CHAPTER 23 Dental Problems of Children with Special Health Care Needs
Approximately 52 million children and adults in the United States have a disabling condition.1 The American Academy of Pediatric Dentistry defines individuals with special health care needs (SHCN) as those with “any physical, developmental, mental, sensory, behavioral, cognitive, or emotional impairment or limiting condition that requires medical management, health care intervention, and/or use of specialized services or programs.”2 Patients with SHCN are at increased risk for oral disease.3
Many children with SHCN are best managed initially by a multidisciplinary team in which a dentist is available to evaluate extraoral and intraoral findings of the child. A diagnosis is then established, and an impression is gained of the child’s strengths and weaknesses and the team’s recommendations for future care. The child may then be “mainstreamed” to a dental practitioner whom the family chooses, if a preference is indicated. The team is available to help the family practitioner or pediatric dentist treat the child and prepare the family for the child’s future treatment needs because oral health is a vital part of the child’s well being and general health.3
Children with SHCN may present challenges that require special preparation before the dentist and office staff can provide acceptable care. In addition, parental anxiety concerning the problems associated with a child’s SHCN frequently delays dental care until significant oral disease has developed. Also, some dentists feel uncomfortable providing treatment for children with SHCN, which results in a loss of greatly needed services. Kane and colleagues reported failure to obtain routine medical care as well as income below 400% of federal poverty guidelines as a barrier to receipt of dental care for children with SHCN.4 Financing and reimbursement issues are other barriers for families with SHCN children and for dental practitioners.5 Nonfinancial barriers such as language and psychosocial, structural, and cultural considerations also interfere with access to oral care.5
DENTAL ACCESS
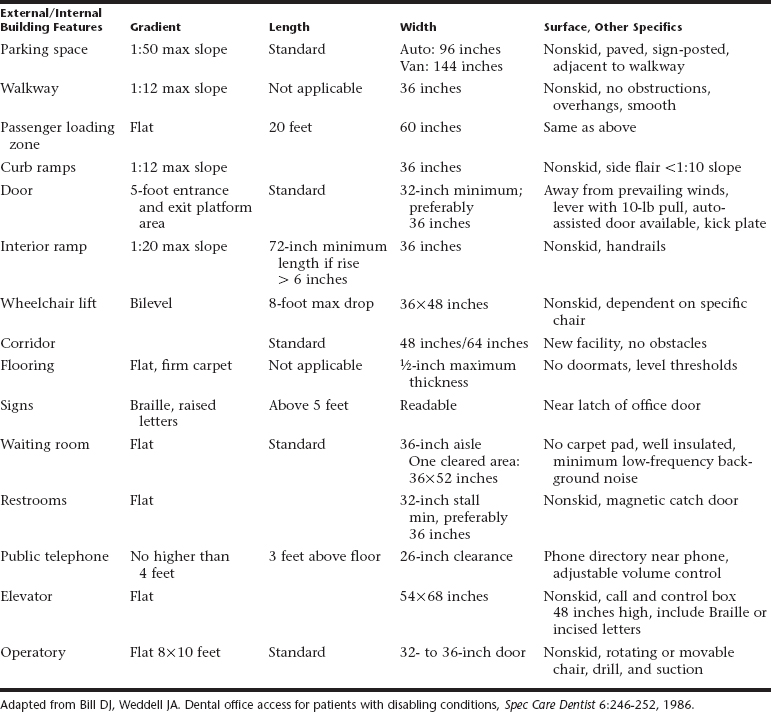
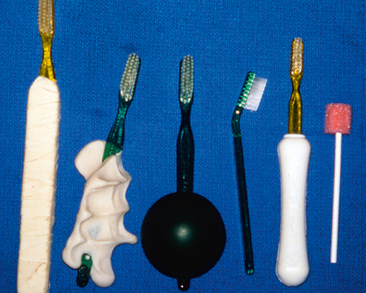
The rapid expansion of the elderly population, the presence of children with SHCN, and the emergence of legislative guidelines for people of all ages with SHCN are three important factors that should prompt dentists to address cost-efficient ways to make their office facilities and operatory areas accessible for persons with SHCN. In August 1984, another federal-level cornerstone was laid for barrier-free facility access with the passage of the Uniform Federal Accessibility Standards.6 Enacted in 1990, the Americans with Disabilities Act defines the dental office as a place of public accommodation.7 Dental consumer populations are becoming more sensitive to the service needs and desires of people with SHCN by improving family conditions and public education. Failure to accommodate SHCN patients could be considered discrimination and a violation of state or federal law. Table 23-1 lists common minimum requirements needed to gain access.
In the dental operatory, doorways should be 4 inches (10 cm) wider than normal. In the dental suite where floor circulation space is at a premium, aisle passage in the operatory area should be planned with the dimensions shown in Fig. 23-1. The required wheelchair turning space and top space under furniture and fixtures may be more readily accommodated if one operatory is specifically designed with a movable dental chair, instrument control unit, and suction system. Movable equipment should enhance the opportunity to back the patient’s wheelchair into the operatory and thus reduce the need for more wheelchair turning space. If possible, a wider radius for turning space is desirable to accommodate wheelchair extensions and adaptations that are required for some persons. Dental chairs should be adjustable for height to match different wheelchair designs.
FIRST DENTAL VISIT
Many people avoid dental treatment for themselves or their children because of their fear that dental visits are routinely painful. Dental professionals should use every opportunity to help patients or parents overcome this barrier into the mainstream of effective dental care and establish a “dental home” with them (see Chapter 1).
Upon scheduling an appointment, the dental receptionist should determine the presence and nature of any SHCN, should determine who the family’s medical provider is, and should alert the dentist so adequate time can be allowed. The initial dental examination for a child with SHCN is like the initial examination described in Chapter 1. Special attention should be given to obtaining a thorough medical and dental history. The names and addresses of medical or dental personnel who have previously treated the patient are necessary for consultation purposes. Consultation with these specialists is common and helps provide insight in case management, planning, and avoiding unwanted outcomes. Health Insurance Portability and Accountability Act compliance is mandatory throughout this process.
RADIOGRAPHIC EXAMINATION
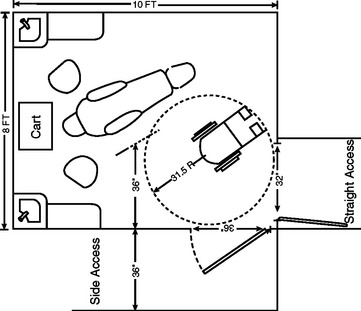
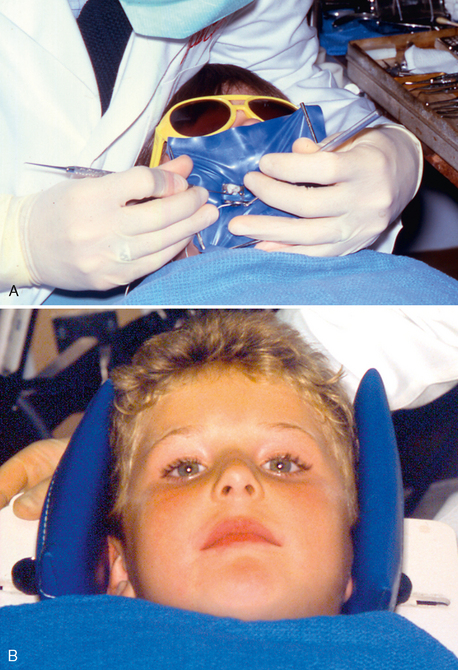
For patients with limited ability to control film position, intraoral films with bite-wing tabs are used for all bite-wing and periapical radiographs. An 18-inch (46-cm) length of floss is attached through a hole made in the tab, as shown in Fig. 23-2, to facilitate retrieval of the film if it falls toward the pharynx. Digital sensors can be cumbersome. Regar dless of the types of radiographs to be made, the patient should wear a lead apron with a thyroid shield, and anyone who helps hold the patient and the film or sensor steady should wear a lead-lined apron and gloves (Fig. 23-3).
PREVENTIVE DENTISTRY
Preventing oral disease before it starts is the most desirable way of ensuring good dental health for any dental patient. An effective preventive dentistry program is important for a child with SHCN because of the predisposing factors that make restorative dental care harder to obtain when it is necessary. Dental diagnosis and treatment planning will necessitate an accurate, up-to-date medical history at each visit. After the diagnosis, the dentist should determine the patient’s needs, assume the responsibility for formulating an individual program for the child, and adequately communicate to the parents and patient how such a program can be effected. Use of a Caries-Risk Assessment Tool (CAT) to integrate these dental risk factors may result in a more aggressive approach to the individual’s dental treatment plan. A clear perception of the situation by everyone involved is essential for a successful preventive program; adequate communication is vital.
HOME DENTAL CARE
Home dental care should begin in infancy; the dentist should teach the parents to gently cleanse the incisors daily with a soft cloth or an infant toothbrush. For older children who are unwilling or physically unable to cooperate, the dentist should teach the parent or guardian to clean teeth twice a day using correct toothbrushing techniques, safely immobilizing the child when necessary. Figure 23-4 shows several positions for toothbrushing that permit firm control and support of the child, adequate visibility, and convenient positioning of the adult, with reasonable comfort for both adult and child (also see Fig. 11-14). Positions most commonly used for children requiring oral care assistance are as follows:
Some parents and health centers have encouraged children with SHCN to assume the responsibility for their own oral hygiene, but the results are usually poor. Although independent brushing is not contraindicated, parents and staff should be aware that, without their follow-up, unsupervised oral hygiene procedures in children with SHCN can have serious dental consequences. The amount of supervision and assistance provided by the parents or staff should depend on the child’s willingness to cooperate and ability to maintain good oral hygiene twice a day.
A plaque control program is essential in monitoring oral hygiene in the child with SHCN and determining the level of success achieved by each patient. The brushing technique for patients with SHCN who have fine or gross motor deficiencies limiting their ability to brush should be effective and yet simple for the person performing the brushing. One technique often recommended is the horizontal scrub method because it is easy to perform and can yield good results. This technique consists of performing gentle horizontal strokes on cheek, tongue, and biting surfaces of all teeth and gums. Other patients with SHCN without such motor problems can use age-appropriate techniques previously discussed in Chapter 11. A soft, multitufted nylon brush should be used.
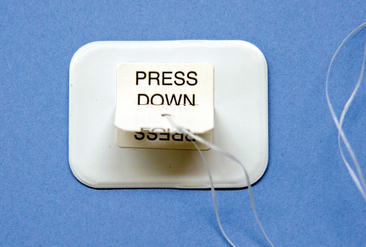
Figure 23-5 illustrates some modifications that may be made to a toothbrush to help persons with poor fine motor skills improve their brushing techniques. Although many types of grips are available, using the patient’s hand to custom-design a handle has often had good results (Fig. 23-6). Electric toothbrushes have also been used effectively by children with SHCN. The vibration and noise tend to desensitize the patient for future dental appointments if followed by positive reinforcement while the design and color is motivational for the child. Daily flossing, with supervision or the use of floss holders, is essential to maintain optimal gingival health.
DIET AND NUTRITION
Diet and nutrition influence dental caries by affecting the type and virulence of the microorganisms in dental plaque, the resistance of teeth and supporting structures, and the properties of saliva in the oral cavity. A proper noncariogenic diet, as outlined in Chapter 12, is essential to a good preventive program for a child with SHCN. As discussed in Chapter 10, one should assess the diet by reviewing answers on a diet survey with the parent, realizing that allowances must be made for certain conditions for which dietary modifications are required. For example, conditions associated with difficulty in swallowing, such as severe cerebral palsy, may require that the patient be on a pureed diet. Patients with certain metabolic disturbances or syndromes, such as phenylketonuria, diabetes, or Prader-Willi syndrome, have diets that restrict specific foods or total caloric consumption. Whatever the special circumstances, any dietary recommendations should be made individually after proper consultation with the patient’s primary physician or dietitian. The oral side effects of their medications should be reviewed with the parents or guardians at each visit to identify specific concerns, for example, of increased caries or gingival overgrowth, to prevent or minimize these problems. Particular emphasis should be placed on discontinuation of the nursing bottle by 12 months of age and cessation of at-will breast-feeding after teeth begin to erupt to decrease the likelihood of early childhood caries.
FLUORIDE EXPOSURE
The judicious use of systemic fluoride is important in the comprehensive management of any dental patient. Special emphasis should be placed on ensuring adequate systemic fluoride for patients with disabilities. The dentist should first determine the concentration of fluoride in the patient’s daily water supply. If the level of fluoride is between 0.7 and 1 ppm, no supplementation is normally required. If the dentist is not sure of the fluoride level of the patient’s drinking water or other sources, an analysis to determine the level is indicated. Once the level has been documented, a determination of the need for fluoride supplementation can be made. The amount of systemic fluoride supplementation necessary, along with the various forms available (i.e., drops, tablets, and rinses), is outlined in Chapter 10.
Whether the patient lives in an area with a fluoridated or nonfluoridated water supply, a topical fluoride should be applied after a regularly scheduled professional prophylaxis. Also, 5% neutral sodium fluoride varnishes have been shown to be beneficial.8 An American Dental Association–accepted dentifrice containing a therapeutic fluoride compound should also be used daily. Some clinicians treating patients with SHCN who have chronically poor oral hygiene and high decay rates suggest a daily regimen of rinsing with 0.05% sodium fluoride solution. Nightly application of a 0.4% stannous fluoride or 1.1% sodium fluoride brush-on gel has also been successfully used to decrease caries in children.
MANAGEMENT OF A CHILD WITH SPECIAL HEALTH CARE NEEDS DURING DENTAL TREATMENT
The principles of behavior management discussed in Chapter 3 are even more important in treating a child with SHCN. Because hospital visits or previous appointments with a physician frequently result in the development of apprehension in the patient, additional time must be spent with the parent and the child to establish rapport and dispel the child’s anxiety. If patient cooperation cannot be obtained, the dentist must consider alternatives such as protective stabilization, conscious sedation, or general anesthesia to allow performance of the necessary dental procedures.
PROTECTIVE STABILIZATION
The American Academy of Pediatric Dentistry’s Behavior Guidance for the Pediatric Dental Patient Reference Manual 2008-09 indicates that the need to diagnose and treat, as well as to protect the safety of the patient, parent, staff and practitioner, must justify the use of stabilization.9 This decision should take into consideration a careful review of the patient’s emotional development, physical and medical conditions (e.g., asthma-compromised respiratory function), dental needs, other alternative behavioral modalities, and quality of dental care. Although the benefits and importance of protective stabilization have been documented, the use of behavioral management or sedation, as discussed in Chapter 14, can reduce the amount of stabilization required. This is only one means of behavior control to achieve an adequate level of dental treatment.
The use of protective stabilization is indicated in the following situations:
The use of stabilization is contraindicated in the following situations:
Common mechanical aids for maintaining the mouth in an open position are shown in Fig. 23-7. Padded and wrapped tongue blades are easy to use, disposable, and inexpensive. Frequently, parents of a child with disabilities are given wrapped tongue blades or Open Wide (Specialized Care Co., Hampton, NH) disposable mouth props to aid with home dental care. The Open Wide mouth prop has a durable foam core on the end of a tongue depressor. It is also easy to use, disposable, and available in two sizes, but it is slightly more expensive than wrapped tongue blades. The Molt Mouth Prop (Hu-Friedy, Chicago, Ill) can be very helpful in the management of a difficult patient for a prolonged period. It is made in both adult and child sizes, allows accessibility to the opposite side of the mouth, and operates on a reverse scissors action. Its disadvantages include the possibility of lip and palatal lacerations and luxation of teeth if it is not used correctly. Caution must be exercised to prevent injury to the patient, and the prop should not be allowed to rest on anterior teeth. The patient’s mouth should not be forced beyond its natural limits because patient discomfort and panic will result, which will cause further resistance and perhaps airway compromise.
Body control is gained through a variety of methods and techniques. For children who have a severe intellectual disability or very young, parents and dental assistants can assist in the control of movements during dental procedures, as shown in Fig. 23-8. Usually, however, for a child who has severe intellectual disability, better working conditions and a more predictable patient response are obtained through the combined use of psychological management techniques, parental assistance, pharmacologic aids, and stabilization.
The following are commonly used for protective stabilization:
The Papoose Board (Fig. 23-9) has several advantages. Simple to store and use, it is available in sizes to hold both large and small children. It has attached head stabilizers and is reusable. It does not always fit the contours of a dental chair, however, and sometimes a supporting pillow is needed. Because it covers the patient’s diaphragm, a pretracheal stethoscope is necessary to monitor respiration if it is used in combination with sedation. An extremely resistant patient may develop hyperthermia if immobilized too long, and, of course, any restrained patient requires constant attendance and supervision.
Mink10 describes the bedsheet (triangular sheet) technique and its use in controlling an extremely resistant child (Fig. 23-10A). This economical method allows the patient to sit upright during radiographic examinations. Its disadvantages include the frequent need for straps to maintain the patient’s position in the chair, the difficulty of its use with small patients, and the possibility of airway impingement if the patient slips downward unnoticed. Hyperthermia may be another problem during long periods of stabilization. Again, the need for constant supervision is emphasized so that these problems may be avoided.
The Rainbow Stabilizing System or “Pedi-Wrap” (Specialized Care Co., Hampton, NH; see Fig. 23-10B), which is available with or without the backboard, also comes in various sizes and allows some movement while still confining the patient. Its mesh fabric permits better ventilation, lessening the chances of the patient developing hyperthermia. It, too, requires straps to maintain body position in the dental chair and constant supervision to prevent the patient from rolling out of the chair.
The beanbag dental chair insert was developed to help comfortably accommodate hypotonic and severely spastic persons who need more support and less stabilization in a dental environment (see Fig. 23-10C). It is reusable and washable, and one size fits most people. Many patients with SHCN relax more in this setting.
The child’s arms and legs can be stabilized with help from the parent or the dental assistant, with Posey straps, or with a towel and adhesive tape (Fig. 23-11). If movement of the extremities is the only problem, having a dental assistant stabilize the child is very helpful. Posey straps fasten to the arms of the dental chair and allow limited movement of the patient’s forearm and hand. This limited movement frequently prevents overaction by resistant or combative patients. Wrapping a towel wrapped around the patient’s forearms and fastening it with adhesive tape (without impeding circulation) is often helpful for an athetoid-spastic cerebral palsy patient who tries desperately, but without success, to control body movements. Protective stabilization actually encourages relaxation and prevents undesired reflexes by keeping the patient’s arms in the midline of the body.
A patient’s head position can usually be successfully maintained through the use of forearm-body pressure by the dentist. Other options include presence of an additional assistant to stabilize the child’s head or use of a Papoose Board head positioner or a plastic bowl (doggie bowl) to provide position guidance (Fig. 23-12).
An explanation of the benefits of protective stabilization should be presented by the dentist before used if communication with the patient is possible. The mouth prop can be identified as a “tooth chair,” the Pedi-Wrap as a “safety robe,” and a stabilization strap as a “safety belt,” which allows the patient to feel secure rather than threatened. The parents should be given a careful explanation about how protective stabilization allows the needed dental work to be done while minimizing the possibility of accidental injury to the patient, parent, staff, or dentist. If a child requires extensive dental treatment and cooperation cannot be achieved by routine psychological, physical, or pharmacologic measures, the use of general anesthesia in a controlled atmosphere, as discussed in Chapter 15, is recommended.
INTELLECTUAL DISABILITY
Intellectual disability is a general term used when an individual’s intellectual development is significantly lower than average and his or her ability to adapt to the environment is consequently limited.11 The condition varies in severity and cause. A classification of intellectual disability is presented in Table 23-2. Intellectual disability has been identified in approximately 3% of the U.S. population. For many years the potential abilities of people with intellectual disabilities were poorly understood, and such individuals were often treated as inferior. They were described using the terms idiot (IQ [intelligence quotient] below 25), imbecile (IQ of 25 to 50), and moron (IQ of 50 to 70). With the formation of the President’s Committee on Mental Retardation in 1968, emphasis was placed on education of individuals with intellectual disabilities to increase their social and civic responsibilities, motor skills, and independence within society.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses