandible or maxilla, with a matching needle. Both periodontal ligament injection and injection through the cortical plate produce effective and rapid intraosseous anaesthesia.
 |
| Figure 14.1
Stabident system, consisting of the perforator, perforator cap and injection needle.
|
These techniques have some disadvantages:
• Infection can be introduced into the tissues unless the soft tissues have been disinfected beforehand.
• The injections are painful unless surface anaesthetic and/or conventional anaesthetic have been administered first.
• Adrenaline (epinephrine) injected intraosseously is rapidly absorbed intravenously. This may result in a noticeable tachycardia. It may, therefore, be wise to use non-adrenaline containing anaesthetics for these injections in patients with cardiac conditions.
• Periodontal ligament injections alter the occlusion of the tooth very slightly by raising it out of its socket, and a careful check of the occlusion of the temporary restoration must be made.
• The anaesthetic is usually only effective for periods of up to 30 minutes.
• It may be difficult to locate the entrance created with the perforator with the injection needle. The X-Tip system (Dentsply, Addlestone, Surrey, UK) overcomes this problem by using a hollow perforator through which the injection needle can be inserted.
Sedation
There are rare and exceptional cases where the use of relative analgesia or intravenous sedation is the only way that a vital pulp can be extirpated, or an abscess drained. Generally, the reasons are not related to the effectiveness of local anaesthesia but to the attitude of the patient. In such instances, before embarking on such a course, the clinician must be satisfied that the patient is fit, the tooth is of sufficient importance to the patient’s well-being, and that the patient will accept subsequent treatment without recourse to further intravenous sedation. For further information on sedation the reader is referred elsewhere.29.30.31. and 32.
PROBLEMS WITH PREPARATION OF THE ROOT CANAL SYSTEM
Access cavity preparation
The preoperative radiograph must be examined carefully prior to beginning root canal treatment in order to detect the position of the coronal pulp chamber, the position of the canals and the presence of any obstructions that might prevent instrumentation. Access cavity position may vary in teeth that have been ‘occlusally realigned’ with cast restorations. It is essential to prepare a sufficiently large access cavity so that there are no visual or physical restrictions; the entire roof of the pulp chamber should be removed. If the tooth has been restored with a satisfactory crown, it may be left in place during endodontic treatment. Removal of the crown with a crown and bridge remover (see below) may improve access but hinder rubber dam placement. Use of magnification and axial light will eliminate most access problems when working through a crown. If the crown is technically deficient or secondary caries is present, it should be removed along with any caries, prior to endodontic treatment. Pulp space anatomy and access cavities are covered in Chapter 4.
Problems with primary preparation of the root canal
During primary (non-retreatment) preparation of the root canal, the clinician may encounter various natural problems, which may hinder biomechanical debridement of the entire root canal system. These include intracanal hard tissue formation and acute canal curvature.
Intracanal hard tissue formation
Pulp stones
Pulp stones are not uncommon and may be identified from preoperative radiographs; they normally present little difficulty in removal when ultrasonic instrumentation is utilized. Piezo-electric powered ultrasonic devices are far more efficient for this purpose than magnetostrictive units. The instrument should be worked around the edge of the stone until it becomes loose. It is more difficult, however, to remove a stone from a root canal, particularly if it is attached to the canal wall. In such an instance, if a file can be passed alongside the stone, it may be removed by careful filing.
Tertiary dentine
Tertiary dentine is formed as a sequel to microbiological or physical trauma. Careful examination of the pulp space on the preoperative radiograph will show its size and to what extent it has been filled with tertiary dentine. The depth of the floor of the pulp chamber from the occlusal surface of the tooth should be assessed from the preoperative radiograph; it is essential to have an undistorted image. This should help prevent damage to the floor of the pulp chamber. Tertiary dentine in the original pulp space should be removed carefully with an ultrasonic instrument or a long-shank bur in the slow-speed handpiece. Diamond-coated ultrasonic tips (CPR tips, Sybron Endo, Orange, CA, USA) or periodontal scaling tips (PS tips, EMS, Nyon, Switzerland) are particularly well suited to removing tertiary dentine. They are designed for piezo-electric ultrasonic units and should be used with copious coolant; inadequate cooling may cause burning of the dentine.
Good lighting and magnification is helpful as this dentine is normally very different in colour and texture to primary dentine; it may vary from being porous and yellow in colour to hard, dark and dense. Use of an endodontic explorer (DG16) is highly recommended to help detect the canal orifices. Periodically, the operator should stop and assess whether the cavity is in the correct position. Where the pulp chamber is only partially obliterated, the patent canal orifices are useful landmarks for orientation. If a canal orifice remains elusive, a radiograph should be taken to check that the cavity is not deviating off course in a mesio-distal direction. Once the explorer will stick in the canal orifice, it is usually possible to negotiate the canal with a fine file (e.g. ISO size 06).
Canals that are completely calcified from the pulp chamber to the apical foramen are very rare. Calcification normally begins in the pulp chamber and continues in an apical direction as a result of mild pulpal inflammation. Sometimes, canals that look completely calcified on a radiograph can be instrumented because a very fine pathway remains within the calcified material. This may not be visible on the radiograph because of inadequate contrast or large film-grain size. For this reason, where endodontic treatment is indicated, an attempt should normally be made to negotiate a fine canal using a small sized file (e.g. ISO size 06), rather than opting for surgery in the first instance (Fig. 14.2). The tertiary dentine which occludes the canal should be removed with an ultrasonic instrument or a long-shank bur in a slow-speed handpiece. Intracanal tertiary dentine is usually much darker than primary dentine, and so magnification and illumination are once again, of great help. Once the canal is patent, preparation is relatively simple. A lubricant with chelating properties such as Slickgel ES (Sybron Endo, Orange, CA, USA) or File-Eze (Ultradent Products, South Jordan, UT, USA) will help to reduce the resistance of a file in a fine canal. It should be made clear that a symptomless tooth with a calcified canal but no periapical radiolucency does not require root canal treatment. 33
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses




