Chapter 29 Ortho-Esthetics
Relating Function and Esthetics
From an orthopedic (bone) standpoint, the seven keys to TMJ health are as follows:
1. The maxilla must be the proper width.
2. The maxilla must be positioned correctly anteroposteriorly.
3. A proper relationship must be present between the maxilla and the mandible.
4. The maxillary incisors must be properly inclined.
5. There must be no unilateral or bilateral crossbite.
6. Lower posterior teeth must be upright over the basal bone.
Clinical Considerations
Proper Maxillary Width
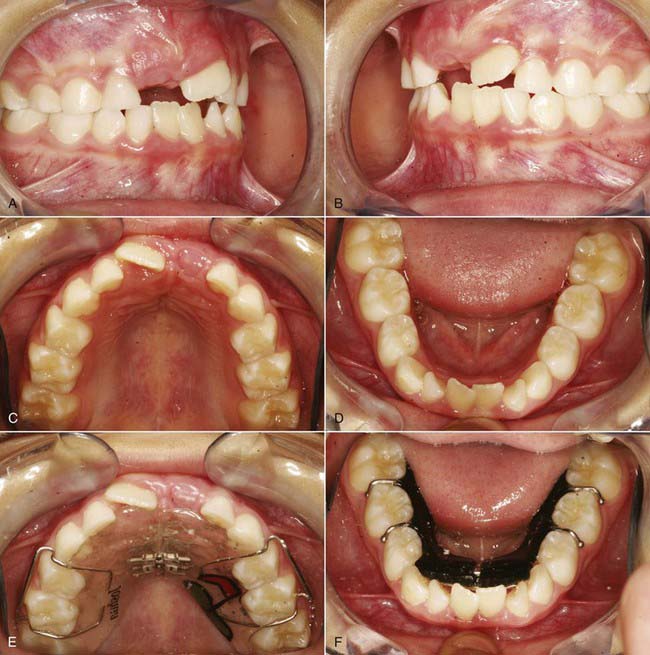
In developing the maxilla to its correct width using functional appliances, the simplest apparatus is the Schwarz appliance, which consists of two pieces of acrylic with a midline screw and four retaining clasps, i.e. Adam’s clasps, on both sides. These appliances are extremely comfortable and can be used to treat patients as young as age 5 years. The midline screw of these appliances is activated twice a week, which equals 0.5 mm per week or 2 mm per month. They are well tolerated by children and teenagers alike, as there is no discomfort involved. The appliance should be worn at all times except when cleaning or for active sports. If a 6 mm expansion is required, then the appliance is activated for 3 months and held for 6 months to prevent a relapse. Statistics show that the results are extremely stable in patients who are nasal breathers and have no airway obstruction (Figure 29-1).
1. Retractive technique. This involves treatment of the permanent dentition and recommends extraction of teeth, usually the bicuspids, to eliminate crowding. Proponents believe the teeth are too large for the arches so permanent teeth are extracted to solve the crowding problem. The consequence of this can be a narrow smile and a posteriorly displaced condyle with resultant internal derangement (temporomandibular dysfunction [TMD]).
2. Functional technique. This involves treatment of the mixed or permanent dentition using functional appliances to expand and lengthen the arches so all the permanent teeth fit. Proponents believe the problem results from the arch being too small for normal-sized teeth, so the arch is expanded to a normal width. Patients treated with a functional philosophy routinely have normal, symptom-free TMJs.
Maxilla Positioned Correctly Antero-posteriorly
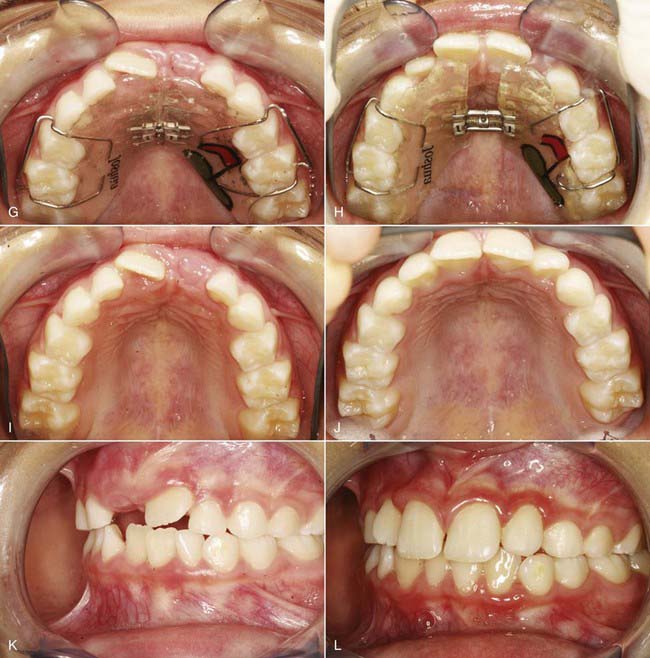
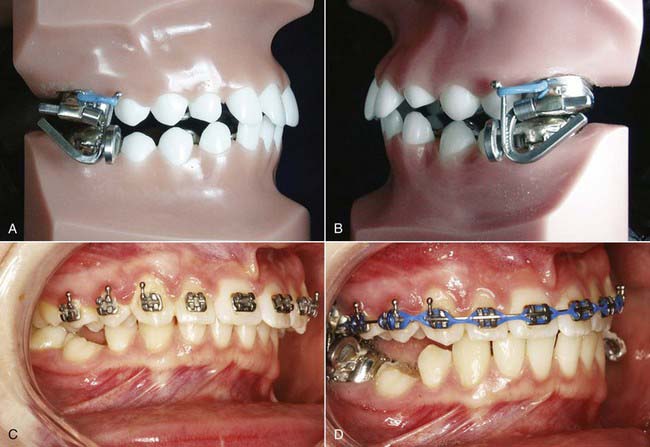
One of the most popular fixed functional appliances for children is the Tandem Appliance, which effectively advances the entire maxilla. Patients with TMDs caused by anteriorly displaced disks and posteriorly displaced condyles must have the maxilla properly positioned anteriorly first. Once the maxilla is moved forward with a functional appliance, such as the Tandem Appliance, and an overjet has been created, the mandible can be advanced, moving the condyle down and forward. Hopefully, this will recapture the anteriorly displaced disk and eliminate the signs and symptoms of TMD (Figure 29-2).
Proper Relationship between Maxilla and Mandible
Tomographic Radiographs of the Temporomandibular Joint
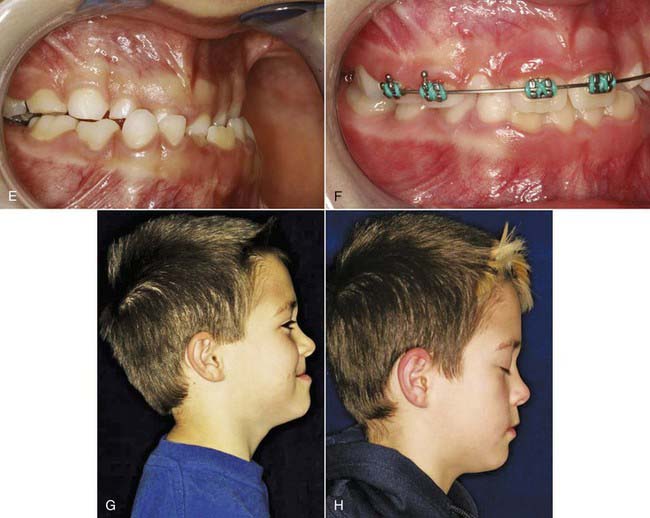
The tomogram shows the position of the condyle in the fossa when the patient is occluding in centric occlusion. In a recent article in the Journal of the American Dental Association, the correct position of the condyle in the fossa was identified as downward and forward, not rearmost and uppermost, as reported in many old textbooks. The ideal position of the condyle in the fossa in centric occlusion is to have a larger posterior joint space than an anterior joint space. The posterior joint space should be at least 4 mm to allow room for the nerves and blood vessels in the bilaminar zone plus a 2 mm superior joint space to allow room for the posterior ligament and a 2 mm anterior joint space to allow room for the disk (Figure 29-3).
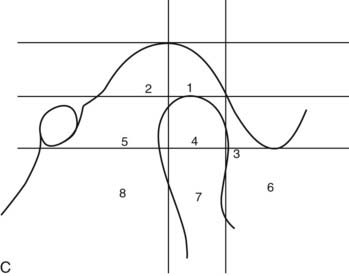
Joint Vibration Analysis
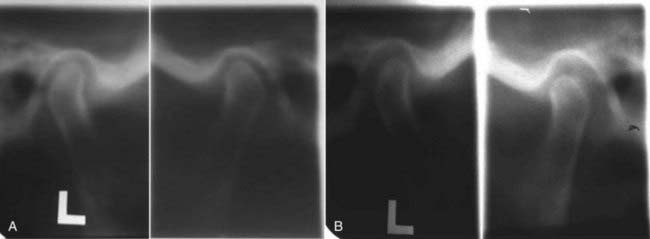
The joint vibration analysis (JVA) device measures vibrations within the joint. Each of the five stages of internal derangements has a distinct vibration that indicates to the clinician just how serious the problem is before treatment. A normal healthy TMJ makes no noise, causes no pain, and makes no vibrations. The JVA diagnostic device can also be helpful during treatment with anterior repositioning splints (adults) or with the Twin Block appliance or Mandibular Anterior Repositioning Appliance (MARA) in children or adults to confirm that the disk has been recaptured (Figure 29-4).
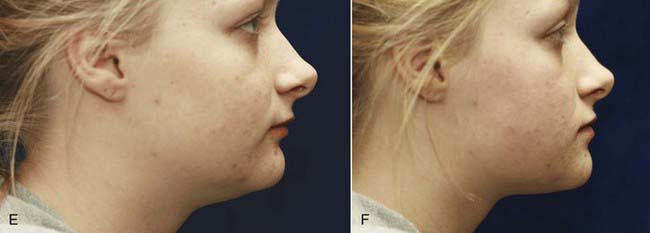
The treatment of choice for a patient with a retrognathic profile, in order to improve the appearance, is to reposition the lower jaw forward using a functional appliance such as a Twin Block (removable appliance) or MARA (fixed functional appliance). The literature is clear that if the disk can be recaptured with the functional appliance that moves the mandible forward, then most patients have a significant reduction in the signs and symptoms of TMD. The treatment objective for these patients is to improve not only the facial esthetics but also the TMJ health (Figure 29-5).
Proper Inclination of Maxillary Incisors
Dentists who fabricate crowns and bridges for patients with Class II, division 2 malocclusion must be extremely careful to diagnose and treat the TMD that exists in most cases before treatment. When the maxillary central incisors are lingually inclined, this frequently traps the mandible and causes the condyles to be posteriorly displaced and the disks to be anteriorly displaced (internal derangement) (Figure 29-6).
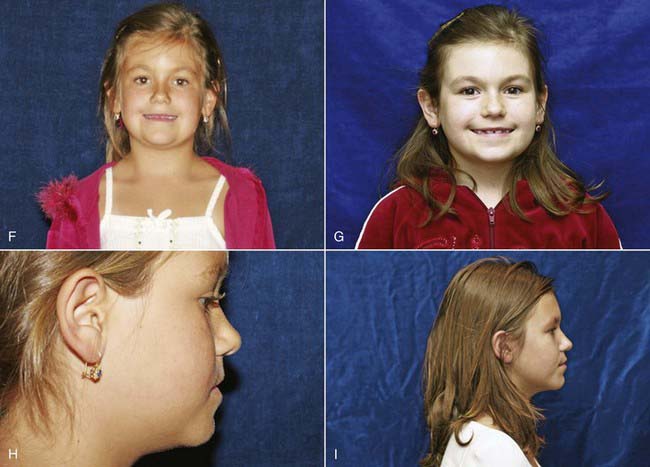
Correction of Unilateral Crossbite
The treatment of choice is to treat these patients at an early age (4 to 12 years) with a Schwarz appliance (removable) or a Hyrax appliance (fixed) to expand the maxillary arch. Both of these appliances accomplish this with midline screws adjusted twice per week. This bilateral expansion allows the mandible to center itself within a properly developed maxilla. Treatment is usually completed successfully within 3 months, including correction of the unilateral crossbite, TMD, and facial asymmetry. The patient is then encouraged to wear the appliance for 6 more months to prevent relapse (Figure 29-7).
Uprighting of Lower Posterior Teeth over the Basal Bone
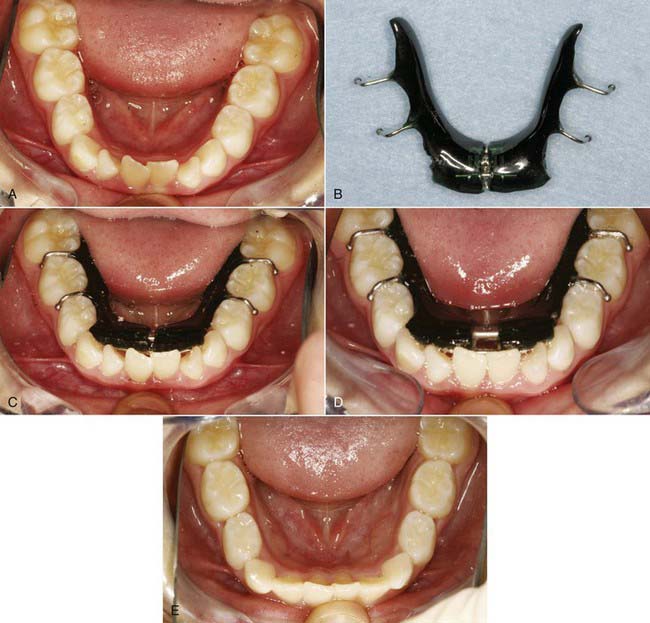
When the lower posterior teeth are lingually inclined, it is very difficult to obtain a proper occlusion. Certainly, it is not the ideal situation in which to fabricate crowns or bridges; it is preferable to have the teeth upright over the basal bone so that the direction of forces can be along the long axis of the teeth and not in a lingual direction, which tends to alter the occlusion. Lower posterior teeth that are lingually inclined can be uprighted with functional appliances to help ensure a proper occlusion and TMJ health. This uprighting of the posterior teeth widens the lower arch and increases posterior vertical dimension, which is one of the keys to TMJ health. This increased width of the lower arch also makes more room for the tongue, which ensures proper speech (Figure 29-8).
Establishment of Proper Vertical Dimension
Patients with deep overbites now have a posterior open bite, making it extremely difficult to chew and causing the TMJ to be unstable. The solution is to build up the first and second lower primary molars with composite to allow the patient to chew and to stabilize the TMJ. This is the treatment of choice for children who brux, have headaches, or experience ear symptoms such as ringing or congestion in the ears. Clinicians must take a complete TMJ history for each patient, regardless of age, to determine whether or not these younger patients have a problem. This technique leaves a space between the upper and lower first molars. Within 2 to 3 months the lower first molars will passively erupt to contact the upper first molars and close the posterior open bite. A new occlusal plane has now been created for the patient. The composite is left on the lower first and second primary molars to support the posterior vertical dimension. When the primary molars are exfoliated, hopefully the lower bicuspids will erupt to the level of the new occlusal plane. The author cannot overemphasize the importance of establishing proper vertical dimension in achieving TMJ health (Figure 29-9).
Two-Phase Orthodontic Treatment
Functional jaw orthopedic appliances can significantly change a patient’s profile and hence facial esthetics (Table 29-1). The ideal time to implement treatment is between ages 6 and 11 years, while the child is actively growing. The treatment of choice is two-phase orthodontic treatment, the objective being to solve the orthopedic problems early in the mixed dentition before the eruption of the permanent teeth. The objective in Phase I is to treat all Class II and Class III skeletal malocclusions with functional appliances to a normal Class I skeletal occlusion in the mixed dentition. Therefore, when all the permanent teeth erupt, the orthopedic (bone or skeletal) problems have been corrected, and the only concern will be orthodontics (crooked teeth). The advantage of this type of treatment is that it produces excellent facial esthetics and drastically shortens the treatment time in fixed braces.
| Phase I (Orthopedic Phase) Mixed dentition | Ages 6-11 years |
| Functional appliances | |
| Phase II (Orthodontic Phase) Permanent dentition | Ages 12-14 years |
| Fixed orthodontic braces |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses