Clinical Diagnosis
1. The gingival diseases (Box 29-1)
2. The various types of periodontitis (Table 29-1)
TABLE 29-1
Features of Types of Periodontitis
| Parameter | Chronic | Aggressive | Prepubertal | Localized Aggressive Periodontitis | Necrotizing Ulcerative Periodontitis |
| Age (years) | 35+ | 20 to 35 | <11 | 11 to 19 | 15 to 35 |
| Calculus | Moderate to abundant | Scanty to moderate | Scanty | Moderate | Scanty |
| Disease progression | Slow | Rapid | Rapid | Rapid | Rapid |
| Distribution | Generalized; associated with etiologic factors | Generalized; no consistent pattern | Primary molars and incisors | First molars and incisors, and no more than two other teeth | ? |
| Prevalence* | United States, >50%; Sri Lanka, 81% | United States, 4% to 5%; Sri Lanka, 11% | ? | <0.50% | ? |
| Racial predilection | No | No | No | More common among blacks | No |
| Familial tendency | No | ? | Yes | Yes | ? |
| Gender distribution | More severe among men | ? | ? | ? | ? |
| Polymorphonuclear leukocyte/macrophage defects | No | Yes | Yes | Yes | Yes |
| Association with systemic problems | No | Some cases | Yes | Yes | Yes |
| Response to therapy | Very good | Variable | Poor | Good | Variable |
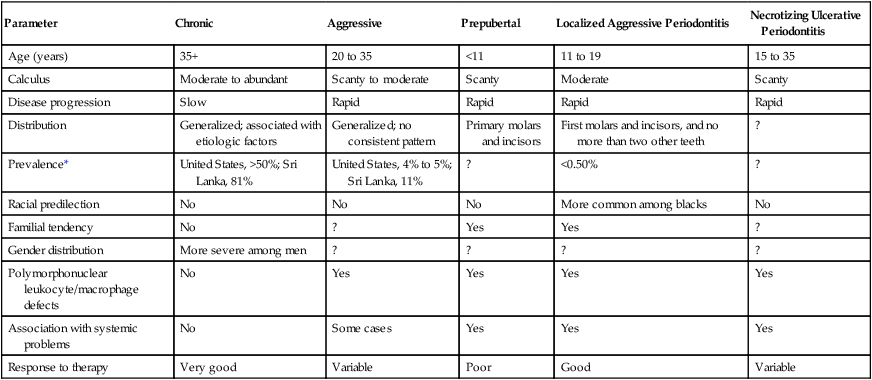
*Prevalence among adolescents between the ages of 14 and 17 years in the United States.
3. The periodontal manifestations of systemic diseases (see Chapter 11)
First Visit
Overall Appraisal of the Patient
Medical History
Most of the medical history is obtained at the first visit, and it can be supplemented by pertinent questioning at subsequent visits. The health history can be obtained verbally by questioning the patient and recording his or her responses on a blank piece of paper or by means of a printed questionnaire that the patient completes. Figure 29-1 is the medical questionnaire form recommended by the American Dental Association.
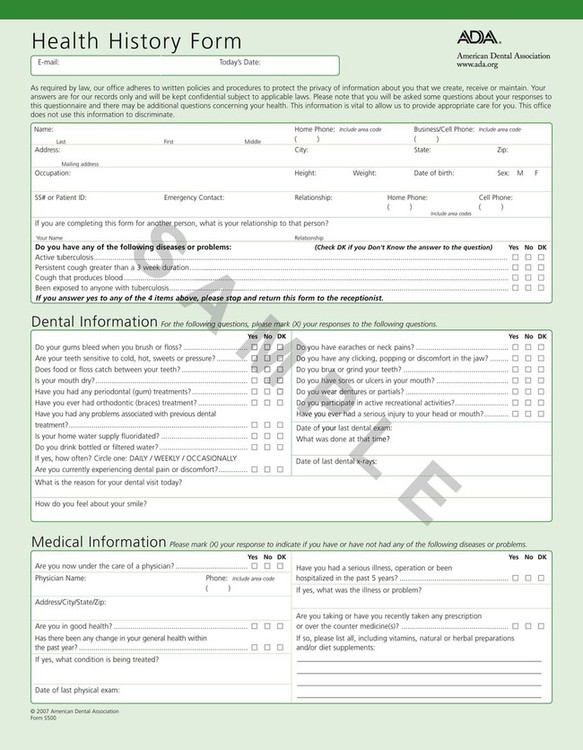
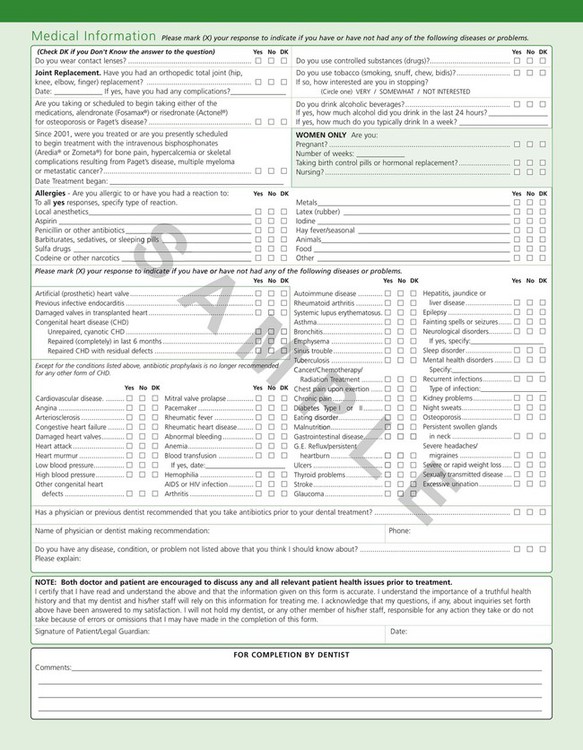
The importance of the medical history should be clearly explained, because patients often omit information that they cannot relate to their dental problems. The patient should be made aware of the following: (1) the possible role that some systemic diseases, conditions, or behavioral factors may play in the cause of periodontal disease; (2) the presence of conditions that may require special precautions or modifications of the treatment procedure (see Chapter 37); and (3) the possibility that oral infections may have a powerful influence on the occurrence and severity of a variety of systemic diseases and conditions (see Chapter 12).
The medical history should include reference to the following:
1. If the patient is under the care of a physician, the nature and duration of the problem and its therapy should be discussed. The name, address, and telephone number of the physician should be recorded, because direct communication with him or her may be necessary.
2. Details regarding hospitalizations and operations, including the diagnosis, the type of operation, and any untoward events (e.g., anesthetic, hemorrhagic, or infectious complications) should be provided.
3. A list of all medications being taken and whether they were prescribed or obtained over the counter should be included. All of the possible effects of these medications should be carefully analyzed to determine their effect, if any, on the oral tissues and also to avoid administering medications that would interact adversely with them. Special inquiry should be made regarding the dosage and duration of therapy with anticoagulants and corticosteroids. Patients who are taking the family of drugs called bisphosphonates (e.g., Actonel, Fosamax, Boniva, Aredia, Zometa), which are often prescribed for patients with osteoporosis, should be cautioned about possible problems related to osteonecrosis of the jaw after undergoing any form of oral surgery involving the bone.
4. All medical problems (e.g., cardiovascular, hematologic, endocrine), including infectious diseases, sexually transmitted diseases, and high-risk behavior for human immunodeficiency virus infection, should be listed. Chapter 26 discusses the subject of human immunodeficiency virus infection.
5. Any possibility of occupational disease should be noted.
6. Abnormal bleeding tendencies, such as nosebleeds, prolonged bleeding from minor cuts, spontaneous ecchymoses, a tendency toward excessive bruising, and excessive menstrual bleeding, should be cited. These symptoms should be correlated with the medications that the patient is taking.
7. The patient’s allergy history should be taken, including that related to hay fever, asthma, sensitivity to foods, sensitivity to drugs (e.g., aspirin, codeine, barbiturates, sulfonamides, antibiotics, procaine, laxatives), and sensitivity to dental materials (e.g., eugenol, acrylic resins).
8. Information is needed regarding the onset of puberty and for females, menopause, menstrual disorders, hysterectomy, pregnancies, and miscarriages.
9. A family medical history should be taken, including that of bleeding disorders and diabetes.
Dental History
Current Illness.
A preliminary oral examination is done to explore the source of the patient’s chief complaint and to determine whether immediate emergency care is required. If this is the case, the problem is addressed after the consideration of the medical history (see Chapters 41 and 42).
The dental history should include reference to the following:
1. Visits to the dentist should be listed, including their frequency, the date of the most recent visit, the nature of the treatment, and oral prophylaxis or cleaning by a dentist or hygienist, including the frequency and date of most recent cleaning.
2. The patient’s oral hygiene regimen should be described, including toothbrushing frequency, time of day, method, type of toothbrush and dentifrice, and interval at which brushes are replaced. Other methods for mouth care, such as mouthwashes, interdental brushes, other devices, water irrigation, and dental floss, should also be listed.
3. Any orthodontic treatment, including its duration and the approximate date of termination, should be noted.
4. If the patient is experiencing pain in the teeth or in the gingiva, the manner in which the pain is provoked, its nature and duration, and the manner in which it is relieved should be described.
5. Note the presence of any gingival bleeding, including when it first occurred; whether it occurs spontaneously, on brushing or eating, at night, or with regular periodicity; whether it is associated with the menstrual period or other specific factors; and the duration of the bleeding and the manner in which it is stopped.
6. A bad taste in the mouth and areas of food impaction should be mentioned.
7. Assess whether the patient’s teeth feel “loose” or insecure, if he or she has any difficulty chewing, and whether there is any tooth mobility.
8. Note the patient’s general dental habits, such as grinding or clenching of the teeth during the day or at night. Do the teeth or jaw muscles feel “sore” in the morning? Are there other habits to address, such as tobacco smoking or chewing, nail biting, or biting on foreign objects?
9. Discuss the patient’s history of previous periodontal problems, including the nature of the condition, and, if it was previously treated, the type of treatment received (surgical or nonsurgical) and the approximate period of termination of the previous treatment. If, in the opinion of the patient, the present problem is a recurrence of previous disease, what does he or she think caused it?
10. Note whether the patient wears any removable prosthesis. Does the prosthesis enhance or is it a detriment to the existing dentition or the surrounding soft tissues?
11. Does the patient have implants to replace any of the missing teeth?
Intraoral Radiographic Survey
The radiographic survey should consist of a minimum of 14 intraoral films and 4 posterior bite-wing films (Figure 29-2).
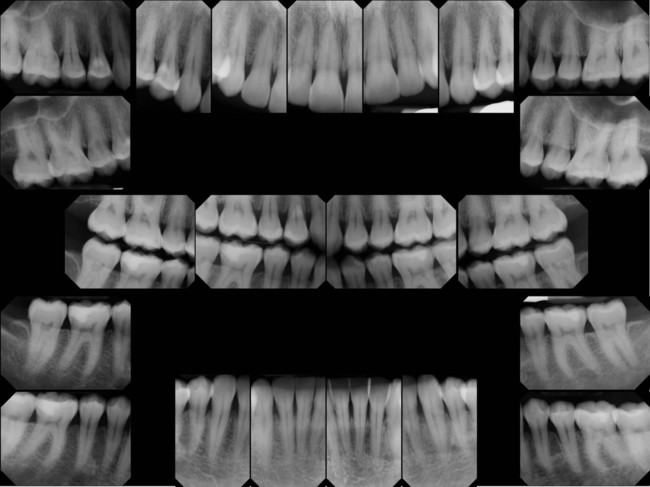
Panoramic radiographs are a simple and convenient method of obtaining a survey view of the dental arch and the surrounding structures (Figure 29-3). They are helpful for the detection of developmental anomalies, pathologic lesions of the teeth and jaws, and fractures as well as for the dental screening examinations of large groups. They provide an informative overall radiographic picture of the distribution and severity of bone destruction with periodontal disease, but a complete intraoral series is required for periodontal diagnosis and treatment planning. Chapter 31 gives a detailed description of radiographic interpretation in periodontics.
Second Visit
Oral Examination
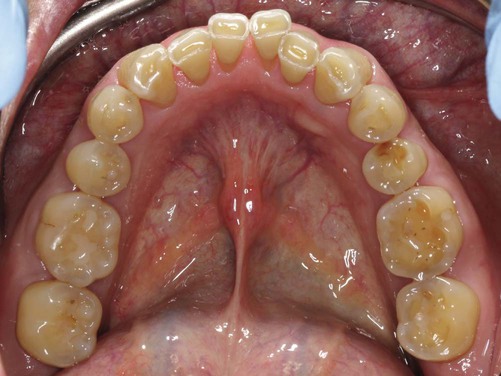
Oral Hygiene.
The cleanliness of the oral cavity is appraised in terms of the extent of accumulated food debris, plaque, and tooth surface stains (Figure 29-4). Disclosing solution may be used to detect plaque that would otherwise be unnoticed. The amount of plaque detected, however, is not necessarily related to the severity of the disease present. For example, aggressive periodontitis is a destructive type of periodontitis in which plaque is minimal. Qualitative assessments of plaque are more meaningful, and their value for diagnosis is discussed in Chapter 8.
Oral Malodor.
Oral malodor, which is also termed fetor ex ore, fetor oris, or halitosis, is a foul or offensive odor that emanates from the oral cavity. Mouth odors may be of diagnostic significance, and their origin may be either oral or extraoral (remote).58 Chapter 52 discusses in detail the problems related to oral malodor.
Examination of the Teeth and Implants
Wasting Disease of the Teeth.
Wasting is defined as any gradual loss of tooth substance, which is characterized by the formation of smooth, polished surfaces without regard to the possible mechanism of this loss. The forms of wasting are erosion, abrasion, and attrition.42,60
Erosion, which is also called corrosion, is a sharply defined wedge-shaped depression in the cervical area of the facial tooth surface.50 The long axis of the eroded area is perpendicular to the vertical axis of the tooth. The surfaces are smooth, hard, and polished. Erosion generally affects a group of teeth. During the early stages, it may be confined to the enamel, but it generally extends to involve the underlying dentin as well as the cementum.
The etiology of erosion is not known. Decalcification by acidic beverages40 or citrus fruits in combination with the effect of acid salivary secretion are suggested causes. Sognnaes66 refers to these lesions as dentoalveolar ablations and attributes them to forceful frictional actions between the oral soft tissues and the adjacent hard tissues. In patients with erosion, the salivary pH, the buffering capacity, and the calcium and phosphorus content have been reported as normal, and the mucin level is elevated.39
Toothbrushing22 with an abrasive dentifrice (Figure 29-5) and the action of clasps are frequently mentioned, but aggressive toothbrushing is the most common cause.30 Tooth position (facial) is also a major factor in the abrasive loss of the root surface. The degree of tooth wear from toothbrushing depends on the abrasive effect of the dentifrice and the angle of brushing.37,38 Horizontal brushing at right angles to the vertical axis of the teeth results in the severest loss of tooth substance. Occasionally, abrasion of the incisal edges occurs as a result of habits such as holding objects (e.g., bobby pins, tacks) between the teeth.

Occlusal or incisal surfaces worn by attrition are called facets. When active tooth grinding occurs, the enamel rods are fractured and become highly reflective to light.74 Thus, shiny, smooth, and curviplanar facets are usually the best indicator of ongoing frictional activity. If dentin is exposed, a yellowish brown discoloration is frequently present (Figure 29-6). Facets vary with regard to size and location, depending on whether they are produced by physiologic or abnormal wear.12,72 At least one significant wear facet has been reported in 92% of adults,63 and facet prevalence approaches universality.10,73 Facets are usually not sensitive to thermal or tactile stimulation.
Facets generally represent functional or parafunctional wear as well as iatrogenic dental treatment through coronoplasty (occlusal adjustment). However, coronoplasty does not appear to contribute to higher ratings of wear.64 Excessive wear may result in the obliteration of the cusps and the formation of either a flat or a cuneiform (cupped-out) occlusal surface. Contrary to earlier thought, attrition in young adults from modern societies is not age related.15,64 This suggests that a significant amount of attrition, when present in young adults, is unlikely to occur as a result of functional wear,32 and it is probably the result of bruxing activity.64 Attrition has been correlated with age when older adults are considered.7,62
The angle of the facet on the tooth surface is potentially significant to the periodontium. Horizontal facets tend to direct forces on the vertical axis of the tooth to which the periodontium can adapt most effectively. Angular facets direct occlusal forces laterally and increase the risk of periodontal damage. However, gradual attrition may be compensated for by continuous tooth eruption without alveolar bone growth, and it is characterized by a lack of inflammatory changes on the alveolar bone surfaces.69
Another mechanism of tooth wear that has been studied recently is called abfraction, and it results from occlusal loading surfaces causing tooth flexure and mechanical microfractures and tooth substance loss in the cervical area.24
Tooth Mobility.
All teeth have a slight degree of physiologic mobility, which varies for different teeth and at different times of the day.47,51 It is greatest when arising in the morning, and it progressively decreases. The increased mobility in the morning is attributed to slight extrusion of the tooth as a result of limited occlusal contact during sleep. During the waking hours, mobility is reduced by chewing and swallowing forces, which intrude the teeth in the sockets. These 24-hour variations are less marked in persons with a healthy periodontium than in those with occlusal habits such as bruxism and clenching.
Single-rooted teeth have more mobility than multi-rooted teeth, with incisors having the most mobility. Mobility occurs primarily in a horizontal direction, although some axial mobility occurs to a lesser degree.49
Tooth mobility occurs in the following two stages:
1. The initial or intrasocket stage occurs when the tooth moves within the confines of the periodontal ligament. This is associated with viscoelastic distortion of the ligament and the redistribution of the periodontal fluids, interbundle content, and fibers.31 This initial movement occurs with forces of about 100 lb, and it is on the order of 0.05 mm to 0.10 mm (50 µm to 100 µm).43
2. The secondary stage occurs gradually and entails the elastic deformation of the alveolar bone in response to increased horizontal forces.45 When a force of 500 g is applied to the crown, the resulting displacement is about 100 µm to 200 µm for incisors, 50 µm to 90 µm for canines, 8 µm to 10 µm for premolars, and 40 µm to 80 µm for molars.43
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses