22 Dental Fluorosis
Dental fluorosis is a permanent hypomineralization of enamel that is characterized by greater surface and subsurface porosity than in normal enamel and that results from exposure of the immature tooth to excess fluoride (F) during developmental stages. Preeruptive enamel maturation consists of an increase in mineralization within the developing tooth and a concurrent loss of early-secreted matrix proteins. Excess F available to the enamel during maturation disrupts mineralization and results in excessive retention of enamel proteins.5 Fluorosis is thought to result from the unerupted tooth’s constant exposure to elevated plasma F concentrations rather than from periodic spikes in F concentration.69 Although sufficiently high F concentrations might affect enamel at all developmental stages,15 early preeruptive maturation appears to be the time when enamel is most sensitive to the effects of F, both in animals16,53 and in humans.19 Elegantly designed human studies have suggested that this critical period for the development of fluorosis in the human maxillary permanent central incisor begins around the age of 22 months and extends for periods of up to several years after that for later-developing teeth.19
In its mildest forms, fluorosis appears as barely discernible fine, lacy markings that follow the perikymata across the width of the enamel surface. At this very mild level, fluorosis can be detected only by an experienced dental examiner. At the opposite extreme, the most severe forms of fluorosis manifest as heavily stained, pitted, and friable enamel that can result in loss of dental function. Fluorosis is a dose-response condition; gradations between these two extremes range from more obvious white, lacy markings to a nontranslucent white coloration of the whole enamel surface. The brown stain that often accompanies moderate fluorosis is a posteruptive feature that results when certain dietary ingredients are picked up by proteins in the porous outer enamel21; it is seen only when porous enamel has formed prior to eruption.
Fluorosed surface enamel contains higher F concentrations than does unaffected enamel, and the F enamel content increases with the severity of the condition.52 Teeth that mineralize later in life generally show more severe fluorotic disturbances than do those that mineralize earlier.3,35–37 Fluorosis is less common in the primary than in the permanent dentition, although fluorosis of the primary teeth does occur.66,67 It is common in the primary dentition in high-F areas of the world, such as East Africa.34,45,46,62
Because dental fluorosis is a dose-response condition, the higher the F intake during the critical period of tooth development, the more severe the fluorosis.14,17,35 The threshold, if indeed there is one, is low: 0.03-0.1 mg F/kg body weight has been suggested as the borderline zone,22 at least for European children. Because that range encompasses the so-called optimum intake range of 0.05-0.07 mg F/kg body weight per day (Chapter 24), it is not clear whether other factors (e.g., nutrition) lead to these differences in estimates or whether they merely reflect biologic variation. Studies in Kenya have found fluorosis with average intakes as low as 0.04 mg F/kg body weight.3 Certainly a range of fluorosis severity is seen among individuals who appear to have similar exposures to F.
In those parts of the world where severe fluorosis is endemic, such as some regions of Africa, the condition can be seen when F levels in drinking water are low,18 so that other, unknown exposure sources must be present. In other cases it occurs with ingestion of certain foods known to be high in F.70 Studies in such localities have increased our understanding of fluorosis, but the living conditions in those areas differ greatly from those in the United States and other high-income countries.
PREVALENCE OF FLUOROSIS IN THE UNITED STATES
Fluorosis in the United States was first mapped by Dean during his classic studies of the 1930s and early 1940s. These studies are discussed in Chapter 24; they are an integral part of the story of how fluorosis and caries experience were first associated with F concentrations in drinking water.
One part of the United States that received a lot of attention from Dean was northern Illinois, where there is an extensive belt of naturally fluoridated drinking water. Seven of these communities, with water naturally fluoridated to varying degrees, were revisited by researchers from the National Institute of Dental and Craniofacial Research (NIDCR) in 1980, in 1985,27 and again in 1990.56 Relating age to fluorosis and tooth calcification, the NIDCR team concluded that F intake had increased during 1970-77 but had not increased subsequently. The 1990 follow-up found that the rise in age-standardized fluorosis prevalence observed in the optimally fluoridated areas over 1980-85 did not continue during 1985-90. At above-optimum water F concentrations, fluorosis either remained stable or showed no sustained increase over the decade between 1980 and 1990.
Although there are difficulties in comparing data obtained 60 years apart, it is clear that the prevalence of dental fluorosis in the United States has increased since the time of Dean.12,60 Prevalence among children was reported to be 22.3% in the 1986-87 National Survey of Dental Caries in U.S. School Children, ranging by age from 18.5% of 17-year-olds to 25.8% of 9-year-olds.7 This higher prevalence in the younger children hints that prevalence might still be increasing. Almost all of the fluorosis recorded in the 1986-87 survey was mild or very mild. Although there is little firm evidence, a slight increase in fluorosis severity may have accompanied the large increase in prevalence.63
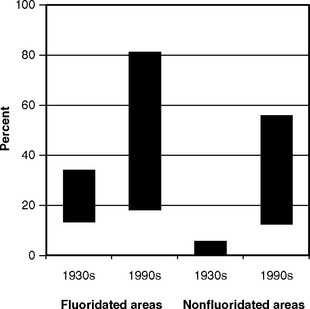
The largest relative increase in fluorosis since Dean’s time has been seen in nonfluoridated areas (Fig. 22-1), which suggests that the F exposure from sources other than drinking water is driving the increase in fluorosis prevalence.
RISK FACTORS FOR DENTAL FLUOROSIS
Because fluorosis is a disturbance of enamel due to excessive F intake during the developmental period, risk factors are related to the ingestion and absorption of F at the critical periods of preeruptive tooth development. Age is a demographic risk factor in that fluorosis can only occur with preeruptive F exposure. There is no evidence for racial or ethnic differences, and socioeconomic status (SES) is a demographic risk factor only to the extent that F exposure from toothpaste and infant formula may vary by SES. There is no reason to believe that the use of F mouthrinses and the presence of professionally applied gels and varnishes are risk factors for fluorosis, although obviously the protocols for application of these products must be designed to minimize ingestion.
Fluoridated Drinking Water
Drinking fluoridated water is a minor risk factor for fluorosis. It was documented long ago that in the United States, even at around 1.0 parts per million (ppm) F, 7%-16% of children born and reared in areas with fluoridated water exhibit mild or very mild dental fluorosis in the permanent dentition.1,14,55 This degree of prevalence was recorded at a time when drinking water was virtually the only source of exposure to F, and prevalence has risen relatively more in the nonfluoridated areas since then.33,56 Even small changes in F concentrations in drinking water can lead to considerable change in fluorosis prevalence.20,61
Fluoride Dietary Supplements
F dietary supplements, in the form of tablets, drops, or F-vitamin combinations, have been used for years in nonfluoridated areas to prevent caries (see Chapter 26). Regardless of the role of F supplements in preventing caries, there is strong evidence that supplements are a risk factor for mild to moderate fluorosis. Case-control studies in nonfluoridated areas of New England found that exposure to F supplements during the first 6 years of life, together with higher SES, significantly increased the risk of developing fluorosis.48,50 Later research, as would be expected, found the risk to be extremely high when supplements are used (inappropriately) in fluoridated areas.49 Other studies have demonstrated the link between use of supplements and fluorosis risk,2,32,34,
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses