Interdisciplinary Strategies for Treating Adult Patients
Mithran S. Goonewardene, Bradley G. Shepherd
The contemporary clinician is generally presented with a patient or parent who is well informed because of the significant opportunities to research treatment options on electronic media. Patients often present with certain expectations resulting from these search activities and are generally aware of possibilities to modify tooth form and color using contemporary methods. Moreover adult patients now represent a significant proportion of individuals seeking orthodontic treatment for esthetic improvement because of changing opportunities or the need for comprehensive rehabilitation.1,2
Adult patients present significant challenges across many spheres of concern.3–5 Often adults have been affected by periodontal disease, attrition, abrasion, and erosion. The most significant challenge to successful treatment may be the effects of long-term and sometimes unsatisfactory restorative dentistry, which may be contributing to the progression of multifaceted deterioration. Moreover adult patients are generally more fastidious but have a degree of psychological tolerance to treatment that must be considered carefully. Adults also measure the compromise of treatment very carefully and must make difficult decisions for themselves, factors that are not as significant for adolescent patients. Finally, from the orthodontist’s perspective, biomechanical side effects usually compensated by growth changes demand more precise execution of tooth movement strategies.
Adult patients often engage in the treatment process and play an active role in decision-making. It is important to realize that there is often a lack of concordance between the clinician’s and the patient’s perception of treatment success. Therefore contemporary clinicians attempt to achieve realistic treatment goals that aim to marry the objectives of both clinician and patient.
Concepts of Interdisciplinary Treatment Planning
Approximately two-thirds of the population exhibit malocclusion, with some individuals able to progress to later adulthood with minimal intervention from a restorative dentist.6 However, a combination of caries-related restorative dentistry procedures, tooth loss, periodontal problems, and tooth surface loss may contribute to challenges for the restorative dentist.7 These issues may result in significant migration of teeth into positions that make routine dentistry problematic. Moreover a significant number of individuals may have had a preexisting malocclusion with some degree of skeletal discrepancy and associated dental compensations, which place unrealistic demands on the restorative dentist and their materials as they attempt to manage patients’ concerns (Fig. 24-1).

Figure 24-1 A–C, A 57-year-old male patient has been partially restored in an attempt to address cosmetic issues related to tooth surface loss and a generally heavily restored dentition. The impact of the significant Class II relationship, deep overbite, and nocturnal bruxism were not considered in the treatment planning process and significant acceleration of lower anterior wear occurred.
The majority of orthodontic patients present following referral from a restorative dentist but some may present spontaneously without referral. In well-established offices with an excellent history of communication between many practitioners, the patients are usually well informed about the problems prior to orthodontic referral. However, a number of patients may be referred for assessment without any preliminary knowledge related to their problems and the issues associated with management (Fig. 24-2). The management of these patients is critical and sometimes challenging. The orthodontist often takes on the role of facilitator among a new group of clinicians to ensure that the patient and all associated clinicians have similar appreciation of the diagnosis, treatment goals, and possible solutions for the patient’s circumstances. In patients with more complex treatment needs that may require periodontal and restorative intervention, treatment requires a consistently coordinated approach for successful management.8,9
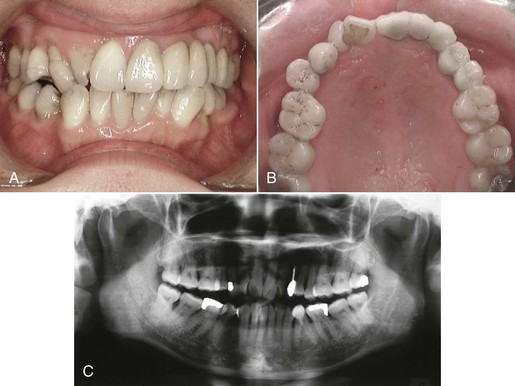
Figure 24-2 A 50-year-old female patient presented soon after placement of a fixed prosthesis by her general dentist. A and B, Intraoral photographs reveal an attempt to replace five dental units after removal of the upper left canine due to failure of post and core crown. There has been no regard for the preexisting malocclusion and the resultant aberrant contours in the compromised final prosthesis. C, The pre-treatment radiograph clearly reveals significant periodontal problems and irregularity that were not addressed as part of the overall treatment plan.
Unidisciplinary Treatment
Unidisciplinary treatment occurs when a clinician attempts to treat a complex problem in isolation.9 It is often disappointing to see a patient who has been treated with a succession of restorative procedures alone, in an attempt to manage a complex dental problem that may be the result of an interaction of tooth loss and periodontal disease on an aberrant skeletal jaw base (Fig. 24-3). Some clinicians even attempt to deliver care in periodontics, endodontics, and orthodontics without the skills and knowledge needed to consider all of the risks and benefits of various therapies. Moreover, these clinicians might not have the skills required to deliver the appropriate therapy to the expected standard of care.

Figure 24-3 A–C, A 53-year-old female patient with a significant Class III malocclusion has been restored with a near complete prosthetic maxillary rehabilitation with no regard to the skeletal relationship. An attempt was made to compensate the prosthetic tooth position for the aberrant jaw relationship, which resulted in excessive loads concentrated on the prosthesis and resultant porcelain fractures. D–F, A 40-year-old female patient presented 7 years after consulting her general dentist for improvement in her esthetics. She has experienced periodontal problems resulting from a combination of labial positioning of the lower incisors, plaque-induced periodontal inflammation, and aggressive tooth brushing. The “overcontoured” veneers have also directly contributed to her periodontal problems. Unfortunately the general dentist did not appreciate the impact of the underlying malocclusion on future stability and simply offered her a veneer option. Orthodontics was never presented to the patient as a potential solution.
Multidisciplinary Treatment
Multidisciplinary treatment progresses beyond unidisciplinary treatment in that clinicians from multiple disciplines are integrated into the treatment in a haphazard way. Often the course of multidisciplinary treatment is dependent on which clinician is seen first.
There are many examples of orthodontic or restorative dentistry initiated in patients with undiagnosed periodontal disease. Orthodontists often complete treatment in partially edentulous patients without consulting the restorative dentist. This may result in inadequate spatial arrangements, with too much space or too little space for an optimal prosthetic outcome.
The characteristic shortcoming of multidisciplinary treatment is poor communication between clinicians who independently might be excellent clinicians but who do not understand the considerations of all specialty areas and their prospective influence on the overall management of the patient (Fig. 24-4).9
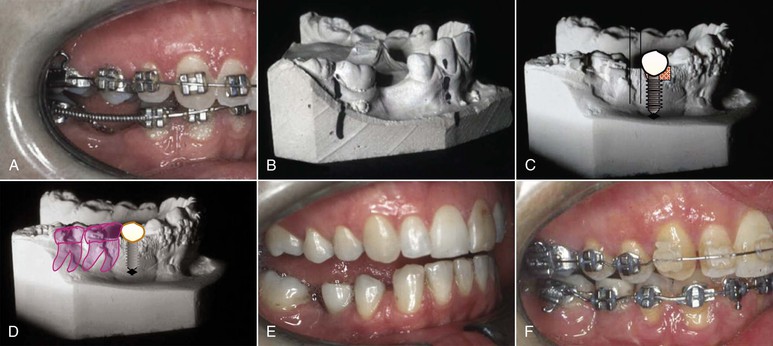
Figure 24-4 A, Adult patient presented to the office in appliances for completion of her orthodontic treatment, which included mandibular advancement surgery and preparation for prosthetic teeth. The transferring orthodontist indicated that the patient was ready for the mandibular surgery and implant placement. B, The pre-treatment model demonstrates a tipped molar. The treatment plan aimed to move the molar distally and open up the space. C, A progress model clearly demonstrates inadequate consideration by the orthodontist for the prosthetic replacement. The decision was made without the input of a prosthodontist. D–F, The appliances were removed and a new plan was formulated. This plan included placement of a premolar-sized implant in the lower right second premolar region, which would be used to protract the molars and close the excess space. The mandible was advanced and the occlusion was detailed into this position. This case demonstrates the need for a coordinated approach with several clinicians involved in the decision-making process.
Interdisciplinary Treatment
Interdisciplinary treatment is characterized by a group of clinicians from numerous backgrounds all contributing to the management of a patient for which their expertise is needed. It is important to establish a working team of specialists who can communicate effectively and meet regularly.8,9
Once a patient has been recognized as needing interdisciplinary management, a specific series of procedures must be considered and adhered to. This ensures that the patient’s interest is foremost.
Preliminary Discussion: Establish Interest
Not all patients are suitable candidates for complex interdisciplinary treatment. After careful consideration of the patient’s primary complaint, it is important to clearly determine the patient’s needs. A common mistake in advising patients with complex needs is to immediately assume that the patient will progress through complex and costly diagnostic processes and interdisciplinary consultations. One clinician should take responsibility for briefly outlining the nature of the problem, the time commitment, and the possible financial cost by establishing a well-defined roadmap for treatment. Often the orthodontist assumes the role of facilitator and he or she must recognize that there are occupational biases between practitioners in various disciplines that may influence the balance of information transfer.10
A simple patient-specific set of records may be considered at this stage to satisfy the requirements of the initial evaluation and information exchange between clinicians (Fig. 24-5).
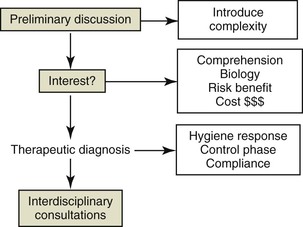
Figure 24-5 The sequence of managing patients from initial consultation to interdisciplinary consultations. It is important that this is performed in a progressive manner to ensure that the patient understands the complexity and general goals of treatment. This may include a period of preliminary treatment that may be considered a therapeutic diagnostic process and may determine the suitability of patients for more extensive treatment.
In patients with moderate to extreme deterioration of the dentition it is important to reflect on how the patient arrived at this juncture. Often the situation has resulted from an unfortunate combination of opportunity and finances; occasionally it has resulted from neglect by the patient, the dental care provider, or both. It is important for the clinician to exercise good judgment and consider whether the patient is a candidate for complex treatment and its associated demands on the patient.
Patients with Significant Periodontal Problems
In patients with significant long-standing pathology such as periodontal disease, caries, and/or periapical pathology, a period of periodontal and caries control therapy may be necessary to establish optimal health prior to initiating orthodontic treatment.11 This period is therefore seen as a provisional or therapeutic diagnostic test. In fact, this may be an ideal method of screening possible interdisciplinary patients. The cost and significant time commitment will identify problematic patients prior to committing to potentially risky tooth movement and placement of complex prostheses in the presence of uncontrolled disease (Fig. 24-6).
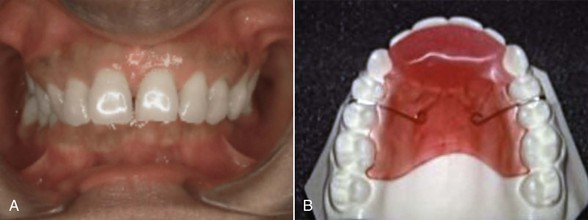
Figure 24-6 A, A 42-year-old patient presented with significant restorative dentistry, periodontal problems, and a deep overbite that required comprehensive interdisciplinary treatment. The patient was sent for stabilization of the periodontal problems and provisional restorations prior to definitive interdisciplinary treatment. B, A removable biteplate serves a dual purpose of relieving the direct gingival impingement on the palatal tissue margins and helping in a preliminary assessment of the patient’s capacity to conform to the demands of treatment. In such patients it is often important to assess whether they will comply with the challenges of multiple appointments over the treatment time, particularly if their history has included periods of neglect and irregular dental attendance.
There is nothing more disastrous for the interdisciplinary clinician than to encounter a patient who fails to attend regular treatment sessions or fails to adhere to the rudimentary home care regime. It is beneficial for all concerned to identify these issues at the outset. In some circumstances patients are placed in a removable biteplate or occlusal splint in addition to the periodontal treatment. This enables the orthodontist to evaluate patient compliance with an appliance as well as the patient’s attention to appointments for orthodontic review.
Patient Review and Definitive Record Taking
Once the patient has been stabilized and is considered a favorable candidate for treatment, he or she may progress to a more complex stage of acquiring complete diagnostic records and referral for interdisciplinary consultations with appropriate clinicians. These may include an orthodontist, restorative dentist or prosthodontist, periodontist, oral surgeon, endodontist, physician, and oral radiologist and computer scientist.8
Numerous developments in information technology enable clinicians to share material in electronic format and, with patient consent, even to share the treatment records of multiple clinicians. This is a time- and cost-effective method for clinicians and patients that provides ready access to all available records and treatment progress by team members.
Establish Treatment Goals
Once the database has been established, a detailed and prioritized problem list is developed.12 The problem list forms the basis for developing a list of “ideal treatment goals.” One clinician will usually take the responsibility of developing this list and circulating the findings to all members of the treatment team.
Communication is facilitated by modern interactive software that enables sharing of data. In addition, many clinicians will meet regularly using a roundtable discussion format to discuss complicated cases. This is valuable time for clinicians even if a case does not involve consideration of a specific specialist’s skills,8,9 as the discussion will enable all clinicians to remain current with developments in other specialty areas. In formal training or treatment institutions, patients are often consulted in comprehensive multidisciplinary clinics and this interaction facilitates interdisciplinary management with all clinicians present.
Considerations in Goal Setting
There are many factors to consider when establishing the goals for a patient’s treatment, including:
• Patient values and quality-of-life issues
• Growth and maturation issues
• Treatment outcomes and associated maintenance requirements
The patient’s primary complaint and dental history are significant at this point because the best indication of the need for intervention is the observation of any deteriorating status in the dentition. It is often more difficult to make a decision to treat a younger adult with a malocclusion than to treat an older individual. Older patients may reveal signs of breakdown such as tooth wear, soft tissue impingement, and/or tooth migration related to their occlusal relationships or they may show no adverse effects from their malocclusions. This is perhaps the most significant aspect in decision-making after the patient’s primary complaint.
In young children it is usually a simpler decision to treat malocclusion to an ideal Class I occlusion. The biological and psychological cost is usually reduced in the presence of optimal oral health. However, in adults careful consideration must be given to achieving realistic goals, which may not be the same as the ideal goals.8 For example, it is not always necessary to treat a posterior crossbite with a shift as part of interdisciplinary treatment nor to achieve an ideal Class I posterior occlusion in every circumstance, particularly if this relationship is not considered to be problematic to the patient’s primary complaint and treatment stability.
A series of treatment solutions with modified goals may be considered by the interdisciplinary group and often team members will be surprised by a totally satisfactory solution that they had not considered that is introduced by a colleague in another discipline (Fig. 24-7).9 Clinicians tend to have an occupational bias when considering treatment options and this type of decision-making environment ensures a thorough evaluation of many possible scenarios.
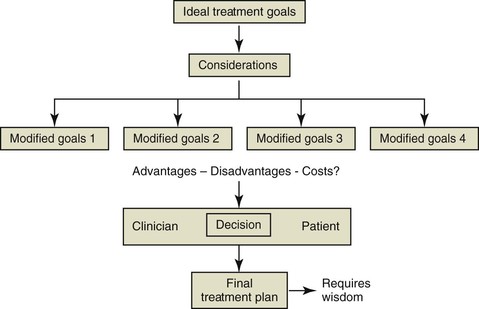
Figure 24-7 Possible complex considerations that influence attainment of ideal treatment goals. A carefully considered treatment plan that represents a joint decision between the patient and clinicians based on their relative value systems will be formulated.
It is important to consider the risks and benefits and the patient’s perspective when outlining the best treatment solution for the patient. One clinician will usually be responsible for carefully and systematically finalizing the discussion with the patient to ensure agreement on a solution that encompasses the patient’s and clinicians’ desires, acknowledged risks and sacrifices, and associated financial considerations. This is particularly important when considering replacement of missing teeth.
Many interdisciplinary treatment plans include replacement of missing teeth and the restorative dentist or prosthodontist must have a comprehensive discussion with the patient on the risks and benefits of the range of replacement options, including removable partial dentures, fixed prostheses, and/or implants. Historically, the success of a restorative option has been simplistically reported as retention of the prosthesis with limited pathology. A more contemporary view of success includes esthetics and periodontal health outcomes as well as factors such as the longevity versus indexed cost, invasiveness and biological cost, and esthetic outcome.4,10–14 These contemporary studies have included a complex assessment of quality-of-life issues from the patient’s perspective in seeking and receiving therapy.
Diagnostic Model Setup
In patients who require routine orthodontic treatment it is fairly easy for the experienced clinician to visualize the final occlusion. However, in patients who require atypical treatment such as lower incisor extraction, canine or incisor substitution, or complex interdisciplinary treatment involving prosthetic replacement of several teeth and even jaw surgery, it may be difficult for clinicians to visualize the final outcome (Fig. 24-8). Technological advances have seen the application of digital study models and the development of digitally assisted setups that facilitate assessment of numerous treatment options on a three-dimensional imaging program but many clinicians still prefer plaster and wax setups (Fig. 24-9).

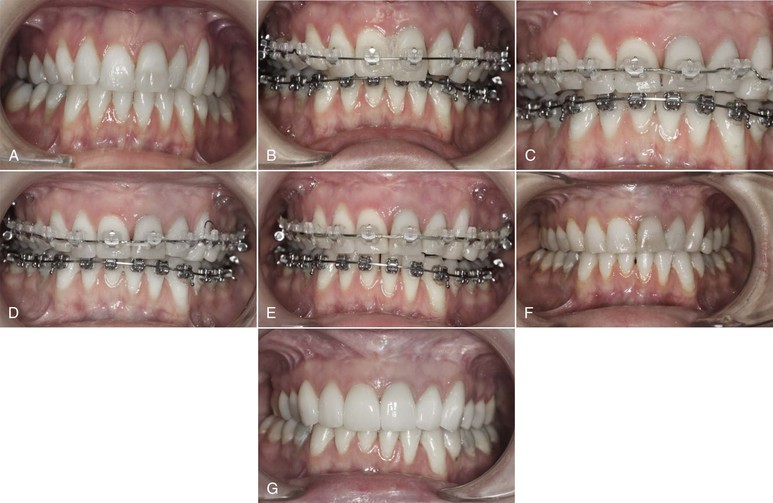
Figure 24-8 A–C, Patient presented with missing lower left first molar and Class I malocclusion. D–F, Plaster and wax diagnostic setup clearly demonstrates alignment of teeth and uprighting of lower left molars in preparation for a prosthetic replacement. All clinicians involved in treatment are now able to visualize the final outcome.
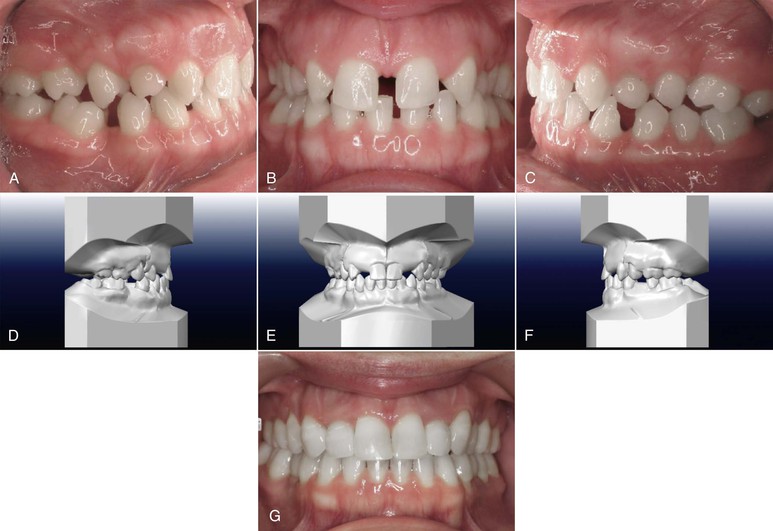
Figure 24-9 A–C, Pre-treatment intraoral views of a partially edentulous patient who requires preprosthetic orthodontics. D–F, Digitally generated diagnostic setup. G, Postorthodontic restorative outcome.
The diagnostic setup is usually prepared after consultation with key clinicians involved in the specific plan. It enables the clinicians to realistically assess:
The diagnostic setup is the key communication tool used by all clinicians and the patient.13 Various simulations may be presented with their relative merits and risks, which will assist in developing the final treatment plan. Moreover once the plan has been accepted by all concerned, it is a key reference point to which all parties, clinicians, and the patient may refer through the course of treatment.
Facilitating Communication: Treatment Sequencing
The final treatment plan will reflect the combined decision of the group of clinicians and the patient. It is now critical to ensure that all clinicians recognize their specific role and the sequence of treatment.
The absence of a treatment sequencing document often results in poor communication and less than optimal outcomes. Clinicians may be surprised when a patient attends for a specific procedure if the recollection of the goals at this stage is not immediately apparent. Significant effort may have to be expended by the clinicians to reacquaint themselves with the treatment plan. Inherent complications in treatment efficiency and possibly inappropriate treatment procedures can result if a clear outline of the goals is not understood.
An interdisciplinary plan will be formulated, principally by the team leader. The orthodontist frequently facilitates this process, as he or she often spends significantly more time with the patient during the course of treatment (Figs. 24-10 and 24-11). Equally so, other team members may find themselves assuming this role at specific phases of the plan. The team leader must ensure that a comprehensive list of procedures with specific goals and timelines is outlined and circulated to all clinicians and to the patient.8 This is a key component in ensuring excellent communication between all parties. It ensures that all clinicians are familiar with the stages of treatment and ensures an efficient transition through treatment. Moreover patients may wish to review their progress by referring to the treatment sequencing document.
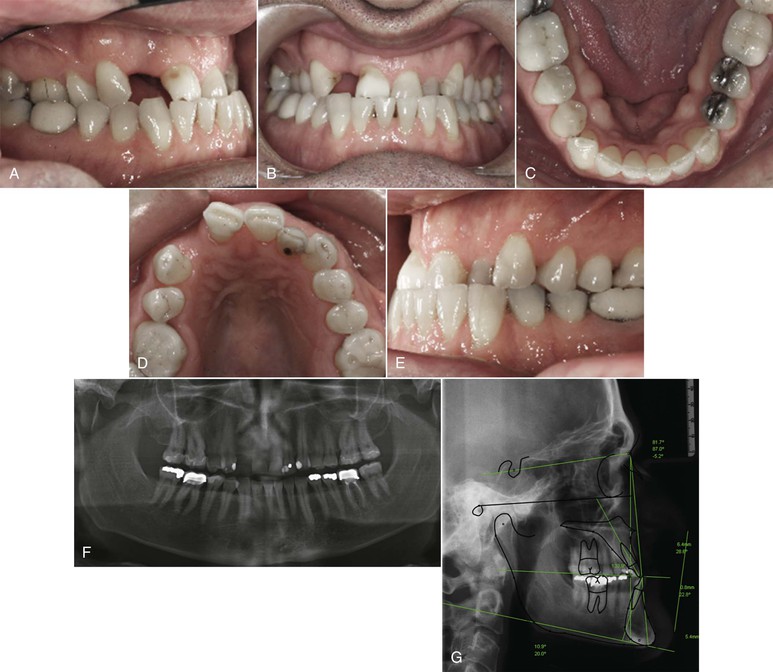
Figure 24-10 A–E, Intraoral views of a 42-year-old male patient who presented with a Class III malocclusion, advanced periodontal problems, a missing lateral incisor, and attrition of the upper central incisors. F, Panoramic radiograph revealed advanced attachment loss around the upper central incisors. G, Cephalometric radiograph revealed a significant Class III skeletal relationship with a retrognathic maxilla that will be managed by maxillary advancement surgery.
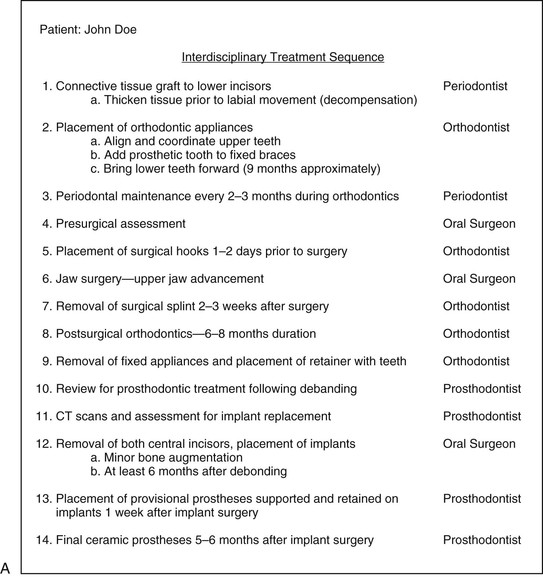

Figure 24-11 A, Interdisciplinary treatment sequence for the patient shown in Figure 24-10. It addresses his periodontal problems first, followed by complex orthodontics, restorative dentistry, and oral surgery. The key elements in this treatment plan are to establish the sequence of events and determine whether his upper central incisors need to be replaced, as they were considered to have a questionable prognosis. The decision by the periodontist and prosthodontist was that implant replacement would offer a more predictable outcome than attempting to retain these teeth. The timing of extraction and implant replacement (with or without grafting) must be determined carefully by the team to ensure that treatment flows smoothly. B–D, Final intraoral photos of the patient following orthodontic treatment, maxillary surgery, and implant replacement. CT, Computed tomography.
Periodontal Implications in Interdisciplinary Treatment
Adults represent a significant number of patients referred for interdisciplinary treatment. The adult patient often has preexisting periodontal problems that need to be evaluated. These may include:
Referral for assessment and management of periodontal problems is probably the most significant step in interdisciplinary treatment.14 Many patients find themselves in this circumstance because of a historical lack of home care and regular dental review. It is often difficult to gauge whether adult patients are committed to what will be a challenging treatment regime in terms of both time and cost. The initial periodontal assessment is often considered a preliminary screening process during which adherence to issues of home care,11 regular appointment attendance, and suitability for a potentially extended course of treatment may be determined.15
The periodontal assessment may include a process of therapeutic diagnosis in which tissue response to treatment is assessed. The primary goal of this treatment is to eliminate and stabilize the disease process. It also enables the clinicians to identify the specific location and architecture of bony and soft tissue lesions.16 These include crater defects; one-, two-, and three-wall defects; furcation defects; and localized horizontal bone loss.17 Through careful consideration of the relative prognoses of various treatment procedures, the interdisciplinary team will determine whether periodontal treatment alone is indicated or the orthodontist may modify the position of the teeth to effect changes in the bony architecture.18,19
Consideration may be given to bone regeneration procedures16,20,21 but often the orthodontist is called on to level teeth by selective vertical repositioning to establish a balanced and healthy bone level across associated teeth, particularly if they are intimately associated with restorative procedures (Fig. 24-12).18,19 These specific procedures may be incorporated into the biomechanical plan (Fig. 24-13).
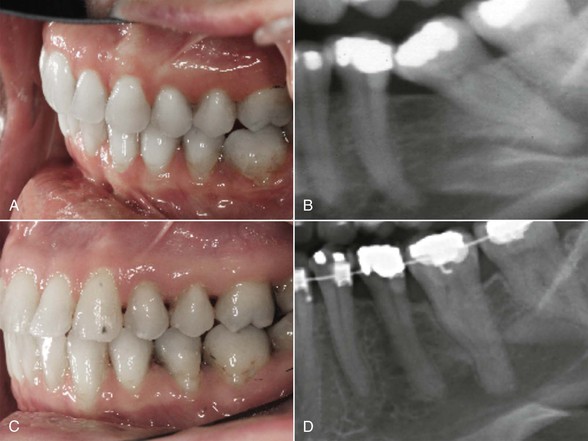
Figure 24-12 The orthodontist may assist in uprighting significantly tipped molars. A and B, A lower second molar tipped significantly due to earlier extraction of the lower first molar. A significant angular periodontal defect has developed. C and D, Uprighting of the molar improved the bony morphology and eliminated the angular bony defect.

Figure 24-13 An adult patient presented with a deep overbite and significant tooth wear. A and B, Pre-treatment intraoral photographs revealed significant loss of attachment on the lower central incisor. C, Management of the deep overbite involved lower incisor intrusion and proclination. A gingival graft was performed to cover the defect and thicken the gingiva prior to bonding of appliances and orthodontic treatment. D, The gingival graft was successful in covering the defect and contributed to a most satisfactory treatment outcome.
The periodontist may consider soft tissue augmentation procedures to prevent further breakdown of the gingival tissues either because the tissues are predisposed to recession by the dental history or because the tooth movement proposed by the interdisciplinary team may predispose the patient to further attachment loss (Fig. 24-14).22–27
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses