CHAPTER 25
Secrets in Computer-Aided Surgical Simulation for Complex Cranio-Maxillofacial Surgery
Cranio-maxillofacial (CMF) surgery is an encompassing term that involves the treatment of diseases, injuries, and deformities of the skull and face. CMF deformities can be either congenital or acquired and include dentofacial deformities, congenital deformities, defects after tumor ablation, posttraumatic defects, and deformities of the temporomandibular joint (TMJ). CMF surgery requires extensive presurgical planning because of the complex nature of three-dimensional (3D) anatomy of the skull and face.
1 How many patients with CMF deformities are in the United States?
In the United States, it is estimated that 17 million individuals aged 12 to 50 years (18% of this population) have malocclusions that are severe enough to warrant surgical correction.< ?xml:namespace prefix = "mbp" />
2 What are the current planning methods for CMF surgery?
CMF surgery requires extensive presurgical planning because of the complex nature of 3D anatomy of the skull and face. The current methods used to plan CMF surgery vary according to the type of surgery being planned but are not much different from the methods that are used to plan simple orthognathic surgery.
In general, current surgical planning methods for complex CMF deformities involve the following steps. The first step is to gather data and quantify the deformity from many different sources, including physical examination and anthropometric measurement, medical photographs, medical imaging studies (cephalometric radiographs and analysis, computed tomography [CT], etc.), and plaster dental models when the surgery involves the jaws. The second step is to simulate the surgery, including prediction tracings, plaster dental model surgery, or CT-based physical model surgery. The last step in surgical planning is to create a way of transferring the surgical plan to the patient at the time of the surgery. This is usually done by creating surgical splints, templates, measurements of the bone movements, or visual “clues.”
3 Why are the current planning methods often not adequate for planning complex CMF surgery?
ISSUES WITH TWO-DIMENSIONAL PREDICTION TRACINGS
The CMF surgery is usually simulated using prediction tracings. The tracings are made from the cephalometric radiograph by outlining the bones and soft tissues onto an acetate paper.
A significant drawback of prediction tracing is that it is two-dimensional (2D).
ISSUES WITH CT MODELS
Three-dimensional CT scans have been successfully used to visualize and quantify the patient’s condition. However, they have not been successfully used for surgical simulation because of two major reasons. First, the CT does not render the teeth with the accuracy that is necessary for surgical simulation.
With the fast development of cone-beam CT technology, the scanning slice thickness is reduced to 0.2 mm. It also has a better control on the artifacts. Radiation exposure to the patients has been significantly reduced. The cone-beam CT scanner has become a favorite gadget for orthodontists and dentists. However, in the treatment of complex CMF deformity, the surgeons want to see the “true” replica of CMF bones. The images from cone-beam CT have relatively lower contrast compared with regular medical CT images. This makes the segmentation process (to separate the bones from soft tissue on the CT image) rather difficult. After 3D reconstruction, it is common to observe that the anterior walls of the maxillary sinus or orbital floors are “mystically” missing on the 3D model. Although the artifacts produced by cone-beam CT are minimal, the rendition of the teeth is still inappropriate for simulating the final occlusion or for making the surgical splints.
ISSUES WITH CT-BASED PHYSICAL MODELS
Another means of simulating surgery is to use CT-based physical models produced by rapid prototyping techniques (e.g., stereolithography apparatus [SLA] models). Even though these models are useful, they have a number of disadvantages. One disadvantage is that in cases involving the occlusion, the teeth are not accurate enough for precise surgical simulation. This is because the CT image data, from which the models are built, are unable to accurately render the teeth and are also subject to artifacts. An additional plaster dental model surgery is still necessary to establish a new dental occlusion and to fabricate surgical splints. Another disadvantage is that it is impossible to simulate different surgeries on a single model. Once the model is cut, it is impossible to undo the cut.
ISSUES WITH PLASTER DENTAL MODEL SURGERY
Surgeries that involve the teeth are also simulated on plaster dental models.
Issues with Face-Bow Transfer
The ability of the surgeon to transfer the desired surgical plan to the patient during orthognathic surgery depends mainly on the accuracy of the surgical splint. The fabrication of an accurate splint requires that the models be mounted to replicate the position of the patient’s dentition. However, Ellis et al.
The advantage of using models that are accurately oriented to Frankfort horizontal becomes evident once the implications of using inaccurately mounted models are understood.
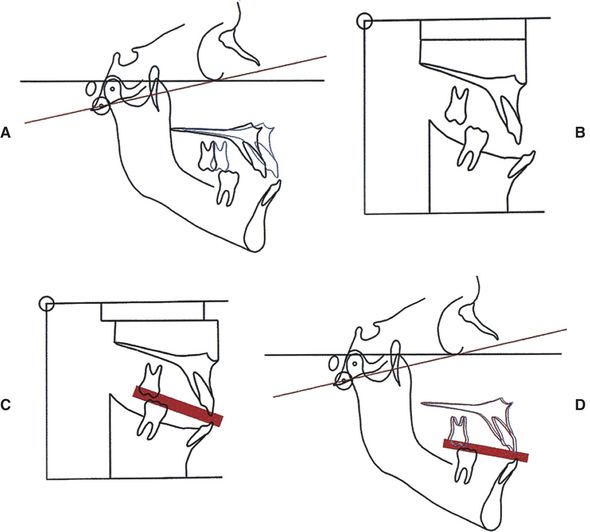
FIG 25-1 Face-bow transfer in a hypothetical patient. A, Prediction tracing in a hypothetical patient. The horizontal line in black is Frankfort horizontal. The red line is the axis-orbital plane, which is 12 degrees off Frankfort horizontal. The plan calls for a 10 mm maxillary advancement (blue line). B, The models mounted on an articulator. Note that the occlusal plane inclination of the mounted models is 12 degrees steeper than the actual occlusal plane. C, Model surgery. The maxillary model has been advanced 10 mm, and the intermediate splint (red) has been fabricated. D, The maxillary position at surgery. The blue outline represents the desired position for the maxilla. The red outline represents the actual position at surgery. Note that the actual position is 1.5 mm behind the desired position.
In order to solve this problem, researchers and clinicians have developed various techniques. Ellis et al.
Issues with Mandibular Autorotation
Predictable outcomes in double-jaw surgery depend on precisely positioning the maxilla. This is important, not only because an ideal maxillary position is necessary to achieve good mid-facial aesthetics, but also because the ultimate position for the mandible depends on it.
The first step in double-jaw surgery is to place an external reference marker (e.g., a K-wire or a screw) in the nasal bones. The vertical distance between this marker and the edges of the maxillary incisors is recorded. This measurement will help establish the correct vertical position for the maxilla. In double-jaw surgery, the maxilla is usually cut first. In order to position the maxilla at the time of the surgery, surgeons use an intermediate surgical splint that determines the AP and transverse position of the maxilla as well as any desired rotations in space. The intermediate splint is temporarily placed between the osteotomized maxilla and the mandible, and the teeth are wired in this position. The vertical position of the maxilla is then determined by autorotating the maxillo-mandibular complex to a predetermined vertical position, using the pre-determined distance between nasal marker and incisor edges as reference. Once the maxilla is in place, the dental fixation is released and the mandible is osteotomized and positioned according to the position of the maxilla. The splint is fabricated prior to surgery using plaster dental models, which have been mounted on an articulator. Articulators are mechanical devices that simulate the movement of the mandible. They are based on the principle that during opening and closing of the mandible in its most retruded position (centric relation), the condyles rotate around a hinge axis (hinge axis theory).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


