CHAPTER 23 THE EVOLUTION OF THE ANGLED IMPLANT
 The Pterygoid/Tuberosity Implant
The Pterygoid/Tuberosity Implant
The first use of an implant placed in the pterygo-maxillary region was documented by Dr. Tulasne at the suggestion of Dr. Paul Tessier in 1985,1 only 3 years after the introduction of the concept of osseointegration to North American practitioners at the Toronto Conference in 1982. By necessity, these implants needed to be angled toward the anterior part of the mouth for access and to create the greatest possible length of implant-bone contact.
Successful placement of an implant in this area requires a volume of bone in the tuberosity region that will accommodate an implant without fenestration laterally. Due to the angulation of placement, however, it is not uncommon to have an implant length capability of 13-15 mm. There are even variants of this procedure using engagement of the sphenoid bone, through a guided approach, that allow placement of implants 20 mm or longer.2
Indications
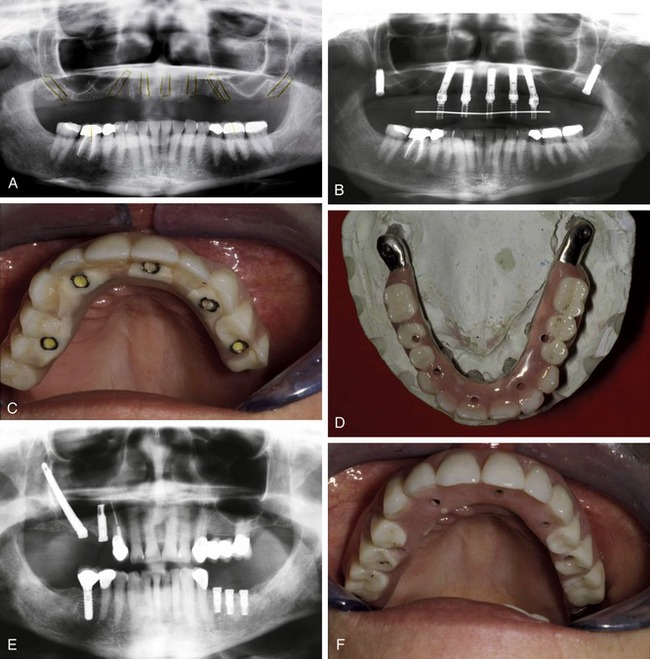
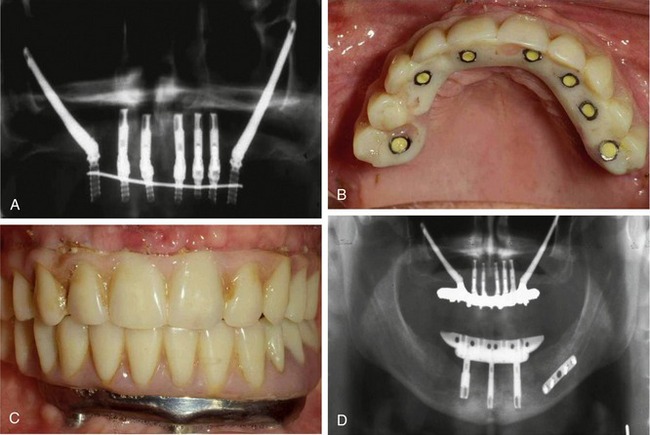
The pterygoid implant generally is used where posterior support for a full-arch prosthesis beyond the first molar is required. The placement of dentition in the area of emergence of this implant is seldom required, but the additional support gained with a beam extension can eliminate cantilever stresses that can be difficult to counter when opposing second molar occlusion is present (Figure 23-1).
This is generally a niche concept, but one that can be very valuable in prosthesis design and construction when additional cantilever support is necessary. As seen in the existing literature specific to the pterygoid approach, there are reported rates of implant success varying from the 92.7% initially seen by Tulasne to between 67% and 93% success in more recent papers.3–8 Although probably not considered a mainstream approach due to a lack of universal application, it is still valuable in specifically indicated situations. When tuberosity bone is available, the use of the pterygoid implant may eliminate the necessity for sinus grafting, which is often a desirable option if the preference of the patient is to avoid a graft approach.
 The Zygoma Implant
The Zygoma Implant
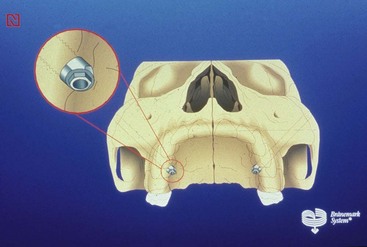
The original design was a stepped, straight, hex-head implant that varied in available lengths up to 50 mm (Figure 23-2). The zygoma implant, as currently used, has an oxide enhanced surface and a premachined 45 degree angled head for improved screw access intraorally (Figure 23-3). The concept is to engage the zygomatic buttress with 11-13 mm of osseointegrated surface apically, and, after passing through the sinus, engage the alveolar and palatal bone in the first molar area coronally. Once integrated, the zygoma implant can provide significant distal support for a variety of clinical applications due to the length and strength of the fixture itself. As with the pterygoid approach, the need for sinus grafting to gain osseous volume and distal implant positioning is often eliminated.9–16
Indications
Cancer
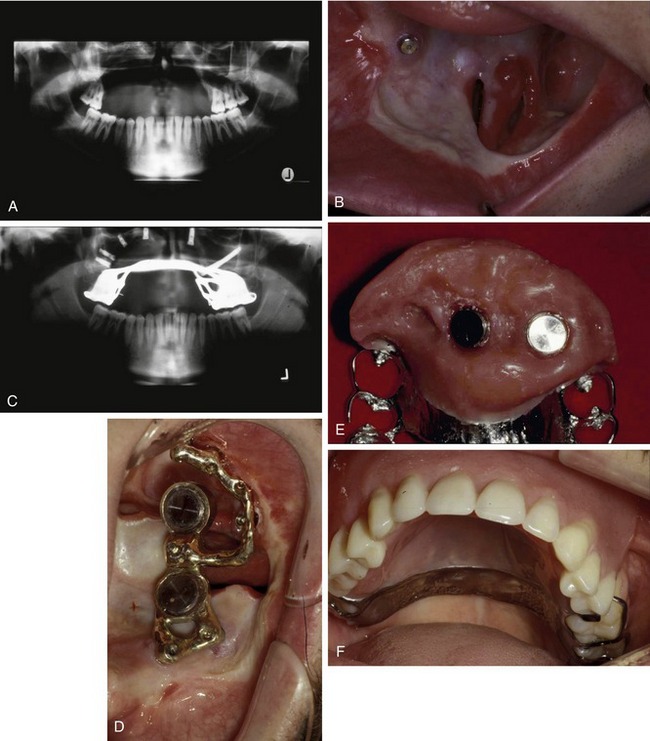
In situations of severe injury or ablative cancer surgery, the zygoma implant can play a critical role in creating a retentive base for prosthesis construction. In many presentations, these patients have minimal or no available alveolar bone, and thus are severely compromised in normal eating or speaking activities. Originally, restorations created before implant availability were only marginally successful, and were dramatically challenged in terms of retention and defect obturation.17–19
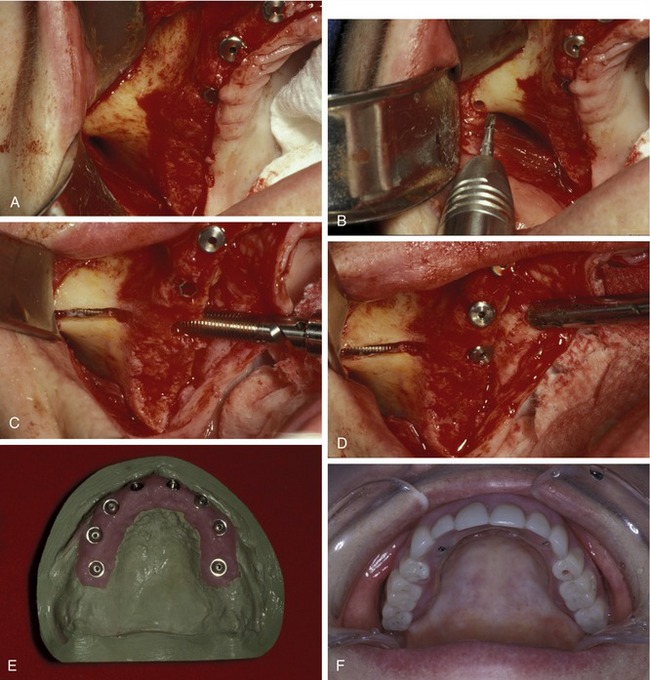
Many oral cancer defects involve the removal of large portions of the alveolus and basal bone, creating a large fistula or communication with the maxillary sinus and associated structures (Figure 23-4, A and B). In such cases, the only available bone in the defect area is in the nasal rim, which is usually very thin, and remotely in the zygomatic buttress. The zygoma implant, in combination with conventional implants placed in any available bone sites, can often provide the basis for a retentive bar structure at the alveolar level (Figure 23-4, C and D). The obturating prosthesis can then be based entirely on the bar structure or on the bar in combination with residual dentition. The resultant restoration will then be resistant to vertical dislodgement in both the superior and inferior directions, and can provide the stability and seal to obturate the defect space effectively (Figure 23-4, E and F).
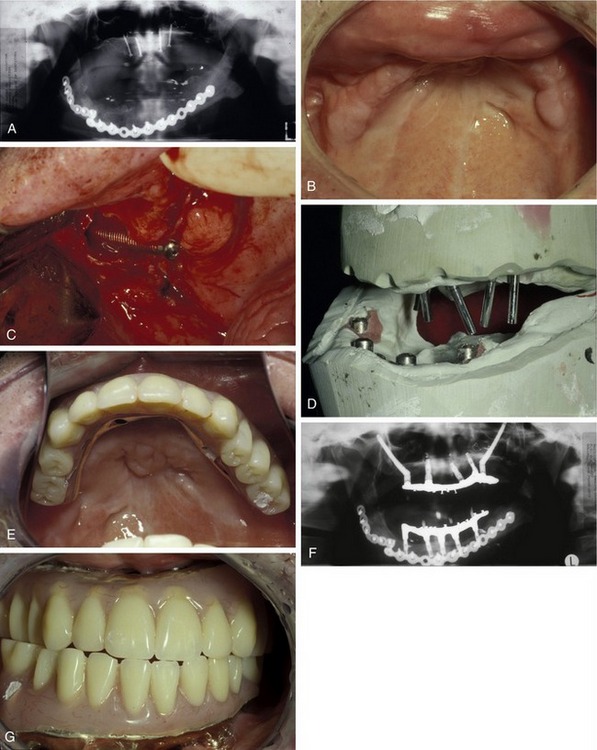
Trauma
Defects of the maxilla from trauma may be similarly challenging with regard to creating prosthesis retention and may vary dramatically in topographical presentation, depending on the nature and severity of the injury. The relative capacity provided by the zygoma implant in these situations is equally valuable for prosthesis construction, even in the near absence of normal tissue position or relationships (Figure 23-5).
Severe Atrophy
Patients who have lost maxillary bone through atrophy to the point where no receptor sites for implants are present may be facing large grafting procedures to rebuild the maxilla. Although this onlay or interpositional approach can eventually provide adequate and usable bone, the grafting process is lengthy, requires recovery from a significant (hip) donor site entry, and may not allow for the use of a maxillary prosthesis of any kind during both the graft healing and implant integration phases. The success rate of implants in these reconstructed sites is also variable and much less predictable than implants placed entirely in host bone.16
The use of zygoma implants in pairs bilaterally (the quad approach) has proven to be valuable in treating these severely atrophic maxillae. By spacing the emergence points through tissue with an anterior/posterior spread, a cross-arch stabilizing effect can be created by the final, or interim, prosthesis. There are fewer limitations on using an aesthetic interior full denture with this technique, as long as indirect transmucosal loading is avoided in the prosthesis design. The single greatest benefit, especially from the patient’s perspective, is the avoidance of a major graft procedure.20,21 A more detailed description of the quad approach with the most current applications of this technology can be found in Chapters 15 and 27.
Immediate Loading
One of the factors that most influences the ability to immediately load a maxillary full-arch implant restoration is the strength of the two distal fixtures. Before the advent of a tilted, or angled, approach, almost all maxillary implants were vertically aligned. As the most distal implants approached the maxillary sinus area, the amount of available bone diminished dramatically, thus reducing the vertical space available for this pair of critical supporting elements. Given the documented poor success of short vertical distal implants (7 and 10 mm) adjacent to the anterior sinus wall, many clinicians were hesitant to attempt loading immediately.22–25 The use of a long and stronger implant in these sites, as the zygoma, created an improved support potential at the cantilever junction and an increased potential for implant integration during the provisional phase (Figure 23-6). Favorable reports on the immediate loading of zygoma/standard implant combinations have shown that this can be a viable approach.
Modifications
A modification in surgical technique suggested by Stella and Warner allowed the zygoma implant to realign against the vertical maxillary buttress, and exit more centrally on the ridge crest of the maxilla. This approach is also less invasive to the sinus and, therefore, allows more implant body contact with bone (Figure 23-7).26
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses