Periodontal Response to External Forces
Adaptive Capacity of the Periodontium to Occlusal Forces
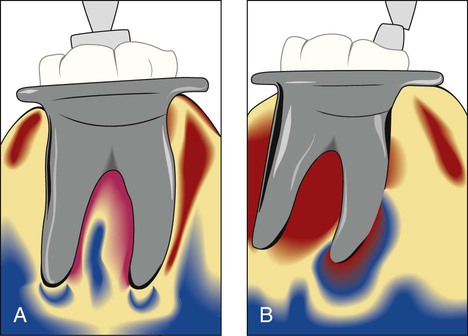
Changing the direction of occlusal forces causes a reorientation of the stresses and strains within the periodontium (Figure 22-1).23 The principal fibers of the periodontal ligament are arranged so that they best accommodate occlusal forces along the long axis of the tooth. Lateral (horizontal) and torque (rotational) forces are more likely to injure the periodontium.
Trauma from Occlusion
An inherent “margin of safety” that is common to all tissues permits some variation in occlusion without adversely affecting the periodontium. However, when occlusal forces exceed the adaptive capacity of the tissues, tissue injury results.43,44 The resultant injury is termed trauma from occlusion, which is also known as traumatism or occlusal trauma.
Thus, trauma from occlusion refers to the tissue injury rather than the occlusal force. An occlusion that produces such an injury is called a traumatic occlusion.2 Excessive occlusal forces may also disrupt the function of the masticatory musculature and cause painful spasms, injure the temporomandibular joints, or produce excessive tooth wear. However, the term trauma from occlusion is generally used in connection with injury in the periodontium.
Acute and Chronic Trauma
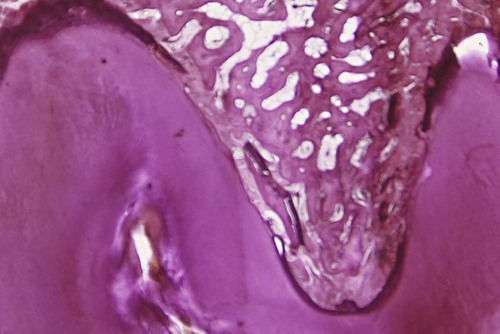
Acute trauma results in tooth pain, sensitivity to percussion, and increased tooth mobility. If the force is dissipated by a shift in the position of the tooth or by the wearing away or correction of the restoration, then the injury heals, and the symptoms subside. Otherwise, periodontal injury may worsen and develop into necrosis accompanied by periodontal abscess formation, or it may persist as a symptom-free chronic condition. Acute trauma can also produce cementum tears (Figure 22-2) (see Chapter 2).
Chronic trauma from occlusion is more common than the acute form, and it is of greater clinical significance. It most often develops from gradual changes in occlusion produced by tooth wear, drifting movement, and extrusion of the teeth in combination with parafunctional habits (e.g., bruxism, clenching) rather than as a sequela of acute periodontal trauma (see Chapter 20). The features of chronic trauma from occlusion and their significance are discussed in the following sections.
Primary and Secondary Trauma from Occlusion
Primary trauma from occlusion occurs if trauma from occlusion is considered the primary etiologic factor in periodontal destruction and if the only local alteration to which a tooth is subjected is a result of occlusion. Examples include periodontal injury produced around teeth with a previously healthy periodontium after the following: (1) the insertion of a “high filling”; (2) the insertion of a prosthetic replacement that creates excessive forces on abutment and antagonistic teeth; (3) the drifting movement or extrusion of the teeth into spaces created by unreplaced missing teeth; or (4) the orthodontic movement of teeth into functionally unacceptable positions. Most studies of the effect of trauma from occlusion involving experimental animals have examined the primary type of trauma. Changes produced by primary trauma do not alter the level of connective tissue attachment and do not initiate pocket formation. This is probably because the supracrestal gingival fibers are not affected and therefore prevent the apical migration of the junctional epithelium.48
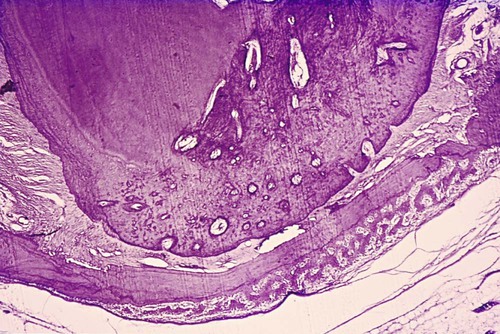
Figure 22-3 depicts three different situations on which excessive occlusal forces can be superimposed:
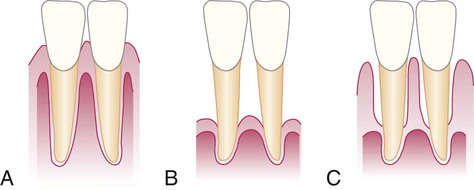
1. Normal periodontium with normal height of bone
It has been found in experimental animals that systemic disorders can reduce tissue resistance and that previously tolerable forces may become excessive.21,51,61 This could theoretically represent another mechanism by which tissue resistance to increased forces is lowered, thereby resulting in secondary trauma from occlusion.
Stages of Tissue Response to Increased Occlusal Forces
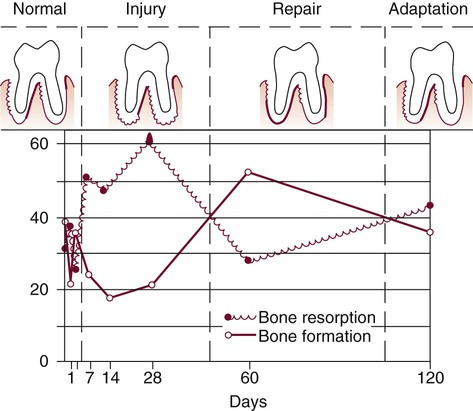
Tissue response occurs in three stages4,8: injury, repair, and adaptive remodeling of the periodontium.
Stage I: Injury
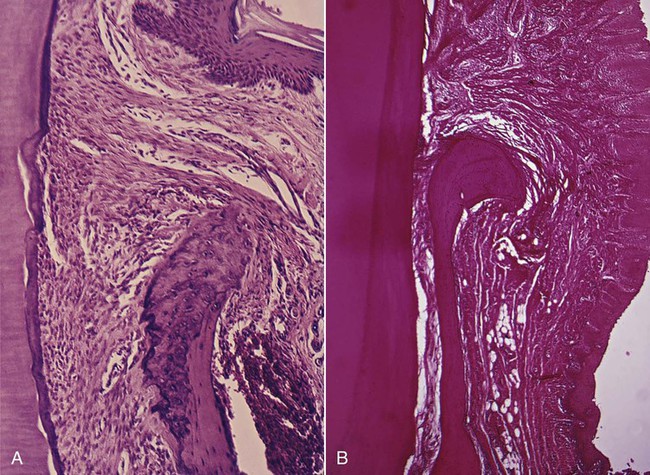
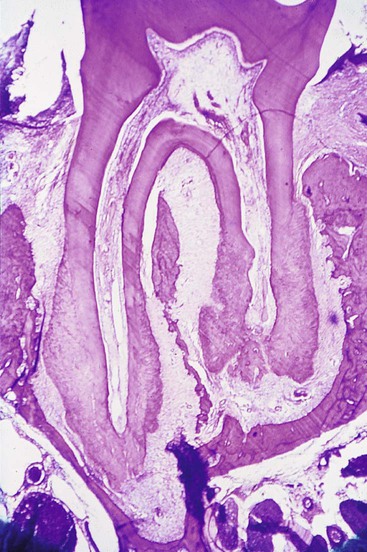
Under the forces of occlusion, a tooth rotates around a fulcrum or axis of rotation, which in single-rooted teeth is located in the junction between the middle third and the apical third of the clinical root and in multirooted teeth in the middle of the interradicular bone (Figure 22-4). This creates areas of pressure and tension on opposite sides of the fulcrum. Different lesions are produced by different degrees of pressure and tension. If jiggling forces are exerted, these different lesions may coexist in the same area.
The areas of the periodontium that are most susceptible to injury from excessive occlusal forces are the furcations.22
Injury to the periodontium produces a temporary depression in mitotic activity, in the rate of proliferation and differentiation of fibroblasts,62 in collagen formation, and in bone formation.29,58,60,62 These return to normal levels after the dissipation of the forces.
Stage III: Adaptive Remodeling of the Periodontium
If the repair process cannot keep pace with the destruction caused by the occlusion, the periodontium is remodeled in an effort to create a structural relationship in which the forces are no longer injurious to the tissues.18 This results in a widened periodontal ligament, which is funnel shaped at the crest, and angular defects in the bone, with no pocket formation. The involved teeth become loose.67 Increased vascularization has also been reported.9
The three stages in the evolution of traumatic lesions have been differentiated histometrically by the relative amounts of periodontal bone surface undergoing resorption or formation5,8 (Figure 22-8). The injury phase shows an increase in areas of resorption and a decrease in bone formation, whereas the repair phase demonstrates decreased resorption and increased bone formation. After adaptive remodeling of the periodontium, resorption and formation return to normal.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses