Aggressive Periodontitis
Periodontitis is the pathological manifestation of the host response against bacterial challenge that stems from a polymicrobial biofilm at the biofilm–gingival interface.51
Historical Background
In 1923, Gottlieb described a patient with a fatal case of epidemic influenza and a disease that he called “diffuse atrophy of the alveolar bone.”25 This disease was characterized by a loss of collagen fibers in the periodontal ligament and their replacement by loose connective tissue and extensive bone resorption, which resulted in a widened periodontal space. The gingiva apparently was not involved. In 1928, Gottlieb attributed this condition to the inhibition of continuous cementum formation, which he considered essential for the maintenance of the periodontal fibers.26 At that time, he called the disease “deep cementopathia,” and he hypothesized that this was a “disease of eruption” and that the cementum initiated a foreign-body response. As a result, it was postulated that the host attempted to exfoliate the tooth, thereby resulting in the observed bone resorption and pocket formation.
In 1938, Wannenmacher described incisor and first molar involvement and called the disease “parodontitis marginalis progressiva.”78 Several explanations evolved for the etiology and pathogenesis of this type of disease. Many authors considered this to be a degenerative, noninflammatory disease process and therefore gave it the name periodontosis.24,52,75 Other investigators denied the existence of a degenerative type of periodontal disease and attributed the changes observed to trauma from occlusion.10,46 Finally, in 1966, the World Workshop in Periodontics concluded that the concept of periodontosis as a degenerative entity was unsubstantiated and that the term should be eliminated from periodontal nomenclature.58 The committee did recognize that a clinical entity different from adult periodontitis may occur among adolescents and young adults.
The term juvenile periodontitis was introduced by Chaput and colleagues in 1967 and by Butler in 1969.9 In 1971, Baer defined it as “a disease of the periodontium occurring in an otherwise healthy adolescent which is characterized by a rapid loss of alveolar bone about more than one tooth of the permanent dentition.5 The amount of destruction manifested is not commensurate with the amount of local irritants.” In 1989, the World Workshop in Clinical Periodontics categorized this disease as localized juvenile periodontitis and as a subset of the broad classification of early-onset periodontitis.11 Under this classification system, age of onset and distribution of lesions were of primary importance when making a diagnosis of this condition.
In 1999, the World Workshop in Periodontics introduced a novel classification that was meant to eliminate the shortcomings of earlier endeavors to classify periodontal disease. Most importantly, the new 1999 classification sought “to discard classification terminologies that were age-dependent or required knowledge of rates of progression.”2 In the new classification scheme, several rapidly progressing periodontitis forms were united under the term aggressive periodontitis.
Classification and Clinical Characteristics
Features
The 1999 International Workshop for the Classification of Periodontal Diseases and Conditions defined the entity of aggressive periodontitis as being characterized by three primary features38 (see Table 25-1):
TABLE 25-1
Diagnostic Criteria to Distinguish Chronic and Aggressive Periodontitis
| Criterion | Aggressive Periodontitis | Chronic Periodontitis |
| Rate of progression | Rapid | Slow, but rapid episodes are possible |
| Familiar aggregation | Typical | Can be present when families share imperfect oral hygiene habits |
| Presence of etiological factors (e.g., plaque, calculus, overhanging restorations) | Often minimal | Often commensurate with observed periodontal destruction |
| Age | Often in young patients (i.e., <35 years old) but can be found in all age groups | Often in older patients (i.e., >55 years old) but can be found in all age groups |
| Clinical inflammation signs | Sometimes lacking (especially in patients with localized aggressive periodontitis) | Commensurate with amount of etiological factors present |
1. The rapid loss of attachment and tooth-supporting bone
With aggressive periodontitis, as compared with the more common variant chronic periodontitis, the loss of attachment progresses significantly faster. To evaluate this rapid course of destruction, the evaluation of clinical or radiographic data from earlier points in time is necessary, thereby allowing for the making of an estimate of the start of the disease. Note that the age of the patient per se is not a primary criterion for the diagnosis of aggressive periodontitis. Because earlier clinical records are often not available, many clinicians argue that a severe loss of attachment in young patients may conceivably be the result of a rapid course of disease progression. However, this is not generally true; the neglect of all oral hygiene in a periodontitis-susceptible individual over a decade will lead to severe attachment loss, even with a slow rate of progression. On the other hand, severe attachment loss in an older individual is not necessarily the result of long-lasting, slowly progressing disease. It is therefore inappropriate to use the age of an affected individual as a primary diagnostic criterion for the distinction of aggressive and chronic periodontitis. Note that, with chronic periodontitis, there are reportedly periods of rapid disease progression that can by themselves be misinterpreted as aggressive periodontitis.
2. The subject is otherwise healthy (i.e., not suffering from any systemic disease or condition that could be responsible for the present periodontitis)
There are systemic diseases that lead to severely altered host defenses against periodontal pathogens, often resulting in the rapid loss of attachment and tooth loss at early age. This disease is designated “periodontitis as a manifestation of systemic disease” (see Chapter 4). Note that the specific properties or abnormalities of some types of immune cells listed later in this chapter and reported to be often associated with the diagnosis of aggressive periodontitis do not themselves qualify for the aforementioned diagnosis.
3. The presence of familiar aggregation
The familiar aggregation of aggressive periodontitis cases is a feature that can be evaluated via medical and dental history questionnaires and by interviewing the patient. However, it is advisable to verify similar cases in the family, if possible, because many individuals may not be fully aware of their diagnoses. Many cases of “bad teeth that run in the family” turn up to be caries related or likely due to chronic periodontitis.
1. Inconsistency of the low amounts of present etiological factors (i.e., plaque) and the observed pronounced tissue destruction
2. Strong colonization by Aggregatibacter actinomycetemcomitans and, in some populations, Porphyromonas gingivalis
3. Immunological differences that do not entail the diagnosis of periodontitis as a manifestation of systemic disease
Subgroups
Aggressive periodontitis can be subclassified into localized and generalized forms. The diagnosis of the subcategory is based on clinical, radiographic, and historical data. These include the age of onset, the involvement of teeth other than first molars and incisors (i.e., the first permanent teeth to erupt), and the presence of a systemic antibody response against periodontal pathogens (see Table 25-2).
TABLE 25-2
Diagnostic Criteria for Localized and Generalized Aggressive Periodontitis
| Criterion | Localized Aggressive Periodontitis | Generalized Aggressive Periodontitis |
| Age of onset | Circumpubertal | Most often <30 years of age, but can also occur in older individuals |
| Serum antibody response against infecting agents | Robust | Poor |
| Destruction pattern | Localized attachment loss at incisors and first molars; interproximal attachment loss at two or more permanent teeth, one of which is a first molar, and involvement of two or fewer teeth other than the first molars and incisors | Generalized interproximal attachment loss at three or more permanent teeth other than the first molars and incisors |
| Additional | Episodic nature of attachment loss |
Generalized Aggressive Periodontitis.
Two gingival tissue responses can be found in cases of GAP (see Figures 25-1 and 25-2). One involves severe, acutely inflamed tissue that is often proliferating, ulcerated, and fiery red. Bleeding may occur spontaneously or with slight stimulation, and suppuration may be an important feature. This tissue response is thought to occur during the destructive stage, in which attachment and bone are actively lost.

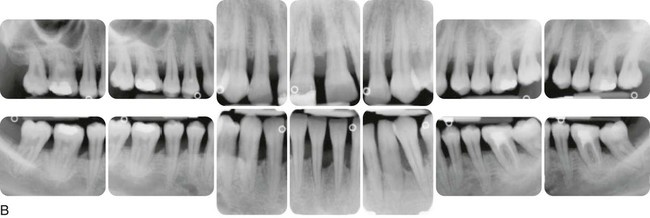
Generalized aggressive periodontitis in a 28-year-old Caucasian, female, nonsmoking patient. A, Clinical views with minimal amounts of calculus and plaque. B, Radiographically, bone loss of 50% or more was present at all teeth.
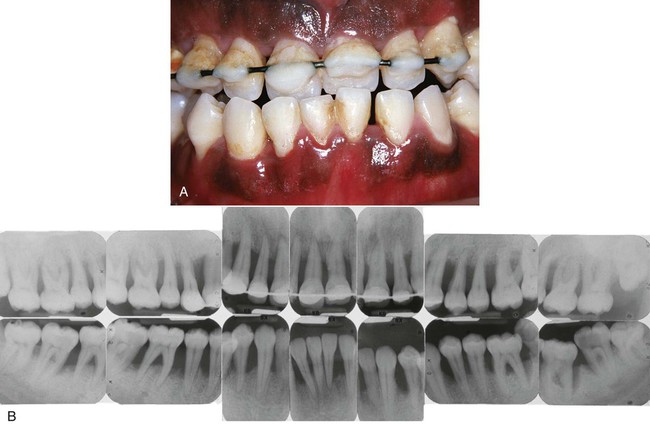
Severe generalized aggressive periodontitis in a 22-year-old black, male patient with a family history of early tooth loss through periodontal disease. A, Clinical view showing minimal plaque and inflammation. A provisional wire-and-resin splint had been placed by the general practice dentist to stabilize the teeth. B, Radiographs showing the severe and generalized nature of the disease, with all erupted teeth affected.
In other cases, the gingival tissues may appear pink, free of inflammation, and occasionally with some degree of stippling, although stippling may be absent. However, despite the apparently mild clinical appearance, deep pockets can be demonstrated by probing. Page and Schroeder thought that this tissue response coincides with periods of quiescence in which the bone level remains stationary.53
Localized Aggressive Periodontitis.
Localized aggressive periodontitis (LAP) is usually found in younger individuals than GAP (see Figures 25-3 and 25-4). It is characterized by more pronounced systemic antibody titers against periodontal pathogens than are found in patients with GAP. This could indicate that, in individuals who are susceptible to disease but who also have the ability to enact a robust response against pathogens, the disease might be limited in extent (i.e., LAP). Alternatively, in individuals with a lesser humoral response, the disease would not be limited to the first permanent teeth, and the patient would develop GAP. This would mean that LAP and GAP would merely be phenotypic variations of the same underlying disease. This assumption is backed by several reports that show a sequence of LAP and GAP in the same individuals over time.8,31,69

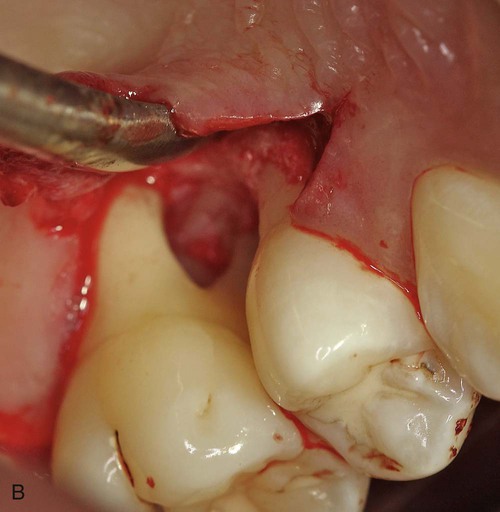
Localized aggressive periodontitis in 15-year-old black, female patient who had a twin with similar disease. A, Clinical view showing minimal plaque and inflammation, except for localized inflammation on the distal side of the maxillary left central incisor and the mandibular right central incisor. B, Radiographs showing localized, vertical, angular bone loss associated with the maxillary and mandibular first molars and the mandibular central incisors. The maxillary incisors show no apparent involvement. C, Surgical appearance of the localized, vertical, angular bony defects affecting the mandibular incisors. Note the wide circumferential nature of the defects and the lack of calculus on the root surfaces.

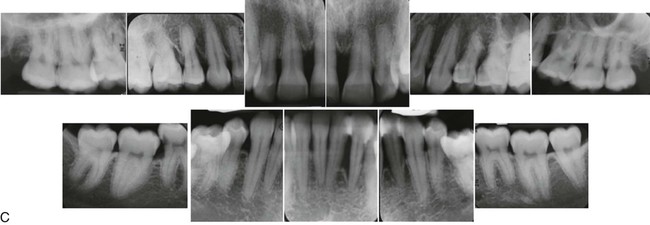
Localized aggressive periodontitis in an 18-year-old Caucasian, female, nonsmoking patient. Familiar aggregation was reported. A, Clinical view showing recessions at the incisors and first molars. B, Intraoperative view showing advanced, localized, angular bony defect associated with a first molar. C, Radiographs showing pronounced localized, angular bone loss. (Courtesy Dr. Hendrik Schulze, Bonn, Germany.)
Epidemiology
The question of the prevalence of aggressive periodontitis in different populations is complicated by the fact that the currently used classification2 is relatively young and not easy to apply in epidemiological studies. Therefore, many available studies either (1) report on older, previously used entities of periodontitis that showed early onset or rapid progression but that are not interchangeable with aggressive periodontitis or (2) report only on periodontitis severity and not on diagnosis (for a detailed review, see reference 15).
Case Definition
As a result, to date, the authors are only aware of a single methodologically sound epidemiological study of aggressive periodontitis that was performed in a population of young Israeli army recruits.40
Thus, to be able to assess the prevalence of aggressive periodontitis in other populations, Demmer and Papapanou15 proposed the use of the generally accepted case definition (see Chapter 5) for periodontitis that was proposed by a working group of the U.S. Centers for Disease Control and Prevention and the American Academy of Periodontology17,54 in combination with the age of the study subject. Specifically, they assessed available studies for the proportion of subjects 25 years old or younger who suffered from moderate or severe periodontitis as well as the proportion of subjects between the ages of 26 and 35 years who suffered from severe periodontitis, both according to the definition proposed by the U.S. Centers for Disease Control and Prevention.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


