Chapter 23 Cements
Section A Contemporary Dental Cements
Relevance to Esthetic Dentistry
In the past (and still), the term “permanent cement” has been used to describe the use of a cement for final, definitive cementation of indirectly placed laboratory-fabricated restorations. Unfortunately the term as it relates to restorative procedures is inaccurate and gives patients a false sense of security and expectation. In the future of fixed prosthodontics, cementation in restorative dentistry should focus on the placement-cementation so that the restoration cannot be removed later. Currently, a more proper term for cementation is “definitive cementation.”1
Relating Function and Esthetics
Clinical Considerations
Other factors are equally as vital as the selection of cement type for clinical success. For example, during the laboratory fabrication of cast and ceramic restorations, some steps can lead to marginal discrepancies and gaps between the restoration and tooth preparation. Today’s contemporary cements provide excellent marginal integrity to compensate for these discrepancies.2–5 An inherent aspect of retention is the taper of the tooth preparation with different cements.6 Zidan and Ferguson6 found that the retentive values of the adhesive resin cements for a tooth preparation with a 24-degree taper were 20% higher than the retentive values of the conventional cements (zinc phosphate and conventional glass ionomer) for a tooth preparation at a 6-degree taper. The use of resin luting agents yielded retention values double those of zinc phosphate or conventional glass ionomer cement. The type of bur or diamond rotary instrument used to prepare for crowns can also affect the retention of a crown placed with different cements.7
A significant issue after cementation is the presence of postoperative sensitivity. Conventional glass ionomer cements have higher rates of postoperative sensitivity than other cements,8 although reports show that when a manufacturer’s recommendations are followed, postoperative sensitivity is the same for zinc phosphate cement and glass ionomer cement.9–11 Before cementation, the tooth must be clean and dried to a level compatible with the cement being used. To err on the side of caution, some recommend avoiding desiccation of the dentin surface of the preparation before cementation12 to decrease the likelihood of postoperative sensitivity after cementation. Other studies describe the use of desensitizing agents and dentin sealers as part of the cementation process.13–17 However, certain desensitizing techniques can have a negative impact on adhesion. Although use of a 5% glutaraldehyde sealer15,16 or a resin desensitizer-sealer14,16,17 is not detrimental to multistep etch and rinse adhesive resin cements or glass ionomer cements, oxalate desensitizers are incompatible with glass ionomer luting agents.18
Material Options
If there were one cement for all clinical situations, it would have to be easily mixed and go through its setting reaction either quickly for a single crown or inlay or onlay or be adjustable to set more slowly for multi-unit, more involved cementation cases. Unfortunately this “holy grail” of cements is not available. However, certain factors and properties can guide the choice of cement for a given situation. In the search for an all-purpose cement, specific physical properties and handling characteristics have been quantified.19–21 The ideal properties of an all-purpose cement include the qualities listed in Box 23-1.
Box 23.1 Desirable Properties of an All-Purpose Cement
Classification of Dental Cements
Dental cements can be classified based on their chemistry and applications19–21 (Table 23-1). All cements must have a film thickness and consistency compatible with cementation, as described in American Dental Association (ADA) specification No. 96 and International Organization for Standardization (ISO) specification 9917. The three categories of dental cements are water-based, resin-based, and oil-based definitive and temporary cements. Examples of each cement type are listed in Table 23-2. This chapter focuses on glass ionomer and adhesive composite resins.
| TYPE OF CEMENT | APPLICATIONS |
|---|---|
| Water-Based Cements | |
| Conventional glass ionomer | |
TABLE 23-2 Partial Listing of Contemporary Cements
| BRAND NAME | MANUFACTURER |
|---|---|
| Conventional Glass Ionomer | |
| Ketac-Cem | 3M ESPE |
| Fuji I | GC America |
| Aqua Meron | VOCO |
| Meron AC | VOCO |
| Riva Luting | SDI |
| GlassLute | Pulpdent |
| CX-Plus | Shofu |
| Resin-Modified Glass Ionomer | |
| RelyX Luting Plus | 3M ESPE |
| RelyX Luting | 3M ESPE |
| Fuji Plus | GC America |
| FujiCEM | GC America |
| Zinc Phosphate | |
| Hy-Bond zinc phosphate | Shofu |
| Zinc phosphate | Bosworth |
| Polyacrylate | |
| Durelon | 3M ESPE |
| Hy-Bond polycarboxylate | Shofu |
| Etch-and-Rinse Resin Cement (Can Be Dual-Cure or Self-Cure) | |
| Infinity | Den-Mat |
| ResiLute | Pulpent |
| RelyX ARC | 3M ESPE |
| C&B-METABOND | Parkell |
| Calibra | DENTSPLY Caulk |
| COMSPAN | DENTSPLY |
| Twinlook | Heraeus Kulzer |
| Nexus 2 | Kerr |
| NX3 Nexus | Kerr |
| Cement-It | Pentron Clinical |
| Lute-It | Pentron Clinical |
| C&B Cement | Bisco |
| DUO-LINK | Bisco |
| Illusion | Bisco |
| CLEARFIL ESTHETIC and DC BOND | Kuraray |
| PANAVIA F2.0 | Kuraray |
| Variolink II | Ivoclar Vivadent |
| Dual Cement | Ivoclar Vivadent |
| ParaCem | Coltène/Whaledent |
| Duo Cement Plus | Coltène/Whaledent |
| PermaFlo DC | Ultradent |
| Self-Etch Self-Adhesive Resin Cement | |
| iCEM | Heraeus Kulzer |
| SmartCem2 | DENSTPLY Caulk |
| Multilink | Ivoclar Vivadent |
| RelyX Unicem | 3M ESPE |
| MonoCem | Shofu |
| MaxCem | Kerr |
| MaxCem Elite | Kerr |
| Embrace | Pulpdent |
| Breeze | Pentron Clinical |
| BisCem | Bisco |
| G-CEM | GC America |
| Veneer Cements (Light Cure) | |
| Choice 2 | Bisco |
| Illusion | Bisco |
| Calibra | DENTSPLY Caulk |
| Variolink veneer | Ivoclar Vivadent |
| RelyX veneer | 3M ESPE |
| Ultra-Bond Plus | Den-Mat |
| NX3 Nexus | Kerr |
| CLEARFIL ESTHETIC CEMENT | Kuraray |
| Compomer Cement | |
| Principle | DENTSPLY Caulk |
Resin-based cements are chemically similar to composite resins. They have higher bond strengths to tooth structure when bonded to dental adhesives. In some cases these cements are self-adhesive to dentin. For some resin-based cements, surface treatments of the restoration combined with primers and monomers allow adherence to dental metallic alloys or ceramics. Although these cements have stronger physical properties, they are generally more technique sensitive to use.22
Each category of cement presents challenges to achieving clinical success. Within each class, these cements have physical properties that allow for a consistency favorable to cementation and a film thickness that will allow for complete seating of a restoration. There is variability in the handling characteristics of each class of cement and even differences within the same class of cement. A recent survey of usage of definitive fixed prosthodontic cements noted that conventional glass ionomer was used 24% of the time, resin modified glass ionomer 46% of the time, composite resin cements 8% of the time, zinc phosphate cement 10% of the time, and zinc polycarboxylate 12% of the time.23 Generally the clinician should not assume that cements within the same class are mixed and manipulated in the same way. The dentist and chairside assistant must read the manufacturer’s instructions relative to material dispensing and mixing before using any cement on a restoration.1,18,23
Water-Based Cements
Resin-Modified Glass Ionomer Cement
Resin-modified glass ionomer (Figure 23-1) (also referred to as resin-reinforced and hybrid ionomer) is supplied as a powder-liquid, a paste-paste, or a unit-dose mixing capsule with a dispensing tip. It is easier to mix than the conventional powder-liquid glass ionomer and has improved physical properties while retaining the properties of self-adhesion and fluoride release. Some resin-modified glass ionomer cements provide a dentin conditioner to improve adhesive bonding. It is acceptable to clear away excess resin-modified glass ionomer cement when it reaches the gel stage or after complete setting. Resin-modified glass ionomer cements are less vulnerable to the effects of early moisture.
Indications for Water-Based Cements
The primary clinical indications for either type of glass ionomer cement are all-metal and porcelain-metal restorations, alumina or zirconia core-type all-ceramic restorations, implant-supported crowns and fixed partial dentures, and metal posts. It is this author’s primary cement for use in cementing all-metal and porcelain-metal restorations. The tooth must not be overly desiccated and dried when using this class of dental cement. One usually wets the dentin using a microapplicator or a damp cotton pellet so the dentin is slightly glossy with no water pooling on the surface. When glass ionomer cements were first introduced there was concern for postoperative sensitivity after cementation,7 but not all studies have found this to be a problem.8–10
Resin-Based Cements
Composite Resin Cements
All cements in this category are relatively insoluble compared with other dental cements. They have the highest mechanical physical properties, including high compressive strength, high flexural strength, good fracture toughness, low coefficient of thermal expansion and contraction, and highest stiffness of any dental cement.1,18,23 Composite resin cements are based on the chemistry of direct placement restorative composite resins and are resistant to wear and abrasion.
This class of cement offers more toothlike translucency. These cements are often available in several shades to permit better matches to adjacent tooth structures. Adhesion of this class of cement to not only tooth structure but also etched porcelain and sand-blasted metal has been demonstrated.24–27 The interface and bond between etched porcelain and composite resin when the porcelain has been treated with a ceramic primer (silane) strengthens the porcelain and eliminates the propagation of microcracks and fractures between the porcelain, composite resin, and enamel.28,29 In terms of handling, composite resin cements have easy flow, spread readily over the surface being cemented, are not tacky, can be polished, and have a chameleon effect relative to surrounding tooth structure.
Etch-and-Rinse (Total-Etch) Adhesive Resin
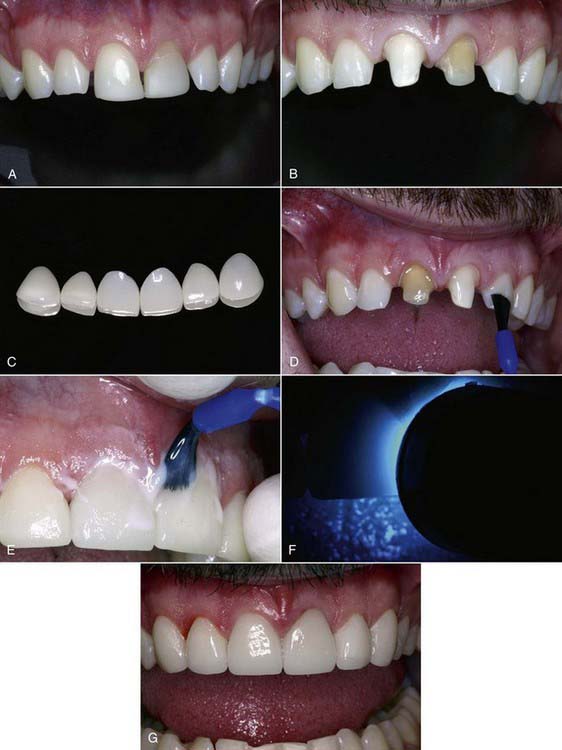
The resin cements in this category require the use of separate tooth etching with phosphoric acid combined with the application of a separate resin bonding agent. When bonding to dentin, these cements use the adhesive as the bonding interface with the composite cement. The cements can be classified as self-cure (autopolymerizing), dual-cure (light cure and self-cure), and light cure. Autopolymerizing and dual-cure composite resin cements can be used for all cementation applications, including all-metal, porcelain-metal, and all-ceramic (fritted porcelain, pressed porcelain, alumina and zirconia porcelain cores) restorations (Figure 23-2).
The use of etch-and-rinse adhesive light-cure composite resin (Figure 23-3) cements should be limited to porcelain veneers and pressable ceramic crowns that allow the curing light to penetrate the porcelain so photopolymerization of the cement under the translucent veneer or crown occurs. The differences in the polymerization mechanism are based on the chemical type of initiator. Self-cure composite resin cements use a peroxide-amine initiator-accelerator; dual-cure composite resin cements use a combination of amine and photoinitiator; and light-cure resin cements use a photoinitiator only. Self-cure composite resin cements can be used to cement all types of indirect restorations, but because of potential problems with color stability, translucent all-ceramic restorations and all-ceramic crowns and veneers should be placed with light-cure composite cements.30–32 When light-cure-only composite resin cements are used with all-ceramic veneers or crowns, the light-curing time should be increased when polymerizing through porcelain thicknesses of 0.5 to 2.0 mm.19
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses