Ethical and Legal Issues
Ethical Considerations
1. Ethics—the science of human duty; correlate motives and attitudes with moral actions and values
2. Professional ethics—rules or standards governing conduct of members of a profession
3. Bioethics—ethical and moral implication of new biologic discoveries and biomedical advances
1. Are the foundation of ethical analysis; explain moral principles
2. Provide a basis for ethical rule, policy development, or both
1. Teleologic/utilitarian ethics (John Stuart Mill)—comprise rules for conduct based on consequences of action; an action is considered right or wrong on the basis of its usefulness; useful actions bring about the greatest good for the greatest number of individuals
a. Act utilitarianism—examines a situation and determines which course of action will bring about the greatest happiness or least harm and suffering to an individual regardless of personal feelings or societal constraints such as laws
b. Rule utilitarianism—searches for the greatest happiness and seeks public agreement to define nature of happiness; considers the law and fairness; an action is considered right if it conforms to a rule; the rule should have positive results in a wide range of situations
2. Deontologic ethics (Immanuel Kant)—focus on the morality of the act rather than the situation or consequences of actions; one would say, “It’s the principle of the thing”; a person’s intention, not the consequences of the action, is key; three important elements: applied universally to all individuals, unconditional, demand an action
a. Act deontology—based on personal moral values of the individual making the decision and considers the ethical principles involved in an action in light of the circumstances—for example, avoid the truth if it is harmful
b. Rule deontology—based on the belief that certain standards for ethical decisions are of greater value than an individual’s moral values; considers the principles and rules in general as they apply to types of actions
3. Virtue ethics (Aristotle and Plato)—focus on character traits and excellence of character; evaluate ethical dilemma by asking, “Is this what a virtuous person would do?”
a. Situational ethics—course of action determined by:
(1) The unique characteristics of each individual
(2) The relationship between the health care provider and the client
b. Principalism—focuses on ethical principles, including autonomy, beneficence, nonmaleficence, and justice
c. Professional codes of ethics—designed in a rule-making format; usually direct decision making among professionals more than ethical theories
1. Veracity—truthfulness; mutuality for the client and the provider, for example, the client must be truthful to receive appropriate care, and the provider must provide truthful information so that the client can exercise his or her autonomy
2. Autonomy—personal liberty; individuals are free to make decisions regarding their own health; respect for the individual autonomy of others is basic to the health care provider–client relationship; informed consent and informed refusal is basic to autonomy (see discussion on informed consent in the section on “Legal issues for the dental hygienist” later in this chapter)
3. Beneficence—the provider’s duty is a commitment to the health and welfare of the client above all other considerations; duty to prevent or remove harm and promote good
4. Nonmaleficence—the provider’s duty not to use the treatment to injure or wrong the client; inflict no harm
5. Fidelity (role fidelity)—health care providers are required to provide services within the scope of their practice; ethics require that health care providers practice within the constraints of the role assumed within the health care environment; the provider is expected to follow through with commitments
6. Confidentiality—based on an individual’s right to privacy, for example, client has the right to expect all his or her medical records and communications to be kept confidential
Professionalism
Defining a Profession
A Characteristics of a profession
1. Special advanced education or preparation
4. Promotion of a body of knowledge in the field (research and theory development)
7. The recognized authority with societal sanction
1. Historical evidence of Western medical ethics traced to guidelines outlining the duties of physicians
2. Early evidence included oaths and rabbinic and Christian sources
4. Oath of Hippocrates—fifth century B.C.E.; statement of principles guiding the professional conduct of physicians
a. Stated “Above all, do no harm”
b. Protected the rights of the patients
c. Admonished physicians to keep the confidence of patients
d. Placed needs of patient above those of society
e. Placed an obligation on physicians to teach the next generation of physicians
5. Ethical codes for health care professionals continue to be evaluated and revised to reflect:
b. Protections for population groups that are subjects in research investigations
a. Self-imposed—the health care professional self-assesses and determines compliance; range of sanctions from a professional organization or licensing agency for lack of compliance
b. Set rules governing behavior—the professional uses them as a framework for action
c. Serving to protect the public—on the basis of ethical principles that support actions to benefit the client and prevent harm
d. Striving to enhance the profession—adherence to code characterizes a profession
7. American Dental Hygienists’ Association (ADHA) Code of Ethics and the Canadian Dental Hygienists’ Association (CDHA) Code of Ethics
a. Identify and describe ethical principles to guide the oral health care provider
b. State the obligations and responsibilities of the dental hygienist
8. Codes of Ethics—compare all codes
a. For the ADHA’s Code of Ethics, visit the Web site at http://www.adha.org/downloads/ADHA-Bylaws-Code-of-Ethics.pdf (also see Appendix C)
b. For the CDHA’s Code of Ethics, visit the Web site at http://www.cdha.ca/pdfs/Profession/Resources/CDHA_Code_of_Ethics_public.pdf
c. For the American Dental Association’s Code of Professional Responsibility and Conduct (revised January 2010), visit the Web site at http://www.ada.org/ethicsconduct.aspx
9. Client’s Bill of Rights—outlines client expectations and provides guidelines for provider conduct; the client has the right to:
a. Respectful, competent, and considerate care irrespective of ethnicity, gender, national origin, age, or disability
b. Receive current, accurate, and complete information regarding diagnosis, treatment, and prognosis
c. Receive information necessary to give informed consent or informed refusal before treatment; be informed of the consequences of refusing treatment.
d. Confidentiality regarding all communications, consultations, and records except when permission has been granted to submit this information to others
f. Obtain information relating to the credentials of all providers rendering services
g. Reasonable continuity of care
h. Examine and receive accurate copies of professional services and fees
i. Receive treatment from health care professionals who act within the limits of their professional licenses (scope of practice) and adhere to the standard of care in delivering services
10. Types of professional credentials
a. Licensure—state regulation of professionals
(1) Granted by a state agency or board
(a) Responsibilities and behaviors prescribed by law in the state practice act in the United States or determined by the provincial practice act in Canada
(b) Responsibilities and behaviors delineated by rules and regulations
(3) Authorized practice by professionals meeting specified qualifications
(4) Failure to meet responsibilities and expected behaviors may result in fines, suspension, or removal of license
(5) Status of license available to public; may indicate current license status (e.g., active, pending, suspended)
(6) The purpose is to protect the public from unqualified or unethical providers
b. Registration—qualified professionals listed in a directory
(1) Dental hygiene is a self-regulated profession in most Canadian provinces, and registration is a provincial responsibility (e.g., College of Dental Hygienists of Ontario http://www.cdho.org/indexmain.htm)
(2) A certificate of registration to practice is issued only to those who meet established standards of qualification and practice
Ethical Issues in Public Policy
A Ethical issues and public policy
1. Distributive justice—fair allocation of resources involved
a. Macro-allocation of resources—based on public needs (e.g., water fluoridation)
b. Micro-allocation of resources—based on individual needs (e.g., fluoride varnish treatment)
2. Distributive justice or allocation of scarce resources—determination of who should receive treatment when all cannot be treated; services may be allocated on basis of:
a. Equity—all persons receive equal treatment
b. Need—treatment allocated on the basis of prioritized needs
c. Effort—treatment allocated to those who have earned it
d. Contribution—treatment allocated to those who are making a contribution to society
e. Merit—treatment allocated to those who are most deserving
3. Influenced by principles of human dignity and human rights and contributing to the common good
4. Current health policy debates
a. Question of whether public health funds should be used for:
(1) Financial assistance and care of the disadvantaged or seniors
(2) Financial assistance and care for undocumented immigrants
(1) Identification of appropriate decision makers to identify and prioritize research agendas, especially for controversial topics (e.g., stem cell research)
(2) Identification of sources of financial support (e.g., what proportion of the national budget should be allocated to health care and research
1. A system of plans of action, regulatory measures, laws, and funding priorities concerning a specific topic or issue
2. Promulgated by a governmental entity or its representatives
3. Public policy is commonly embodied in constitutions, legislative acts, and judicial decisions
C Creating public health policy
1. Goal—assessment of a variety of actions and consequences to solve identified societal problem
2. Action—a decision by all members of society or their elected representatives (e.g., public vote versus state legislature passing statute regarding mandatory use of seat belts)
3. Analysis—determining which policy among alternatives best achieves the goal, how policy should be implemented, or how to evaluate what is currently being done
D Policy makers—usually legislators, members of executive branch of government, and government officials who write regulations
E Policy analysts—provide policy makers with information required to determine the impact of past and current public policies; determine whether new policy should be implemented or present policy or nonpolicy should continue
F Examples of community-based programs requiring public policy analysis
1. Federal or state partnerships to provide oral health services
2. Fluoridation initiatives (e.g., community water fluoridation and school fluoride programs)
3. Caries prevention programs such as dental sealant or fluoride varnish programs in public health settings
4. Provision and funding of oral health care services by nondental personnel
G Policymakers may seek input from professionals or professional associations; health-related professional associations frequently hire lobbyists to influence government policy makers
H Distinctions between ethics and law
1. Laws are societal mandates, whereas ethics are professionally based
2. Ethical principles and legal doctrine are related
a. Ethical principles integral to federal and state legislation that is enacted
3. Ethical duties are usually greater than legal duties; for example, a health care provider who is acquitted in civil or criminal court after being charged with illegal conduct did not necessarily act ethically
4. Compliance with the law sometimes mandates unethical conduct—health care providers are ethically and legally bound to keep confidential all client communications and records; however, the law makes exceptions and requires disclosure to appropriate authorities in specific situations (e.g., in cases of suspected child or elder abuse or threats of inflicting bodily harm to another person or self)
5. Personal values not necessarily congruent with professional ethics or the law—under law, individuals have a right to control their own bodies; this includes the right to refuse medical or dental treatment; health care providers must honor this right despite their own personal values
6. Differentiating between ethics and law (Table 22-1)
TABLE 22-1
Differentiating Between Ethics and Law
| Ethics | Law | |
| Definition | Individual interpretation of the nature of right and wrong and rules of conduct | Rules and regulations by which society is governed set forth in a formal and legally binding manner |
| Source | Internalized; individual nature and beliefs | Externalized rules and regulations of society |
| Emphasis | Individual moral behavior for the good of the individual within society | Social behaviors that are good for society as a whole |
| Conduct | Motives and reasons why the individual behaves the way he or she does | Overt conduct of the individual; what a person actually did or failed to do |
| Sanctions | Professional organization—expulsion from the organization | Judicial and administrative bodies—criminal sanctions such as fines and imprisonment imposed by the courts; civil sanctions such as monetary damages imposed by the courts; disciplinary sanctions such as fines, license suspension, or license revocation by a board of dentistry |
Legal Concepts
1. Rules and regulations that govern society
2. Reflects society’s attitudes, mores, and needs; therefore, law is constantly changing to meet the requirements and expectations of society
a. Constitutional law—supreme law of the land; both state and federal laws must be consistent with the U.S. Constitution
b. The U.S. Constitution establishes the organization of the federal government and places limitations on the federal government through the Bill of Rights (first 10 amendments to the U.S. Constitution)
c. Delineates the specific powers of the federal government to the:
d. Powers not specifically granted to the federal government are the powers of state government
e. Each state has its own constitution that grants powers and places limitations on the powers of the state government
a. Laws made by the legislative branch of government (federal, state, and local governments)
b. State dental practice acts are examples of statutory laws
a. Administrative agencies are given the authority to oversee the specific laws or statutes to ensure that the intent of the law is enforced
b. Administrative laws are the results of decisions of administrative agencies, for example, state boards of dentistry or the College of Dental Hygienists of Ontario implement rules and regulations to enforce the law
c. Administrative agencies may conduct investigations and hearings and may issue decisions that suspend or revoke the license of a dentist or a dental hygienist; decisions of administrative agencies may be appealed through the state court system to determine whether:
a. Determined by courts (state, provincial, and federal), which interpret legal issues in dispute
b. Stare decisis1 (Latin, meaning “let the decision stand”)—doctrine of law whereby the court will base its decision on previous case law (a prior case with similar facts); the previous case must be from the same jurisdiction (state); emphasizes the importance of legal precedent
c. Landmark decisions—court decision that departs from precedent, for example, new technology may require different conclusions based on the same facts
d. Res judicata1 (Latin, meaning “a thing or matter settled by judgment”)—legal doctrine that applies when a legal ruling has been made by a competent court of jurisdiction, and no appeals are possible; prevents parties from taking the same issues to different courts
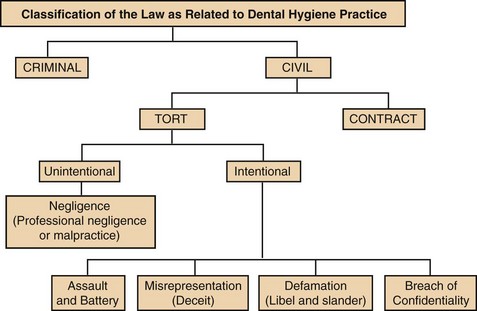
C Classifications of law (Figure 22-1)
1. Common law and civil law—two concepts of legal thought, one from England (common law) and one from Europe (civil law)
a. Common law—general principles derived from decisions in case law using the concept of precedent
b. Civil law—civil code system developed by legislature, based on rules and regulations; enforced through the court system and protects the legal rights of private persons
c. Level of proof—preponderance of evidence; the greater weight of the evidence required in a civil (non-criminal) lawsuit for jury or judge without a jury to decide in favor of one side or the other
2. Criminal law—relates to acts considered offensive to society as a whole
(1) Misdemeanors—usually involve fines of less than $1000 or imprisonment for less than 1 year, or both; examples include vandalism, trespassing, and reckless driving
(2) Felonies—serious crime; usually involve punishment ranging from fines of more than $1000 or imprisonment of more than 1 year (or both); receiving a death sentence depending on the crime committed and the jurisdiction (state); examples include robbery, illegal drug use or sale, and battery
b. Certain violations of law may be considered both criminal and civil, for example, if a client loses his or her life resulting from gross negligence of a dental hygienist, the dental hygienist could suffer loss of professional license, the estate of the deceased person could bring civil charges such as wrongful death against the hygienist, and the state may bring criminal action such as manslaughter against the hygienist
c. Level of proof required to determine innocence or guilt beyond a reasonable doubt; the level of certainty a juror must have to find a defendant guilty of a crime
D Primary individuals involved in a lawsuit
1. Plaintiff—party bringing the lawsuit
2. Defendant—party against whom the lawsuit is filed
3. Attorney—individual serving as an advocate for either the plaintiff or the defendant
4. Expert witness—explains specialized information to jurors; possesses appropriate credentials and expertise
5. Lay witness—testifies as to facts for judge and jury
6. Dental hygienist as a witness (lay or expert)
a. Expert qualifications based on education, licensure or certification, experience, and publications
b. Expertise to testify as to standard of care for dental hygiene
c. Familiarity with the state or provincial dental practice act
d. Knowledgeable about all written records relating to the controversy
e. Knowledge of office or institutional policy and procedure where (and at the time) the incident occurred
E Due process and equal protection
1. Due process—protects the public from arbitrary actions of the state; the law must apply to all persons equally; elements of due process
a. The law, as applied, must be reasonable and definite
b. Fair procedures must be followed in enforcing the law, for example, the state may not arbitrarily take away a license to practice dental hygiene; the hygienist must first be given notice of the violation, a hearing, and an opportunity to respond before license revocation or suspension is imposed
2. Equal protection—equal protection clause of the Fourteenth Amendment to the U.S. Constitution protects individuals from state action; states may not enforce laws based solely on classification of persons such as race, age, gender, religion, national origin, or disability
1. Questions of law or fact—usually the jury determines what is fact from the evidence admitted by the court; the judge determines questions of law
2. Jurisdiction of the courts—authority of the court to determine the controversy, for example, the bankruptcy court may not hear divorce cases
a. Trial courts—courts with trial jurisdiction; usually handle cases such as traffic, probate, family matters, arraignments for felonies, small claims, juvenile, and criminal misdemeanors
b. Appellate courts—courts with trial, appellate, civil, and criminal jurisdiction; usually with a monetary restriction (plaintiff must request a fair minimum amount)
a. Federal district courts—courts with trial jurisdiction; hear only matters that involve federal law or parties with diversity of citizenship (residents of different states)
b. U.S. Courts of Appeal—courts with appellate jurisdiction only
c. U.S. Supreme Court—court with appellate jurisdiction only; decisions cannot be overturned by any other court (state or federal); decisions can only be changed by new congressional legislation or subsequent Supreme Court decisions
1. Each state (or province) has a statute (law) that delineates specific periods within which a lawsuit must be filed after the event that caused the action; after that period, the right to initiate a lawsuit is lost
2. In tort actions, time may be measured from the time of the injury or harm or may be measured from when the plaintiff discovers the injury; periods vary from state to state
H Case law—case law comprises the decisions, or the interpretations made by judges while deciding on the legal issues before them which are considered common law or as an aid for interpretation of a law in subsequent cases with similar conditions; case law is used by attorneys to support their views to favor their clients; it also influences the decisions of the judges; it is public record (occasionally court records are sealed)
1. Legal decisions available in publications appropriate for the level of the court where the case was tried; most decisions of state appellate courts are published in regional reports
2. Citations—references to legal authority that provide key information about the case, for example, in the following citation, Edwards v Penn. Dental Examining Board, 454, A2d 218 (1983): Edwards is the plaintiff (party bringing the lawsuit), the Dental Board is the defendant (party against whom the lawsuit is filed), 454 is the volume number of A2d (second series of the Atlantic Regional Reporter); 218 is the page number; and 1983 is the year the case was decided
Civil Law and the Dental Hygienist
A A lawsuit can be filed against an oral health care provider in two areas of civil law:
B Contract law1—a contract is an agreement between two or more consenting and competent parties to do or not to do a legal act for which sufficient consideration exists; breach of contract occurs if either party fails to comply with the terms of the contractual obligations
1. Two methods to create a contract:
a. Implied contract through signs, inaction, or silence; also called apparent
b. Express contract entered through oral or written communication
2. The contract exists between a client and a health care provider when the client agrees to a specific treatment
3. Contractual responsibilities of the provider to the client
a. Possess proper license and certification
b. Exercise reasonable skill, care, and judgment in diagnosis and treatment
c. Use standard drugs, materials, and techniques
d. Complete the treatment in a reasonable time
f. Complete procedures consented to by the client
g. Provide adequate instructions
i. Maintain confidentiality and client privacy
j. Maintain an appropriate level of knowledge
k. Practice within the scope of practice never exceed the defined scope
4. Contractual obligations of the client
a. Pay a reasonable fee in a reasonable time
d. Provide accurate history; information
5. Client–practitioner relationship—contractual; both are free to enter or decline the relationship; the practitioner may decline to undertake treatment of a client unless he or she has agreed to treat the client by participating in a specific dental insurance plan or the practitioner is employed by another who makes treatment decisions; if the practitioner offers services to the public, he or she may not refuse to treat clients because of race, color, gender, religion, national origin, disability, or any other basis that would constitute invidious discrimination; being bound to the code of ethics assumes a preexisting relationship of the client-practitioner
6. Termination of the client–practitioner relationship may be by:
b. The practitioner, after giving the client notice and an opportunity to secure an alternative source of future treatment
7. Abandonment1—failure of a health care professional to provide services after the health care professional has established a relationship with the client; duty to the client to complete all treatment started; clients may be dismissed from future treatment
C Tort law1—deals with civil wrongs committed against a person or a person’s property; wrongful conduct
(1) Negligence—failure to use such care as a reasonable person would use under similar circumstances
(2) Malpractice—wrongful acts of professional persons; usually failure to meet the standard of care or failure to foresee consequences that one with his or her particular skills and education should foresee
b. Elements of negligence or malpractice, which must be shown in order for a lawsuit to go forward
(1) Duty owed to the client (the plaintiff)
(2) Breach of the duty by the professional or the defendant
(3) Harm to the client (the plaintiff)
(4) Causation—harm must be caused by breach of duty; foreseeability, that is, the event may reasonably be expected to cause the result
c. Standard of care—the degree of care that a reasonably prudent professional should exercise; minimum requirements of acceptable client care, for example, practicing within the rules and regulations of the state or provincial dental practice act
d. Damages (awarded to the defendant; to restore injured party)
(1) Special damages—actual expenses
(2) Nominal damages—at the court’s discretion (could be $1)
(3) General damages—part of harm; difficult to determine (e.g., can include pain and suffering)
(4) Contract damages—for breach of contract
(5) Punitive damages—to punish deliberately wrongful conduct (usually not covered by liability insurance)
(6) States may place a cap on the maximum allowable damages that can be paid
e. Res ipsa loquitur1 (Latin, meaning “the thing speaks for itself”)—legal doctrine that permits the plaintiff to prove negligence or malpractice without proving fault; no expert testimony required if the plaintiff shows a particular result occurred and would not have occurred but for someone’s negligence
(1) The type of injury does not occur unless negligence has occurred
(2) The injury is caused by something or someone under exclusive control of defendant
(3) The injury was not caused by plaintiff by contributing to own injury in any way (no contributory negligence)
f. Defenses to unintentional torts (protect defendant from liability)—not limited to, but include:
(1) Statute of limitations—time limit for initiating lawsuit has passed
(2) Comparative or contributory negligence—injured party is held responsible for a portion or all of the injury (states or provinces differ regarding degree of responsibility)
(3) Release—signed during the settlement of claim to prevent future claims
(4) Immunity—protection from prosecution, for example, the action may fall within a state’s Good Samaritan law
2. Intentional tort—an act must be willful; the defendant must have intended to cause the harm or injury; the act must have been a substantial factor in bringing about the injury
a. Assault—any action that places one in fear of bodily harm (e.g., threatening behaviors)
b. Battery—intentional infliction of offensive or harmful bodily contact; unwanted touching
c. Defamation—communication to a third person of an untrue statement about another person
(1) Libel—written defamation (e.g., untrue or unflattering statement entered into a client’s record)
(2) Slander—spoken defamation (e.g., discussing an employer in a derogatory manner while dining in a restaurant and being overheard by a third person)
d. Invasion of privacy—protects one’s right to privacy
(1) Intrusion on seclusion—invasion of a private place or affairs of another; must be highly offensive to a reasonable person
(2) Appropriation—use of another’s name or likeness for financial gain (e.g., unauthorized photographs of dental clients used in a research article or textbook)
(3) Publicity of private life—publicizing details of another person’s private life; must be highly offensive to a reasonable person; health care professionals must not disclose a client’s information without written authorization (e.g., no disclosure of client information over the phone or to client’s relatives, including spouse or friends)
(4) False light—putting another person before the public eye in a false light; highly offensive to a reasonable person
e. Infliction of mental distress—outrageous conduct that causes emotional distress; behavior must be beyond standards of rudeness; behavior was intended to cause mental distress and actually did cause mental distress (e.g., publicly revealing client’s nonpayment; notifying neighbors or relatives of nonpayment)
f. Fraud or intentional misrepresentation—intentional perversion of truth (misrepresentation) for the purpose of gaining another person’s trust and reliance whereby that person suffers harm or loss as a result of trusting and relying (e.g., never guarantee treatment outcomes)
g. Interference with advantageous relations—generally prevents an individual from interfering with the gainful employment of another; name and definitions may vary from state to state; giving a former employee a poor reference is not a basis for this tort
h. Wrongful discharge—illegal termination of an employee; most dental hygienists are hired without employment contracts and are employees-at-will; they can be fired for any reason except
(1) If reason for firing was against federal and/or state anti-discrimination laws, e.g., pregnancy of employee
(2) If firing is against public policy, e.g., sexual harassment or “whistleblower” cases
(3) Office policy and procedures (oral and written) may be considered an implied employment contract, e.g., office manual must address the issue in controversy
i. Defenses against intentional torts are not limited to, but include
(1) Statute of limitations—whether the time limit for initiating lawsuit has passed
(2) Privilege—person making the statement has the duty to do so; for instance, dental hygienists are often required by state law to report cases of suspected child abuse; in that case they are not held legally liable for doing so
(3) Disclosure statutes (state and federal)—permit access to client records by specific individuals or agencies without client consent, e.g., worker’s compensation statutes allow for such access to client information if a claim is filed
(4) Consent: oral, implied by law, e.g., during emergencies (when a client is not capable of consent), or apparent, e.g., client sits in dental chair and opens his or her mouth for an examination
(5) Self-defense or defense of others—behavior is justified to protect self or others from harm; if force is necessary, one may use only the amount of force necessary for protection (reasonable force)
(6) Necessity—allows personal property to be confiscated, e.g., weapon
3. Informed consent—from concept of battery and individual rights to make choices regarding his or her own body
a. Content—legal requirements vary from state to state; in general, a client must have information that a reasonable person would find material in making a decision regarding treatment
b. Client should be told in a language or format that he or she can understand
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses