Clinical and Radiological Perspective
➧. Introduction, History and Relevance
➧. Challenges in Postmortem Examination
➧. Postmortem Alterations to Teeth and Oral Tissues
➧. Craniofacial Identification
Clinical Methods of Age Assessment
Radiographic Methods for Age Assessment
Estimating Age in Children and Adolescents
Third Molars in Age Estimation
Introduction, History and Relevance
Subsequently, intermittent cases of forensic dental identification in 19th century Europe and America have been reported (Pedersen, 1965). However, Gustafson (1962) believed that the role of forensic odontology in human identification came to prominence toward the end of the 19th century after two major fires in Europe: the first occurred in 1881 when the ‘Ring Theatre’ in Vienna was destroyed during a performance with 449 casualties; and the second— the Charity Bazaar fire in Paris in 1897—resulted in 127 deaths. In both tragedies, dental features were used for identification. According to Harvey (1973), one of the dentists who assisted the identifications in Paris was a Cuban named Oscar Amoedo. In 1898, he authored one of the first books on forensic odontology, L’art Dentaire en Medicine Legale, and is considered a pioneer of modern forensic dentistry. It is noteworthy that Yasutami Kojimahara of Japan had published a similar work titled Dental Jurisprudence a few years earlier in 1894 (Suzuki, 1996). The routine use of dental evidence in human identification gained impetus during the 1950s and 1960s, and forensic dentistry gained organized status in 1972 with the formation of the International Organization for Forensic OdontoStomatology (IOFOS).
Dental Identification
What is Identification?
Identity refers to the characteristics by which a person may be recognized (Acharya and Taylor, 2003) and identification is the establishment of a person’s individuality. Accurate identification of the dead is required both for legal and humanitarian reasons (Brown, 1984). It enables the settlement of insurance and property, permits remarriage of the surviving spouse and facilitate last rites of the body in accordance with appropriate religious customs. Haglund and Morton (1994) believe that a majority of individual identifications in forensic settings are nonproblematic since most individuals die in the company of family and friends. These deaths may occur at home or in a hospital, allowing visual identification. However, in cases where the body is burned, traumatized or decomposed, visual identification can prove unreliable. Hence, Sopher (1972) believes that visual recognition and use of personal effects are the least dependable methods of identification in such circumstances. Therefore, the safest option is for the forensic expert to analyze physical features present in the body.
Principle of Dental Identification
The underlying principle of dental identification is that combinations of dental characteristics are never the same in any two individuals. Several authors believe that the human dentition is unique (Johanson and Lindenstam, 1961; Keiser-Nielsen, 1977; Fellingham et al, 1984; Phillips and Scheepers, 1990). Human beings normally have 32 permanent teeth which vary in morphology and arrangement. Although teeth are relatively resistant to environmental factors and postmortem proteolysis, during life they are susceptible to disease such as caries. As a result, teeth may have undergone treatment in the form of fillings, crowns, etc. Those teeth that cannot be restored may have been extracted and, thus, missing from the oral cavity. According to Keiser-Nielsen (1977), the number of combinations 16 missing teeth can produce is approximately 60 crore. Sixteen filled teeth produce a similar combination. Four missing and four filled teeth combined can produce about 70 crore combinations. Every tooth has five surfaces and taking the 160 tooth surfaces individually would produce astronomical variations. In addition to the features visible on oral examination, radiographs reveal distinct shape and outline of various restorations of the crown and root and anatomic features of the teeth and bone (Sopher, 1972). Hence, the permutations resulting from observing the teeth clinically and radiographically would be phenomenal. It has been calculated that there are 1.8 × 1019 possible combinations of 32 teeth being intact, decayed, missing or filled (Fellingham et al, 1984). Therefore, dental identity can be considered as the sum total of all characteristics of teeth and associated structures which, while not individually unique, equal a unique totality (Acharya and Taylor, 2003).
Dental Identification Procedure
On-site evidence recovery
To begin with, it is essential to collect all dental evidence from the dead body (Haglund and Morton, 1994). This may require the dentist’s presence at the site where the dead body is recovered (Brown, 1984). Dental evidence present at the site where the body was found may be overlooked and not recovered—decomposition and skeletonization often leads to loosening of teeth and the anterior teeth, which have conical roots, may get dislodged. Oliveira and associates (2000) and Duric and coworkers (2004) have reported that incisors, especially maxillary, are most prone to getting lost postmortem. Incinerated bodies have fragile bones and teeth, which can easily be mishandled by an untrained individual; trauma may result in scattering of dental evidence around a large area. Acharya and Taylor (2003) have found that the inability to recover complete and intact postmortem dental data can undermine successful identification. Therefore, to maximize success, one must try to recover all dental evidence that may be present at the site. Hence, care must be taken to document and photograph the scene at which the body is recovered; a forensic odontologist should be present to ensure proper search and recovery of all material of dental significance needed for identification.
Postmortem dental examination and radiography
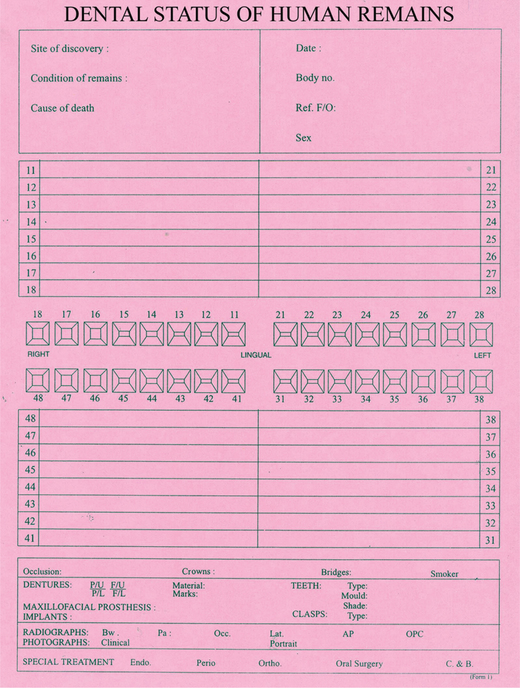
The postmortem dental examination is usually conducted in a mortuary. Case numbers allotted to the body should be verified and entered in the modified Interpol postmortem dental odontograph, also referred to as the ‘pink form’ (Figure 1) before the commencement of examination. A visual appraisal of the body may enable preliminary assessment of the ethnicity, gender and approximate age of the victim. The body bag used to transport the deceased should be thoroughly searched for dislodged teeth or dental appliances. Postmortem dental examination is similar to routine examination of the oral cavity. All oral and dental features, including intact and missing teeth, caries and other pathology, restorations, attrited and rotated teeth should be carefully charted on the postmortem form. This will be the basis for later comparison and verification. Brown (1984) suggests that postmortem examination should be undertaken by dentists working in pairs—one examining and the other recording. The roles are then reversed and the procedure repeated ‘as an added check’. Any dental evidence missing should be reported to the forensic pathologist or accompanying law enforcement personnel. Subsequent dental evidence recovered must be labeled properly.
The dental examination must be complemented with postmortem dental radiography as this will reveal what cannot be observed clinically. Radiographic films may be stabilized in the mouth using readily available materials such as gauze or cotton rolls. Whenever possible, postmortem radiographs should be taken to replicate the type and angle of the antemortem radiographs (Goldstein et al, 1998). According to these authors, if the difference in horizontal angulation between the ante- and postmortem radiographs is more than 10°, comparison will not facilitate identification. However, changes in the vertical angulation or the focal point-film distance do not affect the outcome of comparison. Pretty and Sweet (2001) have suggested that ante- and postmortem radiographs could be marked using a rubber-dam punch to differentiate the two—‘one hole for antemortem films and two holes for postmortem films’. The exposure time may need to be increased or decreased respectively in bloated bodies recovered following drowning and in skeletal remains.
Obtaining dental records
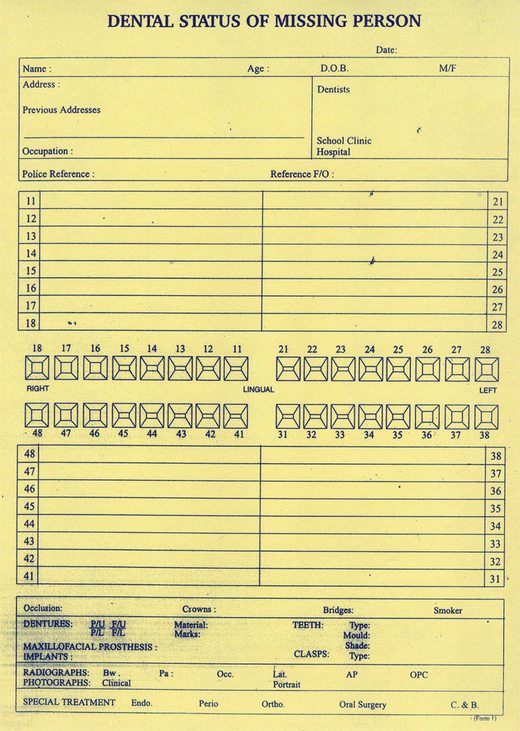
Dental records contain information on treatment and dental status of a person during life. These antemortem records can be obtained from the local dentist, specialist or hospital records. Whenever possible, the original records should be examined. Records include hand-written dental charts, radiographs, study casts and photographs. An individual may have visited more than one dentist for therapy and multiple dental records may exist. Relevant information from the dental records should be transcribed onto the modified Interpol antemortem odontograph (the ‘yellow form’) (Figure 2).
Contribution of dental records in successful identification depends on the availability of original records, their completeness and quality (Acharya and Taylor, 2003). By maintaining good dental records, dentists reflect their awareness and responsibility to forensic identification (note: quality dental records are also important as a counter to malpractice lawsuits). It is also important that these records are relatively recent—records made for a 6-year-old child may not be useful 20 years later in adulthood.
Identification report and conclusion
Subject to the availability of adequate postmortem data and quality antemortem records, Haglund and Morton (1994) have stated that ‘the comparison and eventual dental identification are straightforward and routine’. These authors believe that the quality and quantity of information required for establishing positive dental identification has not been established. In fingerprinting, differences in the ante- and postmortem data rule out a positive match. This concept, however, does not apply to dental identification as long as the inconsistencies are explainable. For example, the postmortem data may reveal a restoration on a tooth but the dental records indicate that the same tooth is intact. This difference, however, can be explained since the restoration may have been placed on a date after the last available dental record. On the other hand, if the postmortem data shows an intact tooth but the same tooth is indicated as being restored in the dental record, this would probably suggest a mismatch. Having compared the ante- and postmortem data, one should address whether the similarities are significant and the differences can be explained. Based on this, a range of conclusions can be reached which have been modified below from McKenna (1986), Silverstein (1995) and Acharya and Taylor (2003).
Excludes identity
The ante- and postmortem data are clearly inconsistent; the data contain unexplainable differences that comprehensively indicate a mismatch.
Digital radiography in dental identification
Traditional methods of radiography involve the use of film. The advent of digital radiography over the past decade, which replaces the radiographic film with an image capturing sensor, presents certain advantages to forensic investigation. Since the images can be viewed immediately after exposure, the operator has the choice to either accept or reject the image depending on its quality. Further, postmortem images may be retaken to replicate the antemortem radiographic position and angulation. This could be particularly relevant in postmortem settings where access to radiographic processing may be unavailable or the ability to retake the radiographs of the decedent at a future date is unlikely. Hanaoka and colleagues (2001) have successfully used the technology in postmortem dental identification and predicted its routine application in the future. They have stated that receiving, sending and storing digital radiographs through computer networks is effortless. According to Hubar and Carr (1999) and Du Chesne and associates (1999), the radiographic image may be enlarged, rotated and its brightness and contrast modified. Several images may be viewed together which allow convenient comparison of ante- and postmortem images. ‘Subtle features difficult to visualize on conventional radiographs such as trabecular bone patterns are seen with greater detail digitally and may further help to corroborate identification of a decedent’ (Hubar and Carr, 1999). However, manipulations which distort the structures visible on the radiograph by changing their angular relationship are not admissible by the courts of law (Du Chesne et al, 1999). Hence, these authors have stated that it must not be the objective of postmortem radiology to manipulate the images ‘to such an extent that optimal or even misleading results are presented’. While it is reasonable to expect forensic experts to avoid such alterations on postmortem radiographs, one cannot be so sure about antemortem digital images. Therefore, the conclusions based on comparison of post- and antemortem digital radiographs may be brought into question by the courts of law, which will probably give greater weight to documentary evidence such as conventional radiographic films than electronic data files.
Challenges in Postmortem Examination
Rigor Mortis
Limited opening of the mouth due to severe postmortem rigor will affect dental examination since access to the oral cavity is limited and viewing the dentition is impaired. In such cases, where the muscles are extremely rigid, the mouth will have to be forced open. The use of trismus screws (made from acrylic) for obtaining initial opening in the anterior dentition followed by Fergusson or Heister mouth gags to increase jaw separation at the posterior region has proven useful in the author’s experience. However, one must be careful not to fracture the teeth. Nakayama and coworkers (2001) have advocated an intraoral approach for myotomy of the temporalis muscle. They contend that mouth opening demands relaxation of the temporalis and, hence, its myotomy will facilitate easy dental examination. Their method prescribes an intraoral incision to expose the coronoid process followed by the insertion of a curved Cooper type scissors through the incision to dissect temporalis fibers that are inserted to the top of the coronoid process (Figure 3A, B). The deep fibers, which may also insert to the mandibular notch, are drawn forward with a channel retractor for dissection (Figure 3C, D). The myotomy is carried out on both the left and right sides.
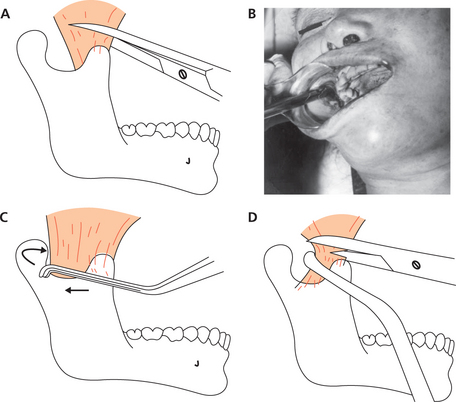
Figure 3 (A, B) Intraoral approach for myotomy: when the temporalis is attached to the top of the coronoid process, myotomy is accomplished with scissors only; (C, D) in case the temporalis is attached both to the coronoid and mandibular notch, a channel retractor is inserted to draw forward the deep end of the muscle to facilitate dissection. (Reprinted from Nakayama Y, Aoki Y, Niitsu H, et al (2001), ‘Forced oral opening for cadavers with rigor mortis: two approaches for the myotomy on the temporal muscles’, Forensic Science International, Vol. 118, pp. 37–42, with permission from Elsevier)
Jaw Resection
Depending on the circumstances of death and condition of the body, the forensic dentist can decide to cut open the soft tissue of the cheek to reach the teeth, or remove the jaws entirely. Resected jaws are easier to examine and radiograph. However, such ‘invasive’ procedures can pose obstacles, especially when the body needs to be viewed by relatives. Furthermore ethical and legal hurdles may be faced. Therefore, one must consider jaw resection as a last option and obtain prior permission from the forensic pathologist.
Postmortem Alterations to the Teeth and Oral Tissues
Incinerated Teeth
Crown
Initial separation of enamel from dentin occurs at 400°C and the enamel shell separates totally at 450°C. At 500°C, Harsányi (1975) has observed deep longitudinal furrows on the crown which almost divide it into several pieces. At this temperature, the pulp chamber and root canal are preserved and not narrowed. Above 500°C, the crown undergoes fragmentation and consistently becomes smaller with further rise in temperature. The narrowed cavities of the pulp chamber and root canal are recognizable even at 1,100°C.
The coronal dentin is exposed at 450°C (following total separation of the enamel shell). Cracks appear at 600°C with disintegration from 800°C onward. While enamel is converted to powder, dentin is not. This has been attributed to hypermineralized pretubular zone of the dentin. Myers and colleagues (1999) believe that the mineral content of dentin, located within its organic matrix composed of type I collagen, helps stabilize the collagen against thermal denaturation and shrinkage. The color changes in the crown and root at different temperatures has been demonstrated by Muller and associates (1998) (Table 1). However, these authors have cautioned that in real-life scenarios, it may be much more difficult to observe the color changes since teeth found at the site of fire need to be carefully cleaned. They added that ‘the presence of a superficial metallic layer, resulting from the dry distillation of organic matter, can lead to observational errors’.
Table 1
| Temperature (°C) | Appearance | |
| 150 | Crown | Normal color and shiny appearance |
| Root | Off-white to light yellow | |
| 200 | Crown | Dull, light brown surface |
| 300 | Crown | Light brown to grayish with dark brown spots |
| Root | Black | |
| 400 | Crown | Dark brown/gray |
| Root | Shiny black | |
| 500 | Crown | Enamel is dark brown or gray; dentin is gray |
| Root | Gray/brown | |
| 600 | Crown | Dark gray enamel and blue-tinted gray dentin |
| Root | Blue-tinted gray with white spots | |
| 700 | Crown | Dark gray enamel and blue-tinted white dentin; the cusp tips are blue |
| Root | Blue-tinted white or white only | |
| 800 | Crown | Dark gray enamel with white spots; white dentin |
| Root | White with gray spots | |
| 900 | Crown | White dentin |
| Root | White with dark gray or black spots at CEJ | |
| 1,000 | Crown | White dentin |
| Root | White with pink tinge at apex | |
| 1,100 | Crown | Chalky white |
| Root | Chalky white | |
| 1,150 | Crown |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses