Chapter 22 Applied Anatomy for Dental Implants
The surgical anatomy of the maxilla and mandible provide the foundation required to safely insert dental implants. The anatomy is also a requisite to the understanding of complications that may inadvertently occur during surgery, such as injury to blood vessels or nerves, as well as postoperative complication such as infection. This information also provides the operator with the confidence needed to deal with these complications. This chapter addresses those issues important in the field of oral implantology.
SURGICAL ANATOMY OF THE MAXILLA AS AN ORGAN
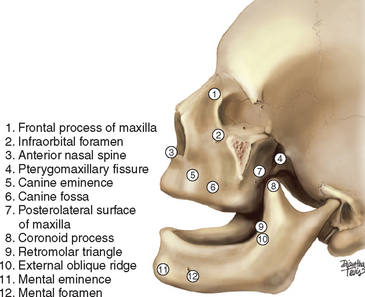
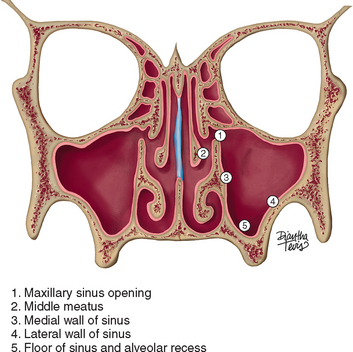
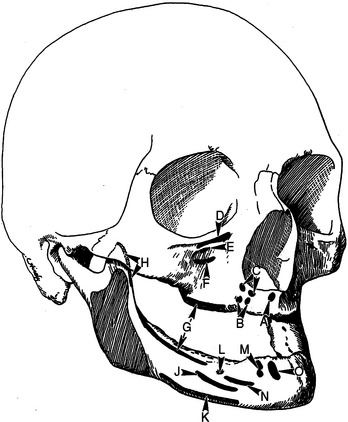
The maxilla is pyramidal in shape with the root of the zygoma as its apex (Figures 22-1 and 22-2). The latter can be palpated in the buccal vestibule of the oral cavity. It divides the facial surface of the maxilla into anterolateral and posterolateral surfaces of the pyramid. The third surface of the pyramid is the orbital plate of the maxilla. The base of the pyramid is the lateral wall of the nose or the medial wall of the maxillary sinus. The alveolar process of the maxilla related to the anterolateral surface carries the incisors, the canines, and the premolars, whereas that of the posterolateral surface carries the molars and ends as the maxillary tuberosity. The intraoral part of the maxilla is limited by the mucobuccal fold and the orbicularis oris muscle anteriorly and by the buccinator muscle posteriorly. The posterolateral surface of the maxilla above the mucobuccal fold forms the anterior wall of the infratemporal fossa and is difficult to palpate. However, the anterolateral surface of the maxilla beyond the mucobuccal fold can be palpated easily under the skin, as can the anterior nasal spine, the anterior nasal aperture, and the frontal process of the maxilla. Intraorally, it is possible to palpate the canine eminence, the canine fossa (distal to the canine eminence and a common site for facial access to the maxillary sinus), the maxillary tuberosity, and the hamular notch. The maxilla extends as a horizontal plate medially to form the anterior two thirds of hard palate. The horizontal plate of the palatine bone forms the posterior one third of hard palate. The palatine bone has a vertical plate that articulates with the base of the maxilla; it also has a pyramidal process that interposes between the maxillary tuberosity and the pterygoid processes of the sphenoid bone. Mucosal incision at the maxillary tuberosity that extends into the hamular notch may expose the pyramidal process of the palatine bone. Distal to this point, one may expose the medial pterygoid muscle, which takes origin from the tuberosity and the lateral pterygoid plate of the sphenoid. The medial wall of the maxilla begins at the sharp edge of the anterior nasal aperture and extends posteriorly, with a concavity that bounds the nasal fossa and continues distal to the canine. Once there, it forms the medial wall of the maxillary sinus and continues all the way back to the maxillary tuberosity. The medial wall of the maxilla provides attachment to the inferior nasal concha and to the vertical plate of the palatine bone. The opening of the maxillary sinus is found in the medial wall of the maxilla, close to the floor of the orbit. The opening is reduced in diameter by the uncinate process of the ethmoid bone. The latter provides the superior and middle conchae of the lateral nasal wall. The orbital plate of the maxilla forms the floor of the orbit and also the roof of the maxillary sinus. The infraorbital canal carries the infraorbital nerve and vessels, and it forms a ridge that can be seen in the sinus cavity.
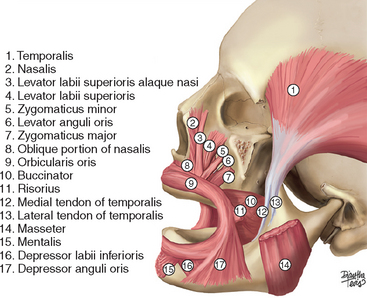
Muscles Attached to the Maxilla
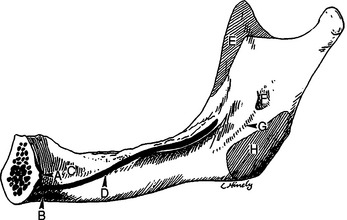
As the maxillary alveolar bone resorbs, the crest of the residual ridge migrates toward the muscles that take their origin from the basal bone of the maxilla. Descriptions of muscles of surgical importance to oral implantologists follow (Figures 22-3 to 22-5).
Buccinator Muscle
The buccinator muscle originates from the base of the alveolar process opposite to the first, second, and third molar of both jaws. This muscle also takes origin from the pterygoid hamulus of the medial pterygoid plate of the sphenoid bone and therefore bridges the gap between the maxillary tuberosity anteriorly and the hamulus posteriorly. Extension of a subperiosteal frame design into the pterygoid plates may interfere with the fibers of these muscles without adding too much to the retention of the implant. When incising and reflecting the mucosa overlying the areas of the maxillary tuberosity and hamular notch before taking impressions for maxillary subperiosteal implants, avoid injuring the tendon of the tensor veli transact muscle, which passes around the pterygoid hamulus. The tendon moves on an underlying bursa whenever the soft palate moves; therefore it may become irritated by the subperiosteal frame and result in inflammation and pain. Fibers of the buccinator and medial pterygoid muscles are also found in the area of reflection. The majority of the fibers of the medial pterygoid muscle originate from the medial surface of the lateral pterygoid plate of the sphenoid bone, whereas the rest of the fibers form the tuberal head, which takes origin from the maxillary tuberosity. Near the pterygoid hamulus, a fibrous tissue raphe or, in some cases, a broad fascialike structure is found between the transaction and the superior pharyngeal constrictor muscles. In some cases, no raphe or fascia is found. Injury to the latter muscle should be avoided during reflection of the mucosa, particularly on the palatal aspect of the area of the hamulus.
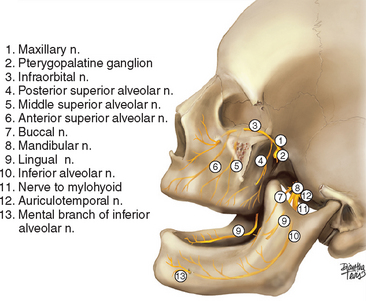
Sensory Innervation of the Maxilla
The maxillary nerve (V2) innervates the maxilla (Figure 22-6). The nerve leaves the middle cranial fossa by passing through the foramen rotundum and appears in the pterygopalatine fossa. It exits the fossa and passes briefly into the infratemporal fossa; from there it enters the floor of the orbit or the roof of the maxillary sinus by passing through the infraorbital fissure. It then exits the orbit via the infraorbital foramen. The pterygopalatine portion of the maxillary nerve provides the descending palatine and sphenopalatine branches. The sphenopalatine nerve enters the nasal cavity from the pterygopalatine fossa by passing through the sphenopalatine foramen. It supplies the nasal cavity and becomes the incisive nerve that supplies the palatine mucosa opposite to the upper six anterior teeth. The descending palatine nerve terminates as the great palatine nerve, which supplies the mucosa of the hard palate, and the lesser palatine nerves, which supply the mucosa of soft palate. These sensory nerves also carry parasympathetic fibers from the sphenopalatine ganglion that innervate the mucous glands of the palate. The infratemporal portion of V2 branches into the posterior alveolar nerve and zygomatic nerve. The latter divides into the zygomaticofacial and zygomaticotemporal cutaneous nerves. The posterior superior alveolar nerve supplies the buccal gingiva, buccal alveolar bone, second and third molars, and two roots of first molar. The infraorbital portion of V2 gives rise to anterior superior alveolar and occasionally middle superior alveolar nerves. These nerves run in bony grooves in the facial wall of the maxillary sinus under the Schneiderian membrane. The nerves supply the sinus wall and the premolars; the canine, lateral, and central incisor on the same side; and also the central incisor at the contralateral side. The infraorbital nerve exits the maxilla at the infraorbital foramen and supplies cutaneous branches to the lower eyelid, side of the nose, and upper lip. Implantologists often need to block V2 or several of its branches. Luckily these can be achieved by an intraoral route. V2 can be reached via the great palatine foramen and descending palatine canal, or via the pterygomaxillary fissure by following the slope of the posterolateral surface of the maxilla into the pterygopalatine fossa.
Palatine Nerve
The greater (anterior) and lesser (posterior) palatine nerves supply the hard and soft palate, respectively. They exit the pterygopalatine fossa through the superior opening of the descending palatine canal, travel downward, and enter the oral cavity by way of the greater and lesser palatine foramina. The greater palatine nerve runs forward in a groove on the inferior surface of the hard palate to supply the palatal mucosa as far forward as the incisor teeth. Here the nerve communicates with the nasopalatine nerve. The nerve supplies the gingiva, mucous membrane, and glands of the hard palate. The greater palatine artery and vein accompany the nerve during its course in the hard palate. As the maxillary alveolar process atrophies, it shifts to the palate and brings the crest of the ridge closer to the groove where the greater palatine neurovascular bundle is found. The restoring dentist should be aware that an incision too palatal to the crest of the ridge in the atrophied maxilla might injure these vital structures. This foramen is entered for a V2 block anesthesia. One may find it by taking a blunt instrument and pressing firmly along the alveolar palatal bone angle. The instrument will depress over the foramen when in the correct position.
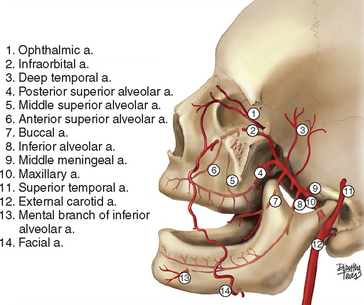
Arterial Supply to the Maxilla
The majority of arterial blood supply (Figure 22-7) comes from the maxillary artery, which is one of the terminal branches of the external carotid artery. The artery starts deep to the neck of the mandibular condyle (mandibular portion) and then proceeds either superficial or deep to the lateral pterygoid muscle (pterygoid portion). It then branches close to the pterygomaxillary fissure, where one branch enters the fossa (pterygopalatine portion). The other branch, called the infraorbital artery, enters the floor of the orbit via the infraorbital fissure; it proceeds in the infraorbital canal and exits on the face by passing through the infraorbital foramen. Branches of the maxillary artery are as follows:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses