CHAPTER 22 Prosthodontic Treatment of the Adolescent Patient
Scientific advancements in the areas of preventive dentistry, access to and use of dental services, water fluoridation, topical application of fluorides, and new commercial preventive dentistry products have led to substantial reductions in dental disease in developed countries. However, Caplan and Weintraub determined that adolescents are still affected by caries, particularly those who are minorities, rural inhabitants, have minimal fluoride exposure, and are from less educated and less affluent families.1 Results of a more recent health and nutrition survey reported by Vargas and colleagues also supports a higher caries prevalence among lower-income children and minorities.2 Assessments of periodontal health by Barmes and Leous3 and by Bader and associates4 show a decrease in severity but indicate that some adolescents are still affected.
Dental trauma continues to be a significant problem among adolescents as supported by Gift and Bhat’s assessment of orofacial injury5; Bader and colleagues’ estimates of the incidence and consequences of tooth fracture6; and Haug and associates’ epidemiologic study of facial fractures and concomitant injuries.7 Pilo and colleagues indicate that congenital anomalies continue to result in missing or malformed teeth.8 In addition, bulimia, anorexia, and dietary habits have led to an increase in the erosion of tooth structure among teenagers, particularly in girls.
RESTORATION OF SINGLE MALFORMED, DISCOLORED, OR FRACTURED TEETH
ALL-CERAMIC AND METAL-CERAMIC CROWNS
Crowns are only indicated when more conservative treatments cannot be performed or have proven to be unsuccessful. All-ceramic crowns are the most esthetic complete-coverage restorations currently available in dentistry. The achievement of optimal longevity with all-ceramic crowns requires normal tooth preparation form because the prepared tooth must provide support for the restoration. Therefore, if a large portion of tooth structure is missing because of trauma or caries, or if previous restorations become dislodged during tooth reduction, then a separate restoration that is well retained in remaining tooth structure should be placed to establish an ideal preparation form (Fig. 22-1). Also, the fracture resistance of all-ceramic crowns is enhanced when other characteristics are present. Occlusal forces should be average or below-average. The centric occlusal contacts should ideally be located over the concave lingual portion of the prepared tooth and not cervical to the cingulum where fracture of the crown is more likely to occur. The prepared tooth should possess average or greater incisocervical length and should not be short, round, or overtapered in form.
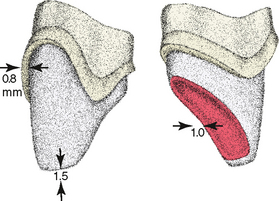
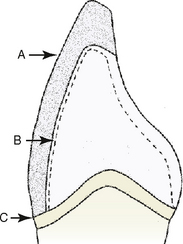
The tooth preparation for an all-ceramic crown (Fig. 22-2) should possess a well-defined, smooth finish line that is 0.8 mm deep around the entire tooth, with the axial surfaces reduced to a depth of 0.8 mm. The lingual reduction for occlusal clearance should be 1 mm. An incisal edge reduction of 1.5 to 2 mm is required and is biologically acceptable even in the presence of large pulps. The use of resin cement and associated dentin bonding is recommended because crown strength is significantly improved. Both chamfer and shoulder finish lines can be used in conjunction with resin cement without compromising restoration strength. If zinc phosphate or glass ionomer cement is used, however, then a shoulder finish line should be used to optimize crown strength.
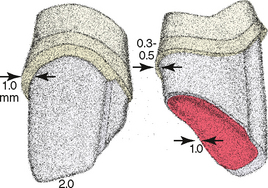
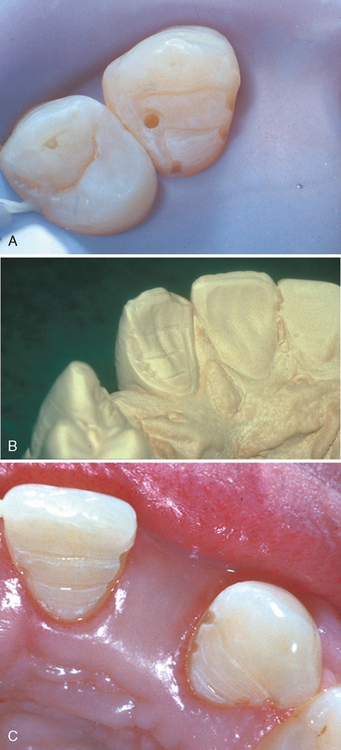
When the ideal tooth preparation form is seriously compromised or the magnitude of occlusal forces contraindicates restoration with an all-ceramic crown, use of the stronger metal-ceramic crown is indicated. The tooth preparation design and reduction depths for a metalceramic crown are shown in Fig. 22-3. When cervical esthetics must be optimized in a metal-ceramic restoration, one can use a collarless design that eliminates facial cervical metal and uses a porcelain facial margin (Figs. 22-4 and 22-5).
Whenever possible, cervical margins should not be extended into the gingival sulcus of an adolescent patient. If oral hygiene is inadequate, subgingival margins may produce accelerated gingival recession or interfere with the normal cervical relocation of the gingival tissues as the patient matures. Both occurrences produce an esthetic liability (Figs. 22-6 and 22-7).
TEETH WITH PULPAL INVOLVEMENT
When tooth fracture or caries involves the pulp and root development is complete, a routine pulpectomy and gutta-percha root canal filling should be completed. Because posts and cores do not strengthen endodontically treated teeth, their use is indicated only when remaining coronal tooth structure does not provide adequate retention for the definitive restoration.9 Restorations that do not use a post should be used whenever possible to replace missing tooth structure and serve as a retentive foundation. It is particularly important that teeth in the mouths of accident-prone adolescents or those in whom athletic trauma has previously occurred be restored without using a post, if possible. This practice helps avoid irreparable damage in the form of root fracture in case the restored tooth is once again subjected to trauma. Even though trauma may result in restoration dislodgment or perhaps even fracture of the tooth, the tooth will have survived at least one more traumatic experience.
FIXED PARTIAL DENTURES
When a tooth is lost, space maintenance should be provided immediately after extraction to prevent tipping, tilting, or rotation of the abutment teeth or eruption of the opposing teeth. Space maintenance should be continued until the fixed prosthesis is completed. If the abutment teeth are malaligned and pulp size does not permit the amount of tooth reduction necessary to align the preparations, orthodontic repositioning of the abutment teeth should be initiated.
RESIN-BONDED RETAINERS
For reasons of pulpal and periodontal health and conservation of tooth structure, resin-bonded retainers are frequently used to replace missing teeth when dental implants are not being used (Fig. 22-8). Retention and resistance form is achieved through tooth preparations, terminating in enamel, coupled with acid etching of the enamel and fixation with resin cement. The conservative approach of using resin-bonded retainers does, however, require that the abutment teeth be intact or minimally restored, with substantial enamel present for bonding procedures. To produce an adequate area for resin bonding, the existing crown should be of average or greater length. A maximal amount of the nonvisible portions of the lingual and proximal surfaces should be covered by the retainers, because Pegoraro and Barrack have determined that bond strength increases with the area of enamel covered.10 The existing crown form, color, and axial alignment must be satisfactory, because this prosthesis design does not permit the incorporation of changes in the facial enamel of abutment teeth. When abutment crown contours or color require esthetic changes, then complete-coverage retainers may produce a superior result.
Several factors important to diagnosis and treatment planning have been identified in clinical studies. Because Dunne and Millar determined that prostheses with only one pontic have much higher success rates, the use of long-span prostheses should be avoided.11 The use of multiple splinted retainers was associated with higher failure rates according to Marinello and colleagues.12 As with any prosthesis, the presence of heavy occlusal forces reduces longevity.13 The use of resin-bonded cantilevered prostheses (using only one retainer) has been reported, and data of Hussey and associates14 and Leempoel and colleagues15 indicate that this type of design can be used successfully in certain situations such as a missing maxillary lateral incisor (Fig. 22-9).
Barrack and Bretz determined that the successful use of resin-bonded prostheses requires establishment of retention and resistance form through tooth preparation (see Fig. 22-9B and Fig. 22-10).16 Because the tooth preparation is limited principally to enamel, these retainers can be used without pulpal damage and the teeth can often be prepared without anesthesia. Besimo states that the proximal surfaces adjacent to the edentulous area should be reduced to remove interproximal undercuts and to provide parallel surfaces that aid retention.17 One or two proximal grooves must be placed to enhance the resistance and retention form (see Fig. 22-10A). Proximal grooves have been identified as a key factor in the resistance to debonding in several studies.16–20 The tooth preparation should include a small peripheral chamfer finish line (see Fig. 22-10B) formed with the tip of a rounded-end diamond instrument. The lingual surfaces of anterior teeth are reduced to create occlusal clearance with the opposing teeth. The minimal occlusal clearance space for short-span (three-unit) prostheses with normal occlusal forces is 0.5 mm. It may not be necessary to reduce the abutment teeth lingually when there is existing occlusal clearance, whereas reduction of opposing teeth may be necessary when occlusal contact occurs over broad areas of the lingual surfaces. Multiple ledges, prepared across the reduced lingual surface (see Fig. 22-10C), increase the casting rigidity and, along with the proximal grooves, aid in retention and resistance form and in orientation of the casting during cementation.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses