25
The oral cavity and related structures
Chapter contents
|
25.4 The nerve supply, blood supply, and lymphatic drainage of the teeth and their supporting tissues |
25.1 Introduction
Technically, the oral cavity consists of the vestibule between the lips and cheeks externally and the teeth and alveolar processes internally and the larger oral cavity proper located internal to the dental arches. In clinical practice, the whole mouth is simply referred to as the oral cavity, but ‘vestibule’ is used for the specific area defined above. For charting of teeth and similar dental procedures, the mouth is divided into quadrants—upper right and left and lower right and left with the midline and occlusal surfaces of the teeth forming the dividing lines.
25.2 Examination of the living mouth
It is a crucial skill for dental students and practitioners to recognize the naked eye appearance of the structures in a normal healthy mouth and variations that occur; abnormal appearances can then be recognized, diagnosed, and treated successfully. Much of the macroscopical appearance is determined by the underlying gross anatomy so this must be understood too. The best way to examine the interior of the mouth is on a subject seated in a dental chair with clinical lighting and the use of a tongue spatula and a dental mirror where necessary. However, you will be able to see most of the important features by examining the inside of your own mouth in a well-lit household mirror.
The following description and illustrations apply to an adult mouth with a full secondary (permanent) dentition of two incisors, one canine, two premolars, and three molars in each quadrant, making 32 teeth in total. Apart from size, the major differences in childrens’ mouths are in the dentition. The primary (deciduous) dentition erupts into the oral cavity between the age of 6 months and 2 years. It comprises two incisors, one canine, and two molars in each quadrant, giving a total of 20 teeth. Most of the teeth of the secondary dentition erupt between the ages of 6 to 12, replacing the primary teeth; a combination of primary and secondary teeth, a mixed dentition, is found between these ages. Primary incisors and canines are replaced by their permanent successors, but the deciduous molars are succeeded by the permanent premolars; the three permanent molars in each quadrant are additional teeth.
Teeth may be lost from one cause or another throughout life and many older people have an incomplete dentition. The proportion of elderly subjects who are completely edentulous (without teeth) is decreasing as more effective preventative and conservative treatment take effect, at least in developed countries. In edentulous patients, the alveolar processes of both jaws are resorbed to some degree. Resorption may be so great that virtually no alveolar ridge can be seen.
25.2.1 The oral mucosa
Before embarking on the examination of the oral cavity, it is important to realize that the appearance of the oral mucosa is not uniform throughout the oral cavity; there are structural and regional variations. The oral mucosa may be divided into three major types.
Lining mucosa is non-keratinizing stratified squamous epithelium supported by connective tissue, the lamina propria, and submucosa containing minor salivary glands and some fat cells. This type of mucosa is generally reddish pink in colour; small blood vessels in the lamina propria are visible through the epithelium in areas where it is particularly thin. Lining mucosa covers the internal surfaces of the lips and cheeks, the ventral surface of the tongue, floor of the mouth, the soft palate, and alveolar processes up to the gingivae.
Masticatory mucosa, as its name implies, is found in areas subject to masticatory wear and tear, the gingivae, and hard palate. It has an external layer of keratinized stratified squamous epithelium supported by the lamina propria. There is no submucosa in the gingivae; it is also absent from the central regions of the hard palate but present under the rest of its surface. In the gingivae and hard palate lacking a submucosa, the lamina propria is firmly attached to the underlying periosteum by a meshwork of collagen fibres to form a composite structure called mucoperiosteum. Masticatory mucosa is thicker than lining mucosa. It is very pale pink in colour and appears almost white in areas of mucoperiosteum due to a greater thickness of epithelium and keratin masking underlying vessels.
Gustatory mucosa covers the dorsal surface of the tongue; its name indicates that it is involved in taste reception. The dorsal surface of the anterior two-thirds of the tongue is also involved in mastication and is, therefore, subject to abrasion. Gustatory mucosa has features in common with masticatory mucosa as well as specializations for taste reception. The epithelium and lamina propria form small projections called papillae; there are four types. The lamina propria is bound by collagen fibres to the underlying muscle and there is no submucosa. The appearance of gustatory mucosa on the tongue is described in Section 25.3.3.
The mucosa covering the posterior third of the tongue is nonkeratinized and covers nodules of lymphoid tissue which make up the lingual tonsil.
25.2.2 The vestibule
The vestibule is little more than a potential space when the mouth is closed since the lips and cheeks are normally closely applied to the labial and buccal aspects of the teeth and gingivae.
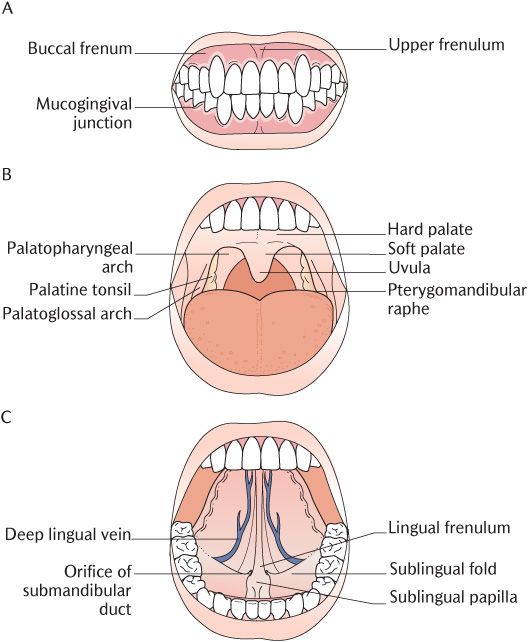
The floor and roof of the vestibule are formed by the reflections of the oral mucosa from the alveolar processes on to the cheeks and lips. The gutters formed by these reflections are called the sulci and are shown in Figure 25.1A. They are designated as the upper and lower buccal sulci in the region of the cheeks and upper and lower labial sulci in the region of the lips.
Pull your upper and lower lips away from your teeth and you will be able to see the frenulum, a narrow midline fold of oral mucosa connecting each lip to the corresponding alveolar ridge; the upper frenulum is usually larger than the lower and both are variable in size. The upper and lower sulci in the premolar regions are usually shallower than elsewhere because of the attachment of the fibres of the lip elevator and depressor muscles to the upper and lower jaw in this area. If you move the lips around, you will see that the folds of mucosa (the buccal frena) over these muscle attachments are very mobile. Care has to be taken during denture construction to ensure the margins of the denture base do not impinge on the frenula or muscle attachments, otherwise lip and cheek movements will dislodge it.
Fig. 25.1 The naked eye appearance of the oral cavity. A) The vestibule; B) The oral cavity with the tongue lowered; C) The oral cavity proper with the tongue raised.
The mucosa lining the lips and cheeks and the sulci has a smooth shiny appearance, is reddish pink in colour, and is loosely attached to underlying structures. A short distance from its reflection on to the alveolar processes the mucosa changes to masticatory mucosa which is tightly attached to the underlying periosteum to form a mucoperiosteum. The gingival mucosa is non-mobile and pinkish in colour. The bundles of fibrous tissue connecting the lamina propria to the bone give it a stippled appearance, somewhat like the texture of orange peel. As shown in Figure 25.1A, the distinct mucogingival junction demarcates the transition from reddish lining mucosa to pink masticatory mucosa; it is a scalloped line running horizontally 2–3 mm above or below the scalloped gingival margins. It is an important landmark when injecting local anaesthetic solution for local infiltration of maxillary teeth in particular (see Section 25.5.1 below).
A small papilla marks the opening of the parotid duct into the vestibule in the upper buccal sulcus opposite the crown of the upper second molar tooth, but this is not always visible. The buccal and labial minor salivary glands in the submucosa of the lips and cheeks open into the vestibule through ducts which are too small to see. You can feel these glands by running your tongue across the inside of the lower lip.
Other clinical aspects of the vestibule are covered in Box 25.1.
Box 25.1 Clinical anatomy of the vestibule
During the reduction of mandibular fractures, it is often necessary to fix the upper and lower teeth together, effectively splinting the mandible. With the teeth in occlusion, the narrow spaces behind the last molars are the only communications between the vestibule and oral cavity proper. Oral feeding can be achieved by passing liquid or semi-solid nutrients through the retromolar spaces using a vessel with a specially designed spout.
A cotton wool roll is usually placed into the upper buccal sulcus during dental procedures; it will lie against the opening of the parotid duct and absorb salivary secretions from the gland.
The duct of one of the buccal or labial glands may be blocked or damaged by minor trauma such as biting the inside of the cheeks or lips; saliva is retained within the gland causing it to swell into a buccal or labial cyst.
25.2.2 The oral cavity (proper)
With your mouth widely open as illustrated in Figure 25.1B, you will be able to see the roof of the oral cavity formed by the hard and soft palate, but the floor is largely obscured by the tongue. If you now raise your tongue as shown in Figure 25.1C, you will see the floor of the mouth formed by oral mucosa covering the mylohyoid muscles. The oropharyngeal isthmus is the junction of the oral cavity with the oropharynx behind. As you can see in Figure 25.1B and hopefully yourself or a willing subject, this is formed on each side by the palatoglossal arch, a fold of mucosa running from the side of the soft palate to the side of the tongue and covering the palatoglossus muscle. This fold is also known as the anterior pillar of the fauces.
The palate
Structurally the palate has two parts that differ in structure and function. Its features are illustrated in Figures 25.1B and 25.2. The hard palate is the bony partition between the nasal and oral cavities and forms roughly the anteriorly two-thirds. The muscular soft palate is attached to the posterior border of the hard palate and projects posteriorly, separating the nasopharynx and oropharynx posterior to the nasal and oral cavities, respectively. Four pairs of muscles attach to the fibrous palatine aponeurosis. The oral surface of the soft palate is concave at rest, conforming to the concavity of the bony hard palate. As shown in Figure 25.1B, a small conical process projects downwards from its free posterior margin; this is the uvula. The soft palate is highly mobile which you can verify watching the soft palate as you or the subject say ‘Aaaa’. When raised, it prevents food and drink entering the nasopharynx and nose during swallowing and also occludes air from the nose during speech; when lowered, the soft palate directs air through the nasal cavity.
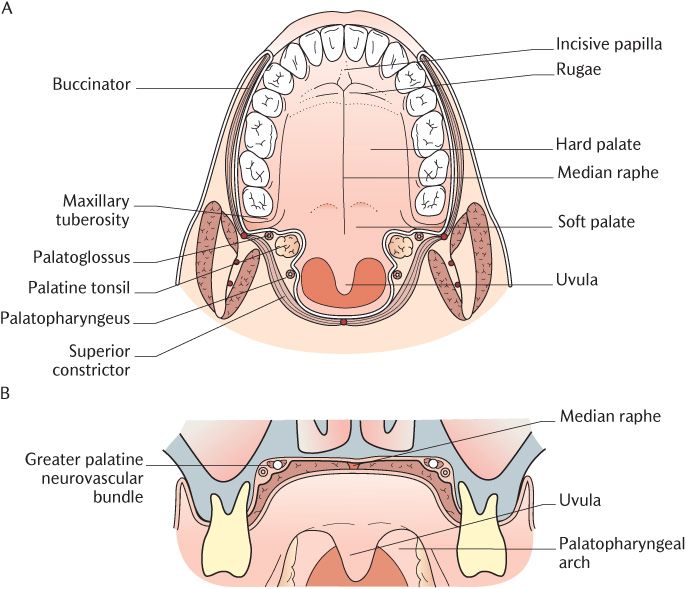
Fig. 25.2 A) An Inferior view of the palate; B) A cross section through the palate.
As illustrated in Figure 25.2B, the submucous layer in the hard palate varies in thickness from one region to another and is absent altogether in some areas. This variation produces the different appearances in different areas which are easily recognizable in the living mouth. In the gingival region adjacent to the teeth and in the midline raphe the submucous layer is absent and the lamina propria of the mucosa and the periosteum blend to form a mucoperiosteum. The mucosa is light pink in colour in these regions and may be almost white in the midline. The palatine raphe ends anteriorly at a small elevation, the incisive papilla, overlying the incisive fossa. The submucosa is relatively well developed between the midline area and the gingival region on each side but the lamina propria is still tightly bound down to the periosteum by bands of collagen. The spaces between these bands are filled with adipose tissue in the hard palate anterior to the canine teeth; the mucosa is raised into a number of transverse ridges called the palatine rugae. These provide a rough surface against which the upper surface of the tongue can press during preparation of food for swallowing and in speech. Further posteriorly mucous glands fill the spaces between the fibrous bands and the mucosa is thinner and pink in colour.
The visible junction of the hard and soft palate does not coincide exactly with the anatomical boundary between them. There is a narrow non-mobile part of the soft palate where the palatine aponeurosis is attached to the posterior margin of the bone. The vibrating line is the junction between the fixed and mobile parts of the palate and may sometimes be seen as a faint transverse groove at rest; the vibrating line is visible when saying ‘Aaaa’. This junction is an important landmark during upper denture construction as described in Box 25.2.
The upper alveolar process ends at the maxillary tuberosity, a rounded prominence posterior to the last molar tooth.
Box 25.2 How far back should an upper denture be extended?
Ideally, the posterior edge of a full upper denture should be positioned in the narrow non-mobile part of the soft palate between the bone–muscle junction and the vibrating line. If it is placed in front of the junction, it will sit on an area of thin submucosa and will consequently lack peripheral seal and cause discomfort. If it is extended behind the vibrating line, it may cause nausea and is likely to be dislodged by movements of the soft palate.
The tongue
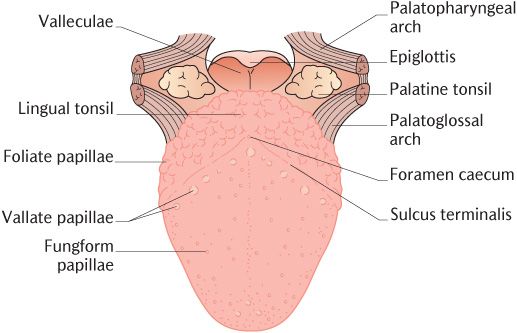
The tongue is much larger than can be appreciated by intraoral examination because it extends backwards into the oropharynx. Even with the tongue fully protruded, it is not possible to see its full extent although careful use of a dental mirror can reveal some additional features. The appearance of the full extent of the tongue is shown in Figure 25.3. The dorsum or upper surface is divided by the V-shaped sulcus terminalis into anterior two-thirds and posterior one-third although this is not visible in the living mouth without the aid of a dental mirror. As already described in Section 21.7, the parts on either side of the sulcus have different embryological origins and, therefore, nerve supply. As you can appreciate from Figure 25.3, the mucosa coverings of the two areas also differ.
Fig. 25.3 The dorsal surface of the tongue.
The anterior two-thirds are covered by gustatory mucosa formed into numerous papillae and tightly bound down to the underlying muscle. There are four types of papillae. The most numerous filiform papillae give the dorsum of the tongue a pink velvet-like texture. They are 2–3 mm long with pointed ends; secondary papillae point downwards and laterally so that the whole structure resembles a minute fir tree. They are keratinized and provide a rough surface for gripping and manipulating food. The outer layers of epithelium are continuously shed. In illness, this shedding may be delayed and the accumulated tissue mixed with bacteria is seen as a grey coating (fur) on the tongue.
The three other types contain taste buds in their lateral surfaces and the upper surface is keratinized. Fungiform papillae have a slightly constricted stalk and a hemispherical upper part which vaguely resembles a mushroom. They appear on the anterior tongue as bright red or sometimes pale spots that are most easily seen towards the sides and the tip. Taste buds are present on fungiform papillae.
As seen in Figure 25.3, there are about twelve large (circum)vallate papillae about 2 mm in diameter parallel and immediately anterior to the sulcus terminalis. They are recessed into the oral mucosa and surrounded by a deep circular furrow. The lateral surface of each papilla bears a large number of taste buds. You will not see vallate papillae on a routine oral examination unless you use a dental mirror to examine the back of the tongue. Minor serous salivary glands open into the sulci surrounding the vallate papillae. Their thin watery secretion probably efficiently removes taste molecules from the taste buds on the papillae in readiness for the next mouthful. Similar mechanism is not required for taste buds on the fungiform and foliate papillae as they are more accessible to saliva.
There are several vertical folds on the posterior part of the lateral margins of the tongue termed foliate papillae which cannot be observed during a standard intraoral examination. These are rudimentary in humans but well developed in other mammals.
Papillae are absent from the posterior third of the tongue where the covering mucosa membrane is raised into numerous low elevations due to the presence of nodules of lymphoid tissue in the submucous layer. These are known collectively as the lingual tonsil.
If you now raise your tongue as shown in Figure 25.1C, you will see that its under surface is covered by thin smooth lining mucosa which is pinkish red in colour and firmly attached to the underlying muscles. A deep lingual vein can be seen on each side through the thin mucosa. A median fold of mucous membrane, the lingual frenulum, connects the ventral surface of the tongue to the floor of the mouth.
The floor of the mouth
The floor of the mouth is also lined with thin smooth lining oral mucosa similar to that found on the under surface of the tongue. As shown in Figure 25.1C, the sublingual papillae are two small elevations located on either side of the attachment of the lingual frenulum to the floor of the mouth. These are the openings of the submandibular ducts. The sublingual folds extend posterolaterally from each papilla as a ridge produced by the underlying sublingual gland. The gland drains through several tiny ducts opened on to the crest of the fold which are too small to see with the naked eye.
The oropharyngeal isthmus and neighbouring region
As illustrated in Figure 25.1B, the palatoglossal arches can be seen most clearly if the tongue is depressed and the soft palate raised by saying ‘Aaaa’. The arches cover the palatoglossus muscles which arise from the soft palate and descend to the lateral side of the tongue. You may be able to see a second pair of folds, the palatopharyngeal arches (or posterior pillars of the fauces), a short distance behind the palatoglossal arches; these overlie the palatopharyngeal muscles extending from each side of the soft palate into the lateral walls of the pharynx. As shown in Figures 25.1B and 25.2, the palatine tonsils are submucosal masses of lymphoid tissue between the palatoglossal and palatopharyngeal arches on each side of the isthmus. The size of the palatine tonsils is extremely variable. Generally, they just protrude beyond the cover of the palatoglossal arch but can project much further or remain under cover of the muscle. They may have been removed by tonsillectomy. The surface of the palatine tonsils is pitted by tonsillar crypts but these are not always easy to see.
Open your mouth as wide as possible, then palpate lateral to the palatoglossal arch. You will feel the sharp anterior border of the ramus of the mandible. Trace this down towards the last lower molar tooth to the small retromolar pad of soft tissue. As illustrated in Figure 25.1B, you should see and feel a shallow groove medial to the ramus, marking the position of the pterygomandibular raphe. The raphe begins from the body of the mandible just behind the last lower molar tooth and runs upwards and medially to the hamulus of the medial pterygoid plate. The raphe is an important landmark for administration of inferior alveolar nerve blocks (see Section 25.5.2).
25.3 The anatomy of oral structures
25.3.1 The lips and cheeks
The lips are formed by the orbicularis muscle and loose connective tissue; they are covered by hairy skin externally and lining mucosa internally containing mucus-secreting minor salivary glands. The structure of the cheeks is similar with the muscle layer formed mainly by the buccinator muscle.
The sensory innervation of the skin and mucosa of the upper lip is from the infraorbital nerve and the upper cheek from the posterior superior alveolar nerves. The lower lip is innervated by the mental nerve and the cheek overlying the lower posterior teeth is supplied by the buccal nerve (see Figure 25.17). Secretomotor neurons to the glands in the upper lip and upper cheek pass from the pterygopalatine ganglion in the infraorbital branch of the maxillary nerve. The parasympathetic supply to the glands in the lower lip and lower cheek pass from the otic ganglion via inferior alveolar and buccal branches of the mandibular nerve.
The lips and cheeks are supplied with blood through the mental artery and the labial and buccal branches of the facial artery and their venous drainage is through tributaries of the facial vein. Lymph from the central region of the lower lip drains to the submental nodes; the rest of the lips and cheeks drain to the submandibular nodes.
25.3.2 The hard palate
The skeleton of the hard palate is formed by the palatine processes of the maxillae and the horizontal processes of the palatine bones as shown in Figure 25.4. The greater palatine nerve emerges from the greater palatine foramen and runs as far forwards as the canine tooth to supply the palatine mucosa, including the palatal gingivae with sensory innervation. As illustrated in Figure 25.4, the nerve runs forwards along a curved line situated in a groove in the bone just medial to where the alveolar processes curve up from the bony plate; the groove is often quite pronounced. The greater palatine nerve also carries parasympathetic post-ganglionic axons from the pterygopalatine ganglion to the palatine glands. The mucosa in the incisor region of the hard palate is innervated by the nasopalatine nerves which emerge on to the hard palate through the incisive foramen as illustrated in Figure 25.4. There is usually considerable overlap of the two sensory supplies. The sensory nerves supplying the palatine gingivae require local anaesthesia prior to certain dental procedures that may traumatize them, such as extractions, gingival surgery, and some restorative procedures. Anaesthesia of the palate is covered in Box 25.3.
The greater palatine artery emerging from the greater palatine foramen lateral to the nerve provides the blood supply of the whole of the hard palate; its course is shown in Figure 25.4. Observe how the artery passes into the incisive foramen in the incisor region where it supplies a small area of nasal mucosa. Blood drains from the hard palate through veins accompanying the artery into the pterygoid plexus. The lymph drainage is to the deep cervical nodes.
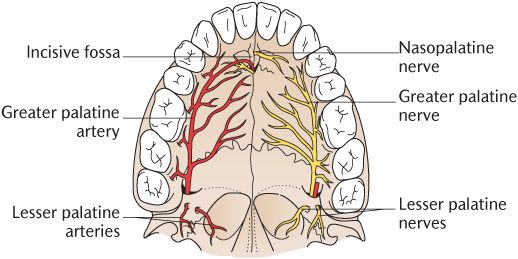
Fig. 25.4 The nerve supply (right) and blood supply (left) of the palate.
25.3.3 The tongue
The tongue is a highly mobile, muscular organ which plays a major part in mastication, swallowing, and speech. Its root is attached to the mobile hyoid bone.
The mucosal coverings of the tongue have already been described on p. 261. A few mucous glands are present on the under surface of the tongue near its tip. The glands in the posterior third of the dorsum are mucus-secreting.
The bulk of the tongue is made up of striated muscles. These can be divided into two groups—the intrinsic muscles with attachments entirely within the tongue and the extrinsic muscles which have one of their attachments outside the tongue. It is often claimed that the principle action of the intrinsic muscles is to alter the shape of the tongue whereas the extrinsic muscles change its position. However, it is virtually impossible to alter tongue shape without altering its position relative to other structures or to alter its position without affecting its shape. The actions of the two groups of tongue muscles are an example par excellence of the group action of muscles.
Extrinsic muscles
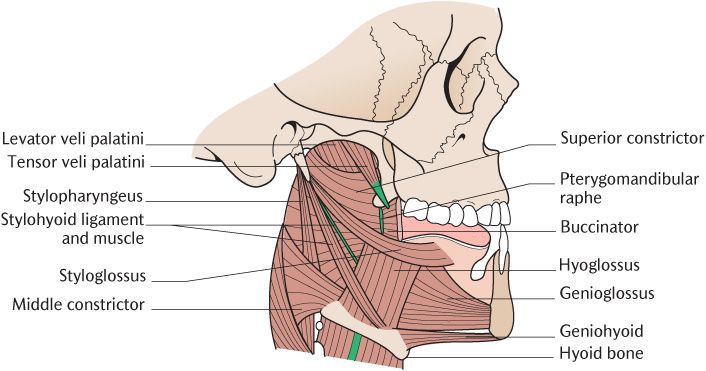
There are four pairs of extrinsic muscles—genioglossus, hyoglossus, styloglossus, and palatoglossus; their general arrangement is shown in Figures 25.5 and 25.6. Palatoglossus is better considered as a muscle of the soft palate on the basis of its development, nerve supply, and actions and is described in Section 28.3.1.
Box 25.3 Local anaesthesia of the palatine nerves
As you can see from Figure 25.2B, the greater palatine nerve runs close to the bone and the overlying mucosa is tightly bound down as mucoperiosteum as described on p. 261. Local anaesthesia in the region of the nerve is, therefore, painful for two reasons. It is difficult to avoid scraping the very sensitive periosteum and the tight mucosa leaves no room for spread of the comparatively small quantity of anaesthetic required. When palatal nerve block is required, the area is first painted or sprayed with topical anaesthetic. Once this has taken effect, an injection may be given if the operative procedure is likely to take time. It is important to make sure that the point of bevel of the needle is on the side away from the bone to minimize the risk of periosteal trauma.
Fig. 25.5 The extrinsic muscles of the tongue and styloid apparatus.
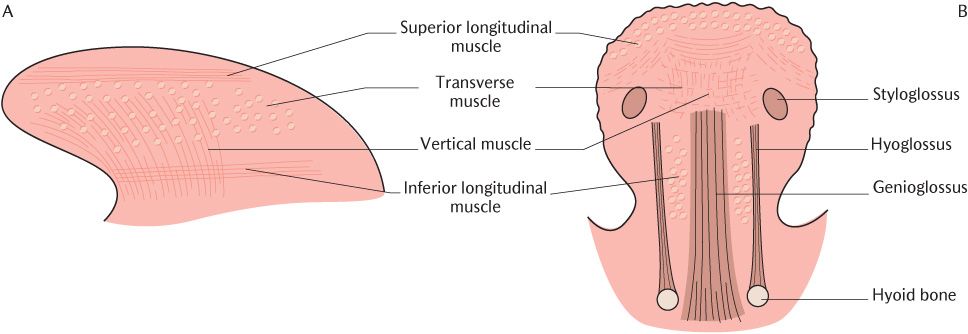
Fig. 25.6 The intrinsic muscles of the tongue. A) Lateral section; B) Transverse section
The genioglossus muscles form the bulk of the tongue. They lie adjacent to the midline separated from each other by a midline raphe of connective tissue formed from the perimysium of the two muscles. Each one is attached to the upper genial tubercle of the mandible immediately above geniohyoid which arises from the lower genial tubercle. Their fibres run posteriorly from the mandibular attachment, fanning outwards along the whole length of the ventral surface of the tongue from root to tip. From the attachments of the muscles, it is easy to appreciate that they draw the tongue forwards and pull down the central part of the dorsum; in reality, they produce a wide range of tongue movements by interacting with the intrinsic muscles.
As shown in Figure 25.5, each hyoglossus muscle is a quadrilateral sheet which arises from the upper surface of the whole length of the hyoid bone; its fibres ascend vertically to insert into the side of the tongue. Its action is to depress the tongue.
Figure 25.5 shows the posterior attachment of each styloglossus muscle into the lower end of the styloid process and adjacent part of the stylohyoid ligament. It runs downwards and forwards across the lateral surface of the superior constrictor muscle of the pharynx into the side of the tongue, interdigitating with the fibres of hyoglossus. It draws the tongue upwards and backwards.
Intrinsic muscles
The intrinsic muscles are arranged in four groups on each side of the median fibrous septum as shown in Figure 25.6. Their fibres run in all three dimensions and interweave with the extrinsic muscles; unlike the extrinsic muscles, they cannot be distinguish/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses