Chapter 41 An Implant Is Not a Tooth: A Comparison of Periodontal Indices
The primary function of a dental implant is to act as an abutment for a prosthetic device, similar to a natural tooth root and crown. The restoring dentist designs and fabricates a prosthesis similar to one supported by a tooth and, as such, also evaluates and treats the dental implant similarly to a natural tooth. Yet fundamental differences in the support system have to be recognized. The purpose of this chapter is to compare the periodontal indices for a natural tooth and an osteointegrated implant.
LITERATURE REVIEW
Several dental health criteria have been adapted for implants.1–12 The clinical criterion most commonly reported is the survival rate, or whether the implant is still physically in the mouth or has been removed.2 Proponents of this method say it provides the clearest presentation of the data; critics argue implants that should be removed because of pain, disease, or the inability to be restored still may be maintained yet wrongfully reported as successful. Reports of natural teeth used to support a prosthesis follow a similar criterion: whether the restoration is still in the mouth. Therefore survival rates rather than success rates are the most common method to report the “success” of the prosthesis, whether the prosthesis is supported by implants or natural teeth. A majority of reports that include clinical criteria include mobility, radiographic assessment, and gingival and plaque indices. Subjective criteria of discomfort and patient satisfaction also are mentioned.
The American Dental Association Council on dental materials, instruments, and equipment states that consideration for an endosteal implant should be given to the evaluation of (1) durability; (2) bone loss; (3) gingival health; (4) pocket depth; (5) effect on adjacent teeth; (6) function; (7) esthetics; (8) presence of infection, discomfort, paresthesia, or anesthesia; (9) intrusion on the mandibular canal; and (10) the patient’s emotional and psychological attitude and satisfaction.3,4 Smith and Zarb5 suggested that patient comfort, sulcus depth, gingival status, damage to adjacent teeth, and violation of the maxillary sinus, mandibular canal, or floor of the nasal cavity are not attributable to the material or design of an implant. As a result, they suggest these should be considered separately and should not be computed in the percentage of implant successes. One may reasonably state that factors controlled primarily by the dentist and the psychological attitude of the patient are not conditions influenced by the implant. However, the sulcus depth and gingival status next to the implant indeed may be related to implant design or surface condition. For example, a smooth, polished collar contributes to crestal bone loss, which affects sulcus depth. The implant surface condition may allow bacteria to form readily on the surface after crestal bone loss and may affect the gingival status of the implant.
LONGEVITY
Success criteria for endosteal implants have been proposed previously by several authors, including Schnitman and Shulman,6 Cranin et al.,7 McKinney et al.,8 Albrektsson et al.,9,11 and Albrektsson and Zarb.10 As Box 41-1 shows, the report by Albrektsson et al.9 was specific for implants with rigid fixation and is used widely today. However, the amount of crestal bone lost during the first year may affect the sulcus depth and environment for the longevity of the implant. Yet this criterion is not mentioned in Albrektsson and Zarb’s classification of health. In addition, survival rates suggested in this guideline are low compared with present-day reports and do not consider the prosthesis survival rather than implant longevity.
Box 41-1 Criteria for Implant Success
From Albrektsson T, Zarb GA, Worthington P et al: The long-term efficacy of currently used dental implants: a review and proposed criteria of success, Int J Oral Maxillofac Implants 1:1, 1986.
The consideration of a minimum implant survival rate should be in the context of the final prosthesis’ survival. For example, many early reports indicated that a fixed prosthesis in a completely edentulous arch may be supported by four implants. More recently, the suggestion has been made to fabricate a fixed prosthesis with immediate loading on as few as three or four implants. In a study of 25 patients with 25 prostheses supported by only four implants, there would be 100 implants. A 75% implant success rate would result in 0% prosthesis success, if each patient lost only one implant. An 85% implant 5-year survival rate still would affect almost half the implant restorations. Of course, this survival rate is not acceptable. Implant survival by itself is not an acceptable criterion to evaluate an implant system, and studies must include the restoration. Albrektsson et al.9 have stated that the required implant success rate is a minimum of 85% for 5 years and 80% for 10 years. These success rates are similar to prosthesis success on natural teeth.13 However, the initial proposed criteria do not evaluate the prosthesis and may be unacceptable to the patients undergoing restoration. Implant survival and the associated prosthesis survival rates need to be evaluated together, because the restoration is the most important aspect to the patient.
Dental implant success rates reported in the literature typically do not address prosthesis failure. Instead, as long as the prosthesis may be refabricated, the reported implant success is not affected. More relevant information is gained when longevity criteria include information on the prosthesis. The clinical criteria established by Misch for optimum to satisfactory health for implants also evaluates prosthesis survival, not only implant survival, and suggests a minimum of 90% prosthesis survival for 10 years1 (Box 41-2).
For the patient and doctors involved in treatment, to lose 10% of the implants before fabrication of the prosthesis is far better than to have 5% implant failure after delivery of the restoration.14 The average implant restoration in a partially edentulous patient has three implants as support. A 5% difference in implant survival may affect 15% of the prostheses. In addition, computed data of dental implant survival/success should include all implants inserted, not just the implants restored or those successfully loaded after 1 year.
PAIN
Subjective findings of pain, tenderness, and sensitivity are common dental conditions that the dentist treats as part of a general practice. Pain and tenderness are subjective criteria and depend on the patient’s interpretation of the degree of discomfort. Pain is defined as an unpleasant sensation ranging from mild discomfort to excruciating agony. Tenderness is more an unpleasant awareness of the region. A natural tooth often becomes hyperemic and sensitive to cold as the first indicator of a problem. A tooth with a more serious condition becomes sensitive to heat and painful to percussion, indicating pulpitis. Dental emergencies usually are associated with pain, and the dentist is adept at its diagnosis and treatment planning. An implant rarely is troubled by the subjective criteria of pain or sensitivity. The implant does not become hyperemic and is not temperature sensitive, and the early warning signs and symptoms of a problem may not be present. In addition, pain rarely is associated with the implant after healing. This criterion is less contributory to implant health determination.
MOBILITY
Tooth Movement
The tooth exhibits normal physiologic movements in vertical, horizontal, and rotational directions. The amount of movement of a natural tooth is related to its surface area and root design. Therefore the number and length of the roots; their diameter, shape, and position; and the health of the periodontal ligament primarily influence a tooth’s mobility. A healthy tooth exhibits zero clinical mobility in a vertical direction. Actual initial vertical tooth movement is about 28 μm and is the same for anterior and posterior teeth.15 The vertical movement of a rigid implant has been measured as 2 to 3 μm under a 10-lb force and is due mostly to the viscoelastic properties of the underlying bone.16
Horizontal tooth mobility is greater than vertical movement. A very light force (500 g) moves the tooth horizontally 56 to 108 μm. The initial horizontal mobility of a healthy, “nonmobile” posterior tooth is less than that of an anterior tooth and ranges from 56 to 75 μm, which is two to nine times the vertical movement of the tooth. Initial horizontal mobility is even greater in anterior teeth and ranges from 90 to 108 μm in health.15,17
Muhlemann found that tooth movement may be divided into initial mobility and secondary movement.18 The initial mobility is observed with a light force, occurs immediately, and is a consequence of the periodontal ligament. If an additional force is applied to the tooth, a secondary movement is observed, which is related directly to the amount of force. The secondary tooth movement is related to the viscoelasticity of the bone and measures as much as 40 μm under considerably greater force.
Implant Movement
Rigid fixation is a clinical term that means the absence of observed clinical mobility. Osseointegration is a histologic term defined as bone in direct contact with an implant surface at the magnification of a light microscope.19 Over the years, these two terms have been used interchangeably, and implant abutment support is most predictable with rigid fixation. Rigid fixation indicates the absence of clinical mobility of an implant tested with vertical or horizontal forces less than 500 g, similar to evaluating teeth. Lack of clinically observable movement does not mean the true absence of any movement. A “nonmobile” posterior natural tooth actually moves horizontally 56 to 73 μm. The human eye does not perceive this movement.
The anterior teeth, which often have slight clinically observable movement, actually move approximately 0.1 mm. A healthy implant moves less than 73 μm; thus it appears as zero clinical mobility.16 Lack of implant mobility (IM) does not always coincide with a direct bone-implant interface.8 However, when observed clinically, rigid fixation usually means that at least a portion of the implant is in direct contact with bone, although the percentage of bone contact cannot be specified.20 A mobile implant indicates the presence of connective tissue between the implant and bone.
The implant-bone interface also exhibits lateral movement. Sekine et al.16 evaluated the movement of endosteal implants with rigid fixation and found a range of 12 to 66 μm of movement in the labiolingual direction. Komiyama21 reported 40 to 115 μm of implant movement in the mesiodistal direction under a force of 2000 g (about 4.5 psi) and a labiolingual range of 11 to 66 μm.
Rangert et al.22 suggested that part of this movement may be due to component flexure. However, the greater implant movement in the mesiodistal dimension corresponds to the lack of cortical bone between the implants in this direction compared with the thicker lateral cortical plates present in the labiolingual dimension. The mobility of implants varies in direct proportion to the load applied and the bone density and reflects the elastic deformation of bone tissue. These mobility characteristics corroborate the findings of Fenton et al.,23 who applied a 500-g load for 4 seconds to maxillary anterior teeth and osseointegrated implants. The implants were displaced a mean of 10 μm with a rapid elastic return (less than 1 millisecond), whereas the teeth showed a mean displacement of 57 μm with a prolonged viscoelastic return.
Increased tooth mobility may be caused by occlusal trauma or bone loss. However, increased tooth mobility alone is not a criterion of periodontal health or pathology. Unlike a tooth, for which mobility is not a primary factor for longevity, mobility is a primary determining factor for implant health.24,25 Rigid fixation is also an excellent indicator of the health status because it is an easy, objective test. As such, rigid fixation is usually the first clinical criterion evaluated for a dental implant. The techniques to assess rigid fixation are similar to those used for natural tooth mobility. Two rigid instruments apply a labiolingual force of approximately 500 g.26 The amplitude of tooth mobility may be rated from 0 to 4, where 0 is normal mobility from physiologic movement, 1 is detectable increased mobility, 2 is visible mobility up to 0.5 mm, 3 is severe mobility up to 1 mm, and 4 is extreme mobility including vertical movement. This same gradient may be used for oral implants with slight modification. As Box 41-3 depicts, IM-0 corresponds to the absence of clinical mobility, IM-1 demonstrates detectable increased movement, IM-2 is visible mobility movement up to 0.5 mm, IM-3 is severe horizontal mobility greater than 0.5 mm, and IM-4 is visible horizontal and vertical movement. The implant mobility scale was used frequently for plate form implants because a clinical goal was for slight mobility when joining the device to natural teeth. However, the goal for root form implants always should be rigid fixation and IM-0 status.
Box 41-3 Clinical Implant Mobility Scale
| Scale | Description |
|---|---|
| 0 | Absence of clinical mobility with 500 g in any direction |
| 1 | Slight detectable horizontal movement |
| 2 | Moderate visible horizontal mobility up to 0.5 mm |
| 3 | Severe horizontal movement greater than 0.5 mm |
| 4 | Visible moderate to severe horizontal and any visible vertical movement |
Chances improve to return rigid fixation to an implant if no mobility is noted before the implant is placed into function. An implant with horizontal movement greater than 0.5 mm (IM-3) is at much greater risk than a tooth. The dentist should not restore an implant with any clinical mobility, because the risk of failure is great. However, once the prosthesis is completed and IM-1 develops, the risk is small to decrease almost all stress and evaluate implant mobility after several months. An osseointegrated implant with greater than 0.5 mm horizontal mobility (IM-3) or any vertical mobility (IM-4) should be removed to avoid continued bone loss and future compromise of the implant site.
On occasion, an implant that was rigid may spin in the bone at stage II uncovery, when the implant abutment is threaded into position.27,28 The weak bone-implant interface is broken when the shear forces of adding an abutment are placed on the implant body. If this occurs, the implant cover screw should be reinserted and the implant allowed to “reintegrate” with the bone. The chances are good that 3 additional months of healing will allow the implant to reestablish a bone-implant interface. At the reinsertion of the abutment, a lesser torque is used initially, so the interface does not strip again. After an additional time of progressive loading, the abutment screw may be tightened as usual, although a countertorque method on the abutment is suggested.
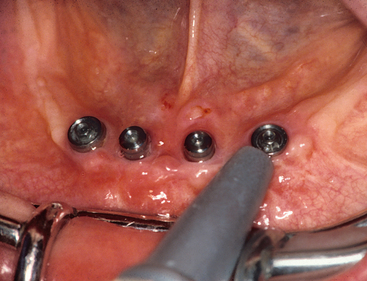
The Periotest (Gulden-Medizinteknik, Bensheim an der Bergstrasse, Germany) is a computer-mechanical device, developed by Schulte, that measures the dampening effect or attenuation degree against objects by developing a force of 12 to 18 N against a pistonlike device, which then measures the distance the piston recoils into the chamber after striking an object.29 A soft surface or mobile object gives higher recordings than a hard or rigid object. The recordings range from negative (8) to positive (50) numbers. Teeth with zero clinical mobility have typical ranges from 5 to 9. The degree or absence of clinical movement around an implant corresponds to values ranging from −8 to +9, or 17 degrees. This greatly aids the dentist’s tactile senses. The bone density around the implant may be correlated with these numbers. This device has been used as a clinical tool to evaluate slight changes in implant rigid fixation or to identify prostheses that become partially unretained30–32 (Figure 41-1). More recently, a nondestructive resonance frequency analysis technique to measure implant stability and osteointegration has been introduced and provides similar valuable information as to the clinical movement and bone density around implants.33,34
CRESTAL BONE LOSS
The marginal bone around the implant crestal region is usually a significant indicator of implant health. Most often the surgical trauma causes little bone loss, but on occasion bone loss may reach several millimeters. The dentist may assess the presence of surgical bone loss before fabrication of the prosthesis. Crestal bone loss after prosthesis delivery is a primary indicator of the need for initial preventive therapy. Early loss of crestal bone beyond 1 mm from the microgap of the abutment after prosthesis delivery usually results from excess stress at the permucosal site or implant crest module design.24,25,35
The level of the crestal bone is measured from the crestal position of the implant at the stage II uncovery surgery. When the abutment is attached to the implant body, approximately 0.5 to 1 mm of connective tissue forms apical to this connection.36 An implant originally placed 2 mm above the bone and another countersunk 2 mm below the bone have a different initial bone loss history after the abutment is attached to the implant. Whenever possible, the implant should be inserted at or above the bone crest to avoid an increase in the sulcus depth around the implant related to the crestal bone loss after abutment placement. Initial bone loss during the surgical healing phase also may vary for submerged and unsubmerged healing protocols.37–43
The initial bone loss beyond the abutment connection and smooth neck region of the implant after function is often a result of excessive stress at the crestal implant-bone interface.24,25,35 The dentist should evaluate and reduce stress factors, such as occlusal forces, cantilever length, and especially parafunction, on observation of initial bone loss after loading. Secondary bone loss around an implant is usually a compound condition created by bacteria and increased stress (a result of parafunction or increasing crown height from crestal bone loss and anaerobic bacteria forming once the sulcus is greater than 5 to 6 mm).44
Several studies report marginal bone loss after the first year of function in the range of 0 to 0.2 mm.19,43,45–48 Adell et al.19 determined that successful implants after the first year of loading had an average 0.1 mm of bone loss for each following year. Cox and Zarb45 observed a similar amount of mean bone loss of 0.1 to 0.13 mm per year after the first year of prosthesis function. Kline et al. reported these numbers represented an average of bone loss measurements. The majority of implants do not lose bone each year.43 However, if one implant in 10 loses 1 mm of bone, the average bone loss is 0.1 mm. One should be careful when an implant is losing bone as shown radiographically. One should suspect occlusal overload, including parafunctional habits. Occlusal overload is especially notable when only one or two implants have lost bone and the other implants in the restoration are not affected.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses