Chapter 26 Technology and Esthetics
Section A Minimally Invasive Dentistry: Dental Procedures and Technology
Relevance of Minimally Invasive Dentistry to Esthetic Dentistry
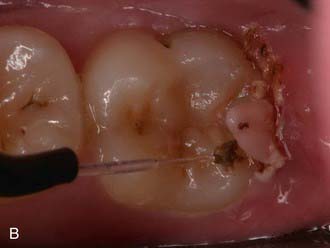
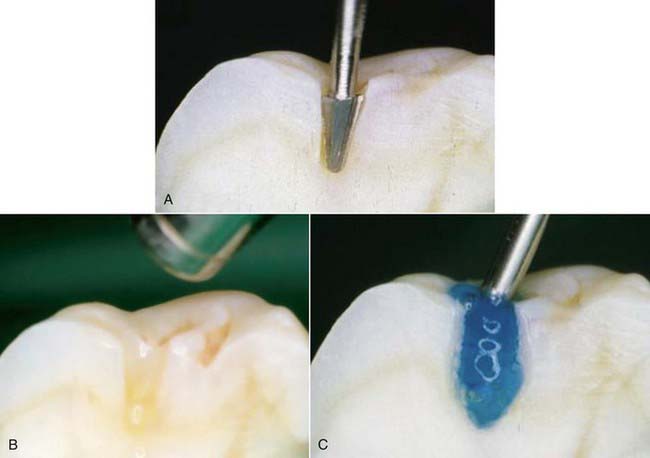
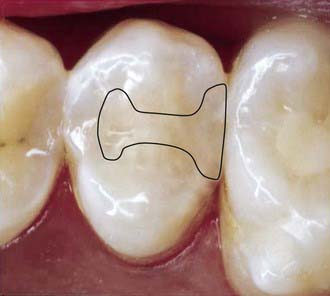
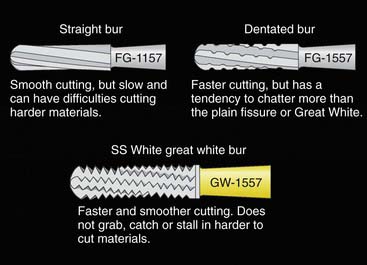
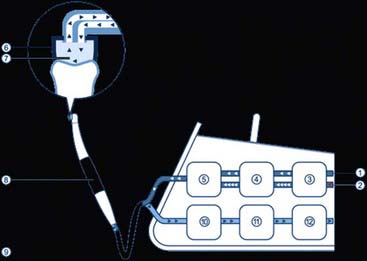
The less destruction of tooth structure, the more conservative the preparation. The more of the original tooth structure that can be maintained, is generally more esthetic. In dealing with a carious occlusal pit and fissure lesion that extends into dentin, management with a minimally invasive approach is preferable—for example, using the SS White fissurotomy burs (SS White Burs, Inc., Lakewood, New Jersey) (Figure 26-1, A) and exposing the dentin, plus subsequent treatment with ozonation of tooth surface and rinsing with ozonated water (Figure 26-1, B). The disinfection of remaining carious dentin is possible as long as the lesion is relatively superficial. An acid-etching technique (Etch-Rite, Pulpdent Corporation, Watertown, Massachusetts) is then used on the enamel (Figure 26-1, C), followed by a use of single-bottle seventh-generation system (Bondforce, Tokuyama Dental America, Inc., Encinita, California) for bonding to enamel and dentin (Figure 26-1, D). After light polymerization (Figure 26-1, E), an appropriate flowable composite resin (BEAUTIFIL Flow Plus, Shofu Dental Corp., San Marcos, California) can be inserted into the cavity (Figure 26-1, F). This is a very minimally invasive approach that produces end results that are esthetically pleasing for the patient (Figure 26-1, G).
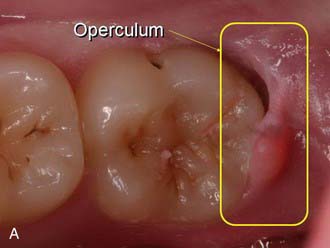
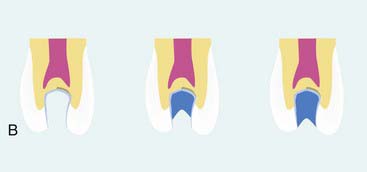
Patients who are esthetically oriented are generally more up-to-date with modern health concepts and philosophies. Dentistry has moved away from the destructive template approach that involved cutting prescribed shapes into the teeth (Figure 26-2). Modern dental practice is much more focused on a disease-oriented approach, in which the diseased tissues are removed and only those modifications that are absolutely necessary to improve the longevity of the restoration are made to the cavity site (Figure 26-3).
Brief History of Clinical Development of Minimally Invasive Dental Procedures and Technology
The earliest perhaps inadvertent attempts at esthetic dentistry or minimally invasive dentistry were made by Michael G. Buonocore in the 1950s (see Figure 8-16). He was the first to etch teeth and to begin the process of bonding to tooth structure, which is inherently more conservative of teeth than preparing shapes that physically retain amalgam. As this approach progressed from enamel etching to the inclusion of dentin etching/conditioning in subsequent years, it became more widely used, so that by the turn of the twenty-first century over 50% of North American posterior restorations were performed with adhesive procedures. Subsequently the single-bottle, seventh-generation adhesives were developed. Other innovative technologies helped to ensure that the surface to be restored was relatively free of bacteria that cause decay, or at least less inclusive of those bacteria (Figure 26-4).
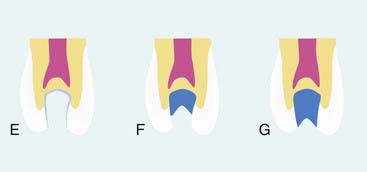
The philosophy is now even more conservative. The infected dentin is managed with ozone and photoactivated disinfection (PAD). This allows the operator to dramatically reduce the number of microorganisms remaining in the retained dentin, which can then be infiltrated with adhesives that bond to this surface. This process is most conservative with direct composite restorations. Ozone can penetrate to a somewhat deeper sub-surface level than PAD. Ozone is available in a gaseous form, such as that provided by the HealOzone system (Curozone GmbH, Wiesbaden, Germany) (Figure 26-5) in action and in aqueous form with ozonated water.
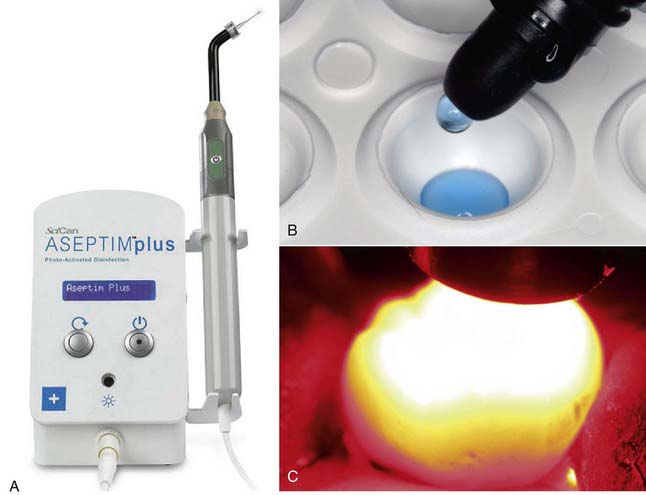
PAD is available commercially as well. The most common system used is Aseptim Plus (SciCan, Ltd., Toronto, Canada) (Figure 26-6, A). A dye that attaches to microorganisms (Figure 26-6, B) is placed on the prepared tooth surface then is irradiated with a light-emitting diode (LED) light to effectively kill the microorganisms near the surface (Figure 26-6, C).
Relating Function and Esthetics
Maintaining the natural tooth structure assists in both function and esthetics. For example, if an operator is removing caries from a mesial-occlusal-distal (MOD) cavity in the upper first premolar, and if the base of the retained buccal cusp is supported by more conserved tissue, clearly that buccal cusp has greater strength than that allowed by the traditional invasive approach of cavity preparation, which undermines and weakens the remaining cusp (Figure 26-7). Natural tooth structure is better than the best restorative materials available and supersedes any synthetic material the dentist can place. Generally, if the dentist can maintain the natural occlusion, the natural form and shape of the tooth, and the functional outline of the dentition and soft tissues, the health of the patient’s oral environment will be better and more easily maintained over a longer term.
Clinical Considerations
Indications
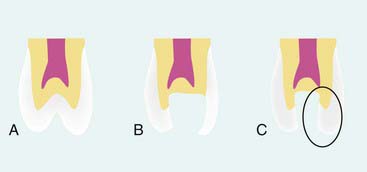
The indications for minimally invasive dentistry include every preparation and intervention that an operator carries out. Minimally invasive techniques are not solely applicable to pits and fissures but also deal with overall health and patient management. Even deep carious lesions can be managed to avoid traumatic exposure of the pulp or even potential further damage to the pulp through additional heating, desiccation, or trauma associated with operative procedures in close proximity to the pulp (Figure 26-8).
Contraindications
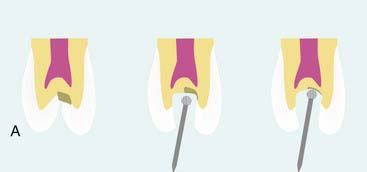
Minimally invasive dentistry is both a clinical approach and a philosophical one. In practical terms, it is a clinical approach because it is something that every dentist aims to achieve for every preparation for each patient. However, the philosophical approach of non–minimally invasive dentistry has been predominant for over a century within the dental profession. It predated the modern pharmaceutical approach to managing infected tissues. In the past, a number of studies have shown that any infection remaining in the tissues could progress, thereby leading to ongoing problems beneath restorations (Figure 26-9). Caries may progress, with all the attending implications. Of the pharmaceutical approaches to management, the two most notable are ozone (gas or ozonated water) and PAD. These approaches destroy or reduce the pathogenicity of the cariogenic flora remaining beneath cavity preparations. This allows a much more minimally invasive approach. This treatment modality is not limited to the management of caries or cavity preparations; it can be used in endodontics, periodontal therapy, and other areas.
Material and Assessing Options
Clinical dentistry can be a rather difficult occupation. The oral cavity is not a treatment-friendly space; it is small, has restricted access with numerous interfering oral structures, and is generally quite dark. Seeing minute details (during diagnosis or treatment) and visualizing procedures in progress can be both difficult and stressful. The improperly positioned patient’s head can cause significant physical discomfort to the practitioner seeking better visual access and may in time cause the dentist physical damage that may impede the continued practice of dentistry (Figure 26-10).
Magnification
Magnification provides the means to alleviate many of these problems and concerns and allows the dentist to practice more comfortably while ensuring that dental procedures can be delivered at the most exacting level (Figure 26-11).

FIGURE 26-11 Practitioner wearing magnification loupes.
(Courtesy Orascoptic, Middleton, Wisconsin.)
Visualization
Improved visualization of minute yet significant dental detail simplifies diagnosis and enhances clinical treatment. The dentist using magnifying loupes can examine both hard and soft tissue surfaces in more exacting detail, thus often diagnosing problems at an earlier stage than previously possible. Earlier diagnosis benefits the patient through more conservative, less invasive treatment (Figure 26-12).
Fortuitously, magnification loupes force the operator into a more ergonomic posture, reducing back and neck strains (Figure 26-13). A dentist who is using properly fitted magnification loupes is required to view the oral cavity and to operate from a more ergonomic and healthier sitting position. There is less stress on the back and neck muscles, reducing strain and contributing to more comfortable and productive working sessions. Magnification is responsible for reducing eyestrain by providing a clear and magnified view of the working area. Decreased eye fatigue contributes to a more satisfying clinical practice, particularly toward the end of a working day or a long working week. In addition, the improved clinical visualization allows more precise and less invasive treatment.
Esthetic and cosmetic procedures call for invisible margins and tooth-restorative interface transitions. These technique-sensitive, yet critical, features are far easier and less demanding to develop when the visual working field is enhanced to twice normal (or greater) size. If the margin seems to “disappear” when magnified, then it will certainly not be visible to the naked eye. The fine internal and external colorations and characterizations that are required for “invisible” margins are virtually impossible to achieve without appropriate magnification (Figure 26-14).
Illumination
The science and art of illuminating the operative site have advanced rapidly in recent years. Dentists, like medical surgeons, have found that maximizing visual acuity at the work site not only is important, it is essential (Figure 26-15). Suitable lighting provides much-improved diagnostics, greatly enhanced treatment opportunities, and better treatment outcomes. Vision and visibility in the oral cavity are always major concerns. Hands, instruments, or even a slight movement of the patient’s head can often obstruct the overhead dental light. Fiberoptic light handpieces have been the standard of care for several decades, and most dentists will not consider high-speed tooth preparation without targeted illumination of the operative site (Figure 26-16). Although in-handpiece lights are effective in illuminating the immediate working area, often a larger sphere of visibility is needed (Figure 26-17). In addition, as dental professionals get older, their eyes require more light to see and work effectively. Increasingly they have begun to use illuminating headlamps. Earlier lighting models were heavy, bulky, wired (to the battery), and cumbersome. The innovative and very convenient solutions to illumination problems inside the oral cavity consist of LED bulbs that provide 500 foot-candles of light intensity or more. Best of all, the headlight’s weight on a standard clip is less than 1 oz. Headlights are also effective clinical treatment adjuncts for hygienists as well as others on the dental team.
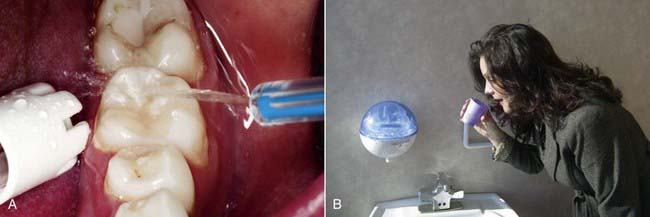
Isolation
There are typically three major problems when working in the mouth: (1) the lack of visibility of the teeth or soft tissues, (2) the physical interference of the tongue and cheeks in the work areas, and (3) the presence of copious amounts of saliva that tends to flood surfaces just when they need to be dry. In fact, most of the benefits of four-handed dentistry involve improved isolation and moisture control in the working area. The Isolite system (Isolite Systems, Santa Barbara, California) (Figure 26-18, A) isolates the working field by keeping away the tongue and cheeks. It is attached to the high-volume suction port and aspirates both excess saliva and coolant water from the handpiece. It also provides bright, shadowless illumination inside the mouth through the light distribution system in the Isolite mouthpiece (Figure 26-18, B). The light source is external, and the brightness can be adjusted as per the needs of the operator. The single-use mouthpiece is readily inserted into the patient’s mouth, and patients find the mouthpiece very comfortable as resting the teeth on the bite block makes it easier to keep the mouth open for extended periods during procedures. The illumination is delivered into the mouth using an LED light source; there is no electrical current or any danger of shock in the mouth. The continuous aspiration of both the buccal and lingual sulci keeps the field dry and the working area clean and clearly visible. The Isolite mouthpiece is flexible and acts as a single-unit replacement for numerous isolation, illumination, and aspiration devices.
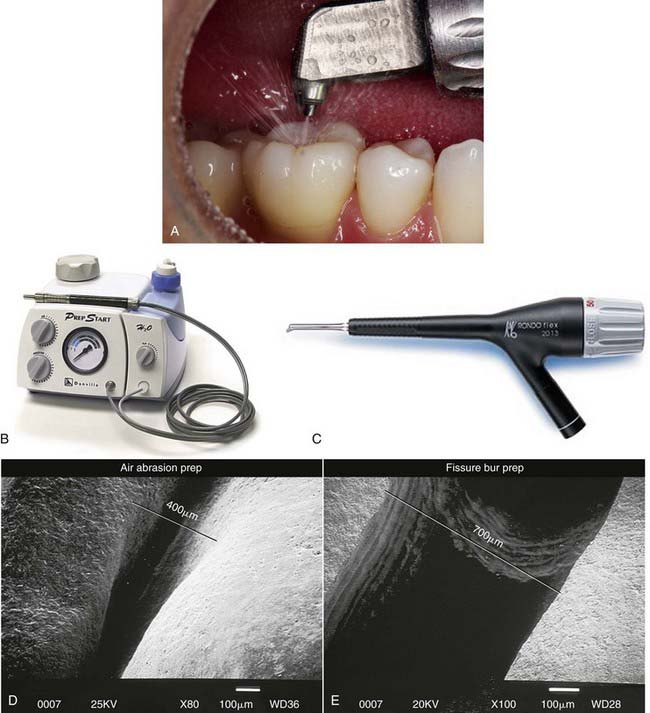
Preparation
Clearly the tools that are used to prepare the cavity are very important. Air abrasion must be well directed and aimed into the cavity with appropriate high-aspiration suction so as not to produce excessive debris around the rim of the preparation (Figure 26-19, A). The PrepStart H2O (Danville Materials, San Ramon, California) (Figure 26-19, B) and the RONDOflex (KaVo Dental, Charlotte, North Carolina) (Figure 26-19, C) are the two highest-ranked air abrasion systems for use in cavity preparations, particularly in pits and fissures (Figure 26-19, D and E).
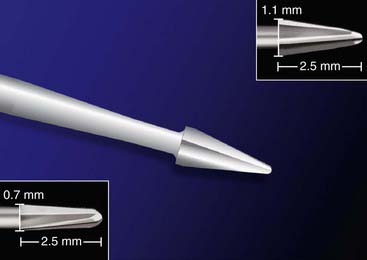
The SS White Fissurotomy bur (Figure 26-20) is a novel approach to ultraconservative dental treatment. The shape and size of the bur are designed specifically for the purpose of treating small, incipient, and pit and fissure lesions. The head length of the bur is 2.5 mm, the average thickness of occlusal enamel, allowing the dentist to limit the bur tip to cut to just below the dentino-enamel junction (DEJ) and not further into the dentin (conservation). The tapered shape of the bur (visualization) allows the cutting tip to encounter very few dentinal tubules (patient comfort) at any given time and has been designed to minimize heat buildup and vibration. Because the cutting of the Fissurotomy bur is restricted largely to enamel, patient discomfort is minimized and the need for local anesthetic is eliminated in most cases. The Fissurotomy bur is far less invasive than similar length carbide and diamond burs. Traditional cutting burs remove far more enamel at any depth of cut and are designed to access caries that has progressed well beyond the DEJ, whereas the Fissurotomy bur has been anatomically designed to enlarge the fissure and eliminate small caries without removing excessive healthy enamel or dentin.
The SS White Great White bur (Figure 26-21) is an excellent instrument for generating conservative preparations, particularly in posterior teeth. Its highly dentated surfaces quickly and effectively cut tooth structures, amalgam and composite resin, and restorative metals. Its geometric configuration is highly suitable for developing ideal cavity preparations for class I and II posterior composite resins. The Great White bur does not grab, catch, stall, or break in harder-to-cut materials such as amalgam, composite, and semi-precious and non-precious castings.
The HealOzone system (Curozone, Wiesbaden, Germany) (Figure 26-22) produces ozone that safely kills cavity-causing bacteria in and on the tooth (Figure 26-23). To prevent potential lung inhalation, it is important to follow manufacturer directions. Ozone treatment (as seen in the HealOzone system) is highly effective in managing superficial infected dentin.
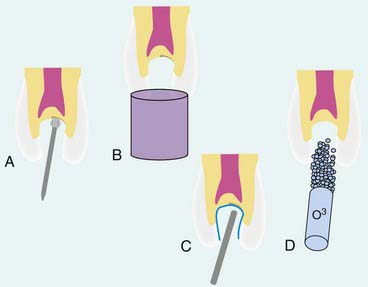
Single Surface Occlusal Cavity
As previously documented in Figure 26-9, A, the majority of the decay is removed. Often, undetectable surface bacteria remain that can cause further decay after the restorative process (Figure 26-24, A). Ozone gas can be used to kill bacteria in the surface dentin layers (Figure 26-24, B). Alternatively, PAD can also be used to destroy the remaining bacteria (Figure 26-24, C). After either of these treatments or independently, ozonated water can be used in rinsing the cavity preparation to provide a bactericidal effect (Figure 26-24, D). Then a seventh-generation adhesive is applied to the prepared surfaces, air dried, and polymerized (Figure 26-24, E). The composite restorative material is placed into the cavity in small increments (up to 2 mm) and polymerized (Figure 26-24, F). The composite material is built in increments to the occlusal surface, polymerized at every step, and then finished to full occlusal contour and esthetics (Figure 26-24, G).
The Aseptim Plus unit (see Figure 26-6, A) is a PAD device that infiltrates the cell wall using tolonium chloride dye. PAD is discussed thoroughly in Section D of this chapter.
Innovative Elements
Air Abrasion
With respect to cavity preparation, innovations involve the use of water with the air abrasive stream, which reduces the dust that would otherwise spread around the mouth and the operatory (Figure 26-25). The traditional handpiece methods used by dentists to prepare teeth for restoration, combined with their associated sounds and sensations, can have a tremendous impact on the image of the practice, its marketing potential, and treatment acceptance by patients. Most patients dislike the noise and the vibration of the drill during the cavity preparation, often commenting on the need for alternative treatment options. Drill-less techniques have been used in dentistry for more than half a century. In the last two decades, novel abrasion technologies and improved adhesive restorative materials have made these options practical and effective.
Ozone
With the HealOzone system, ozone is delivered inside a cup directly into the lesion being treated (Figure 26-26). If the cup loses its seal, the cup simply sucks air into itself and ceases to deliver ozone. Radical ozone ions can be quite damaging to the lungs and should not be inhaled in significant dose. The HealOzone system has been proven in many studies to be absolutely safe to use. Even when it is inadvertently misused, there is no danger of any damage occurring to the lungs of the patient, the operator, or assistants because of the safety mechanisms that have been built into the technology (Figure 26-27).
Water Ozone Systems
Ozonated water systems are also very safe. Any ozone not delivered into the water bottle is converted into oxygen by the safety mechanisms, which is then blown into the dental operatory. The ozonated water is produced in total safety. The ozonated water can be used directly in irrigating syringes, ultrasonic scalers, cavity preparation rinses, root canal irrigation, or mouth rinsing for patients before, during, and after treatment to promote healing (Figure 26-28).
Innovative Elements of Fissurotomy
The SS White Fissurotomy bur (Figure 26-29) uses shapes as narrow as 0.7 mm and a cutting side as small as 2.5 mm long. The 2.5 mm relates to the average depth of the occlusal enamel. The operator can control the preparation with the Fissurotomy bur to ensure that it continues to cut enamel only, never entering the dentin. This eliminates the likelihood of patient discomfort. The conical shape of the Fissurotomy bur permits comprehensive visual access to any remaining carious material.
Treatment Considerations
Operative Considerations
Restorative Dentistry
The electrical caries monitor (ECM) is used to objectively quantify the severity of the root caries index (Figure 26-30). Previously, primary root lesions were classified by color, texture, hardness, cavitation, size, and severity. The ECM can be used to determine the severity of primary carious lesions because it is a less invasive but equally accurate way to detect carious lesions when compared with tactile methods.
Surface Finishing and Polishing
For finishing, the least invasive and the most rapid procedure is generally the best. The SS White Jazz Supreme polishing system (Figure 26-31) is a one step, one instrument polishing system that provides a highly successful clinical approach. Most polishing systems offer a series of progressively smoother polishing instruments, from coarse to medium to fine, but with the Jazz System a single instrument is used throughout the polishing process. The progressive abrasiveness depends on the pressure that the operator places on the instrument during the polishing of the tooth surface. With greater pressure, the effect is more abrasive, actually removing or smoothing the surfaces. As less pressure is applied, the bur’s action tends to buff and produce a final luster. Within seconds an acceptable anatomy can be molded, shaped, and polished to a high-gloss, high-luster surface that will last for many years.
Agrillo A, Sassano P, Rinna C, et al. Ozone therapy in extractive surgery on patients treated with bisphosphonates. J Craniofac Surg. 2007;18:1068-1070.
Agrillo A, Ungari C, Filiaci F, et al. Ozone therapy in the treatment of avascular bisphosphonate-related jaw osteonecrosis. J Craniofac Surg. 2007;18:1071-1075.
Al Shamsi AH, Cunningham JL, Lamey PJ, Lynch E. The effects of ozone gas application on shear bond strength of orthodontic brackets to enamel. Am J Dent. 2008;21:35-38.
Arita M, Nagayoshi M, Fukuizumi T, et al. Microbicidal efficacy of ozonated water against Candida albicans adhering to acrylic denture plates. Oral Microbiol Immunol. 2005;20:206-210.
Azarpazhooh A, Limeback H. The application of ozone in dentistry: a systematic review of literature. J Dent. 2008;36:104-116.
Barandun A, Boitel RK. Thirteen years of experience with the Barandun irrigator and ozone treatment in endodontics. Oral Surg Oral Med Oral Pathol. 1962;15:986-995.
Baysan A: Management of primary root caries using ozone therapies, 2002.
Baysan A, Beighton D. Assessment of the ozone-mediated killing of bacteria in infected dentine associated with noncavitated occlusal carious lesions. Caries Res. 2007;41:337-341.
Baysan A, Lynch E. Clinical reversal of root caries using ozone: 6-month results. Am J Dent. 2007;20:203-208.
Baysan A, Lynch E. Effect of ozone on the oral microbiota and clinical severity of primary root caries. Am J Dent. 2004;17:56-60.
Baysan A, Lynch E. The use of ozone in dentistry and medicine. Prim Dent Care. 2005;12:47-52.
Baysan A, Lynch E. The use of ozone in dentistry and medicine. Part 2. Ozone and root caries. Prim Dent Care. 2006;13:37-41.
Baysan A, Prinz JF, Lynch E. Clinical criteria used to detect primary root caries with electrical and mechanical measurements in vitro. Am J Dent. 2004;17:94-98.
Baysan A, Whiley R, Lynch E. Antimicrobial effects of a novel ozone generating device on micro-organisms associated with primary root carious lesions in vitro. Caries Res. 2000;34:498-501.
Beighton D, Lynch E. Comparison of selected microflora of plaque and underlying carious dentine associated with primary root caries lesions. Caries Res. 1995;29:154-158.
Beighton D, Lynch E. Relationships between yeasts and primary root-caries lesions. Gerodontology. 1993;10:105-108.
Beighton D, Lynch E, Heath MR. A microbiological study of primary root-caries lesions with different treatment needs. J Dent Res. 1993;72:623-629.
Bezirtzoglou E, Cretoiu SM, Moldoveanu M, et al. A quantitative approach to the effectiveness of ozone against microbiota organisms colonizing toothbrushes. J Dent. 2008;36(8):600-605.
Bezrukova IV, Petrukhina NB, Voinov PA. Experience in medical ozone use for root canal treatment. Stomatologiia (Mosk). 2005;84:20-22.
Bocci V. Oxygen-ozone therapy: a critical evaluation. The Netherlands: Kluwer Academic Publishers; 2002.
Bocci V. The case for oxygen-ozone therapy. Br J Biomed Sci. 2007;64(1):44-49.
Bocci VA. Scientific and medical aspects of ozone therapy. State of the art. Arch Med Res. 2006;37:425-435.
Brailsford SR, Lynch E, Beighton D. The isolation of Actinomyces naeslundii from sound root surfaces and root carious lesions. Caries Res. 1998;32:100-106.
Cardoso MG, de Oliveira LD, Koga-Ito CY, Jorge AO. Effectiveness of ozonated water on Candida albicans, Enterococcus faecalis, and endotoxins in root canals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:85-91.
Celiberti P, Pazera P, Lussi A. The impact of ozone treatment on enamel physical properties. Am J Dent. 2006;19:67-72.
Chahverdiani B, Thadj-Bakhche A. Ozone treatment in root canal therapy. Introduction and general discussion. Acta Med Iran. 1976;19:192-200.
Collier FI, Heath MR, Lynch E, Beighton D. Assessment of the clinical status of primary root carious lesions using an enzymic assay. Caries Res. 1993;27:60-64.
Dahnhardt JE, Jaeggi T, Lussi A. Treating open carious lesions in anxious children with ozone. A prospective controlled clinical study. Am J Dent. 2006;19:267-270.
de Monte A, van der Zee H, Bocci V. Major ozonated autohemotherapy in chronic limb ischemia with ulcerations. J Altern Complement Med. 2005;11:363-367.
Deltour G, Vincent J, Lartigau GL. Lethal effect of ozone on certain aerobic bacteria strains in a model of the dental pulp chamber. Rev Odontostomatol Midi Fr. 1970;28:278-284.
Ebensberger U, Pohl Y, Filippi A. PCNA-expression of cementoblasts and fibroblasts on the root surface after extraoral rinsing for decontamination. Dent Traumatol. 2002;18:262-266.
Estrela C, Estrela CR, Decurcio Dde A, et al. Antimicrobial potential of ozone in an ultrasonic cleaning system against Staphylococcus aureus. Braz Dent J. 2006;17:134-138.
Fisch EA. Therapy of periodontal inflammation. Minerva Stomatol. 1955;4:8-10.
Gracer RI, Bocci V. Can the combination of localized “proliferative therapy” with “minor ozonated autohemotherapy” restore the natural healing process? Med Hypotheses. 2005;65:752-759.
Grootveld M, Silwood CJ, Lynch E. High resolution 1H NMR investigations of the oxidative consumption of salivary biomolecules by ozone: relevance to the therapeutic applications of this agent in clinical dentistry. Biofactors. 2006;27:5-18.
Holmes J. Clinical reversal of root caries using ozone, double-blind, randomised, controlled 18-month trial. Gerodontology. 2003;20:106-114.
Huth KC, Jakob FM, Saugel B, et al. Effect of ozone on oral cells compared with established antimicrobials. Eur J Oral Sci. 2006;114:435-440.
Huth KC, Paschos E, Brand K, Hickel R. Effect of ozone on non-cavitated fissure carious lesions in permanent molars—a controlled prospective clinical study. Am J Dent. 2005;18:223-228.
Huth KC, Saugel B, Jakob FM, et al. Effect of aqueous ozone on the NF-kappaB system. J Dent Res. 2007;86:451-456.
Johansson E, Andersson-Wenckert I, Hagenbjörk-Gustafsson A, Van Dijken JW. Ozone air levels adjacent to a dental ozone gas delivery system. Acta Odontol Scand. 2007;65:324-330.
Kandic D. Use of ozone in conservative dentistry. Stomatol Glas Srb. 1968;15:159-165.
Lynch E. Evidenced based caries reversal using ozone. J Esthet Restor Dent. 2008;20:218-222.
Lynch E. Evidenced based efficacy of ozone for root canal irrigation. J Esthet Restor Dent. 2008;20(5):287-293.
Lynch E, Beighton D. A comparison of primary root caries lesions classified according to colour. Caries Res. 1994;28:233-239.
Lynch E, Beighton D. Relationships between mutans streptococci and perceived treatment need of primary rootcaries lesions. Gerodontology. 1993;10:98-104.
Martínez-Sánchez G, Al-Dalain SM, Menéndez S, et al. Therapeutic efficacy of ozone in patients with diabetic foot. Eur J Pharmacol. 2005;31:151-161.
Miller BJ, Hodson N. Assessment of the safety of two ozone delivery devices. J Dent. 2007;35:195-200.
Murakami H, Mizuguchi M, Hattori M, et al. Effect of denture cleaner using ozone against methicillin-resistant Staphylococcus aureus and E. coli T1 phage. Dent Mater J. 2002;21:53-60.
Nagayoshi M, Fukuizumi T, Kitamura C, et al. Efficacy of ozone on survival and permeability of oral microorganisms. Oral Microbiol Immunol. 2004;19:240-246.
Nagayoshi M, Kitamura C, Fukuizumi T, et al. Antimicrobial effect of ozonated water on bacteria invading dentinal tubules. J Endod. 2004;30:778-781.
Oizumi M, Suzuki T, Uchida M, et al. In vitro testing of a denture cleaning method using ozone. J Med Dent Sci. 1998;45:135-139.
Overdiek HF, Honrath L. Ozone in the treatment of root canal gangrene. Zahnarztl Welt Zahnarztl Reform Zwr. 1951;6:373-376.
Petrucci MT, Gallucci C, Agrillo A, et al. Role of ozone therapy in the treatment of osteonecrosis of the jaws in multiple myeloma patients. Haematologica. 2007;92:1289-1290.
Polydorou O, Pelz K, Hahn P. Antibacterial effect of an ozone device and its comparison with two dentin-bonding systems. Eur J Oral Sci. 2006;114:349-353.
Rickard GD, Richardson R, Johnson T, et al. Ozone therapy for the treatment of dental caries. Cochrane Database Syst Rev (3):CD004153, 2004.
Sandhaus S. Ozone therapy in odontostomatology, especially in treatments of infected root canals. Rev Belge Med Dent. 1965;20:633-646.
Schmidlin PR, Zimmermann J, Bindl A. Effect of ozone on enamel and dentin bond strength. J Adhes Dent. 2005;7:29-32.
Siqueira JFJr, Rôças IN, Cardoso CC, et al. Antibacterial effects of a new medicament—the ozonized oil compared to calcium hydroxide pastes. Rev Bras Odontol. 2000;57:252-256.
Stübinger S, Sader R, Filippi A. The use of ozone in dentistry and maxillofacial surgery: a review. Quintessence Int. 2006;37:353-359.
Valacchi G, Bocci V. Studies on the biological effects of ozone: 10. Release of factors from ozonated human platelets. Mediators Inflamm. 1999;8:205-209.
Valacchi G, Fortino V, Bocci V. The dual action of ozone on the skin. Br J Dermatol. 2005;153:1096-1100.
Walker JT, Bradshaw DJ, Fulford MR, Marsh PD. Microbiological evaluation of a range of disinfectant products to control mixed-species biofilm contamination in a laboratory model of a dental unit water system. Appl Environ Microbiol. 2003;69:3327-3332.
Zbinden M. General report on the use of chlorine and ozone in root canal therapy. SSO Schweiz Monatsschr Zahnheilkd. 1951;61:332-336.
Section B Diode Lasers: The Soft Tissue Handpiece
Diode Lasers: The Science in Brief
The word laser is derived from the acronym for light amplification by stimulated emission of radiation. Lasers are commonly named for the substance that is stimulated to produce the coherent light beam. In the diode laser, this substance is a semiconductor (a class of materials that are the foundation for modern electronic devices, including computers, telephones, and radios). This innovative technology has produced a laser that is compact and far lower in cost than earlier versions. Much of the research has focused on the 810-nm diode laser. Energy of this wavelength is ideally suited for soft tissue procedures because it is highly absorbed by hemoglobin and melanin. This gives the diode laser the ability to precisely cut, coagulate, ablate, or vaporize the target soft tissue.1
Treatment with the 810-nm diode laser (Figure 26-32, Picasso diode laser, AMD Lasers, Indianapolis, Indiana) has been shown to have a significant long-term bactericidal effect in periodontal pockets. A. actinomycetemcomitans, an invasive pathogen associated with the development of periodontal disease and generally quite difficult to eliminate, responds well to laser treatment.2,3 Scaling and root planing outcomes are enhanced when diode laser therapy is added to the dental armamentarium. The patient is typically more comfortable during and after treatment, and gingival healing is faster and more stable.4,5
Diode Laser: Why do I need this technology?
The 810-nm diode laser is specifically a soft tissue laser. This wavelength is ideally suited for soft tissue procedures because hemoglobin and melanin, both prevalent in dental soft tissues, are excellent absorbers. This provides the diode laser with broad clinical utility: it cuts precisely, coagulates, ablates, or vaporizes the target tissue with less trauma, improved postoperative healing, and faster recovery times.6–8 Given the incredible ease of use and its versatility in treating soft tissue, the diode laser becomes the “soft tissue handpiece” in the dentist’s armamentarium. The dentist can use the diode laser soft tissue handpiece to remove, refine, and adjust soft tissues in the same way that the traditional dental handpiece is used on enamel and dentin. This extends the scope of practice of the general dentist to include many soft tissue procedures.
The procedures discussed in the following sections are easy entry points for the new laser user.
Gingivectomy, Hemostasis, and Gingival Troughing for Impressions
The diode laser (Picasso) makes restorative dentistry “a breeze.” Any gingival tissue that covers a tooth during preparation can be easily removed, as hemostasis is simultaneously achieved (Figure 26-33). The restoration is no longer compromised because of poor gingival conditions. There is no more battling with unruly soft tissue and blood. Excess gingival tissue can be readily managed (Figure 26-34) for improved restorative access for class V preparation (ezLase, Biolase Technology, Irvine, California).
Gingival troughing before an impression is taken (see Figures 26-33, E and 26-34, A [Picasso]) ensures an accurate impression (particularly at the all-important margins) and an improved restorative outcome. Packing cord is no longer necessary.
Operculectomy, Excision and/or Re-Contouring of Gingival Hyperplasia, and Frenectomy
Operculectomy, excision and/or re-contouring of gingival hyperplasia, and frenectomy are not commonly offered or performed by the general dentist. These procedures are examples of the expanded range of services readily added to the general practice. The dentist becomes more proactive in dealing with hyperplastic tissues that can increase risk of caries and periodontal disease (Figure 26-35).
A frenectomy is now a simple and straightforward procedure (Figure 26-36 [ezLase]).
Laser-Assisted Periodontal Treatment
The use of the diode laser in conjunction with routine scaling and root planing is more effective than scaling and root planing alone. It enhances the speed and extent of the patient’s gingival healing and postoperative comfort.4,5 This is accomplished through laser bacterial reduction (Picasso), débridement, and biostimulation (Figure 26-37).
A. actinomycetemcomitans, which has been implicated in aggressive periodontitis, may also be implicated in systemic disease. It has been found in atherosclerotic plaque,9 and recent data have suggested that it may be related to coronary heart disease.10 The diode laser is effective in decreasing A. actinomycetemcomitans2,4 and thereby indirectly improving patients’ heart health.
Laser Education
Most diode laser manufacturers provide some education to get the new user started quickly and effectively. The most comprehensive online diode laser introductory course with certification (including the science and safety and clinical procedures) can be found at the International Center for Laser Education, www.dentallaseredu.com (877-522-6863). This course provides everything necessary to get started with soft tissue diode laser therapy. Advanced courses are available for more complex procedures.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses























 S. Irjicianu, A. Joan, E. Ozone in endodontic therapy. Stomatologia (Bucur), 1970;17:303-307.
S. Irjicianu, A. Joan, E. Ozone in endodontic therapy. Stomatologia (Bucur), 1970;17:303-307.