21 RETAINERS FOR PARTIAL REMOVABLE DENTAL PROSTHESES
There exist different philosophies regarding the need for fabrication of cast restorations for abutment teeth before fabrication of a partial removable dental prosthesis (partial RDP). Some authors advocate making such removable prostheses with a minimum of mouth preparation. They do not suggest the routine use of cast restorations for abutment teeth but prefer to modify the remaining natural dentition through enamoplasty and/or addition of composite resin. This has the advantage of reducing both treatment time and expense. Other authors, however, point to the advantages of using cast restorations on abutment teeth, suggesting that through precise shaping of the axial contours of such restorations, the masticatory and retentive forces can be directed more favorably through appropriate use of occlusal rest seats and guide planes. In addition, cast retainers permit incorporation of intracoronal rest seats or precision attachments, which can offer significant esthetic advantages over clasp retained partial RDPs. Use of cast crowns also allows splinting of abutment teeth with resultant reduction of mobility.1
The correct choice of treatment for any patient depends on a thorough history and examination and an accurate diagnosis and prognosis (see Chapter 1). Decisions concerning the restoration of abutment teeth involve many factors—caries, existing restorations, tooth vitality, shape and angulation, oral hygiene, and cost and experience—that must be assessed and evaluated. Only then is the selected treatment likely to achieve the planned outcome that is based on the functional requirements of the patient.
TREATMENT PLANNING
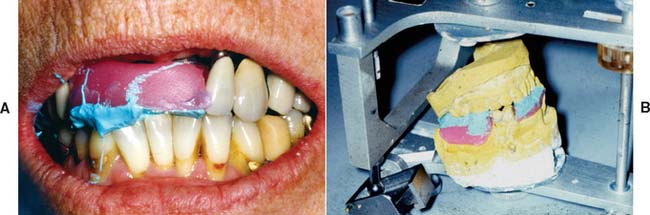
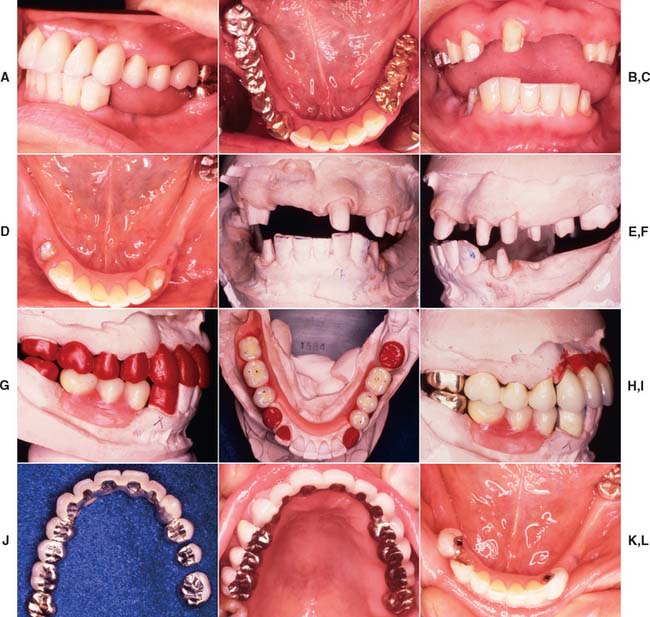
The fabrication of a precisely fitting partial RDP is one of the more challenging tasks in restorative dentistry. Without a careful all-inclusive diagnosis and well-designed treatment plan, the chances of success are minimal. Patients who require a removable prosthesis usually have sustained extensive damage as a consequence of caries, periodontal disease, or trauma and may have extensive fixed and removable prosthodontic treatment needs (Fig. 21-1) They also may exhibit acquired or congenital intraoral defects. As a result of prolonged loss of arch integrity, there may be drifting or tipping, and the occlusion is often less than ideal.
Treatment plans that include a removable prosthesis may require additional diagnostic procedures besides those described in Chapters 1 and 2. Accurate diagnostic casts mounted in centric relation are extremely important. If all posterior teeth are absent, it is much more difficult to relate opposing diagnostic casts, and stable record bases must be made under these circumstances (Fig. 21-2). The necessary degree of stability can be obtained only if such record bases are fabricated on the cast that is to be articulated.
The use of a dental surveyor (Fig. 21-3) is essential during treatment planning for the following reasons:
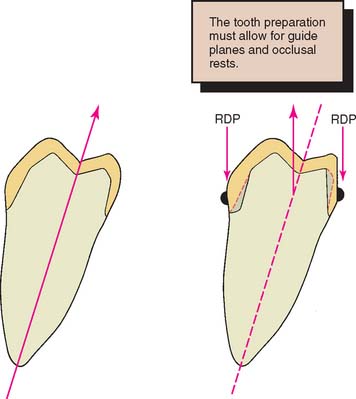
The most appropriate anteroposterior and mediolateral tilt of the cast must be selected. Careful analysis is essential because a compromise between the requirements of an ideal tooth preparation (see Chapter 7) and the requirements for a particular tooth to be used as an abutment to support and retain an RDP is often necessary. The path of placement of the RDP is the most important factor in determining how much tooth reduction is needed to meet mechanical and esthetic requirements simultaneously (Fig. 21-4).
When the diagnostic cast is surveyed, the anteroposterior tilt should be established first. The lateral inclination is then determined. The operator should focus on the relative alignment of selected abutment teeth, any tissue undercuts, and the available occlusocervical dimension for anticipated proximal and reciprocal guide planes. The feasibility of recontouring axial walls and the possible consequences of such recontouring must also be considered. For instance, it may be necessary to treat a malposed tooth orthodontically or endodontically if recontouring is not feasible. Similarly, removal of a tooth that unnecessarily complicates partial RDP design should be considered and carefully weighed against the effect of that decision on the stability of the prosthesis. If future loss of an already compromised tooth would render the partial RDP useless, it may be better to remove that tooth before initiating any prosthetic treatment.
When a patient has lost anterior teeth, the path of placement of a partial RDP should be parallel to the proximal surfaces of the abutment teeth adjacent to the space (Fig. 21-5). This results in superior esthetics because it minimizes the space between the artificial and natural teeth. Sometimes esthetics can be improved by use of a rotational placement path.2
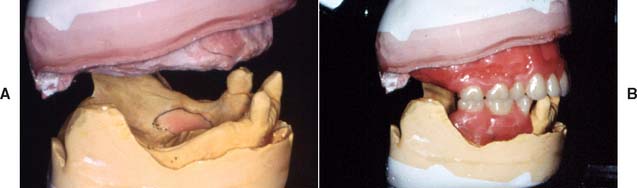
Apparently complex decisions as to the best combination of tooth preparation and path of placement can be greatly simplified through diagnostic tooth preparation, waxing, and denture tooth setting (Figs. 21-6 and 21-7). These trial procedures on diagnostic casts help determine how to achieve the best mechanical and esthetic result without deviating from the principles of occlusion or making excessively bulky restorations that inevitably cause periodontal complications. The concept is to determine the precise end point in regard to occlusion and appearance with interchangeably articulator-mounted casts of the pretreatment and posttreatment condition, before treatment is initiated. The use of such cross-mounted casts (see also Chapter 3) also enables the treatment sequence to be simplified by allowing one arch to be treated at a time. The restorations on the first arch to be restored are fabricated against the diagnostically waxed opposing cast (Fig. 21-8; see also Fig. 3-34).
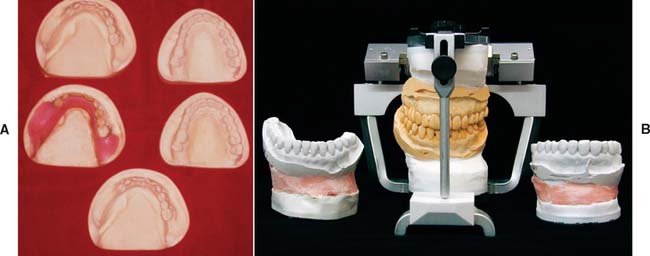
Fig. 21-8 Cross-mounted casts are used to simplify complex prosthodontic treatments. One set of casts is waxed to the end point of treatment, whereas the other set is left unaltered to enable the definitive casts to be mounted. An additional cast is needed for surveying a removable prosthesis. A, Casts needed for treating a patient who required a maxillary fixed prosthesis opposed by mandibular fixed and removable prostheses (see Fig. 21-7). B, The duplicated casts are mounted in the identical relationship on an articulator. Treatment can now be undertaken in phases. First the mandibular teeth are prepared, and a definitive cast is obtained. This is mounted against the maxillary unaltered cast, which is then replaced by the identically oriented, diagnostically waxed cast for the laboratory fabrication of the mandibular fixed prosthesis. (See also Fig. 3-34.)
(A, Courtesy of Dr. J. H. Bailey.)
Prerequisites for Success
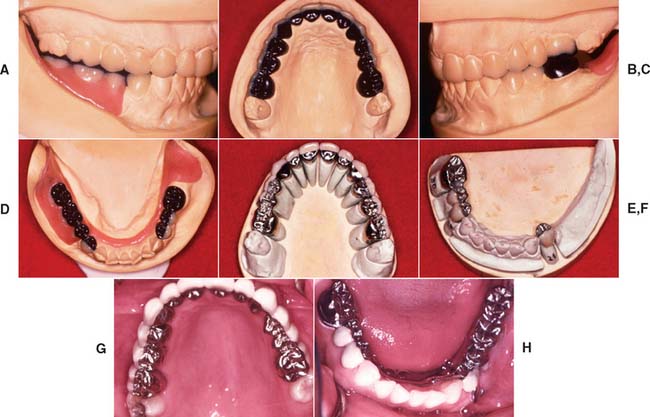
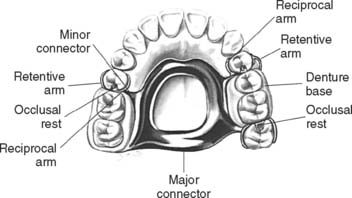
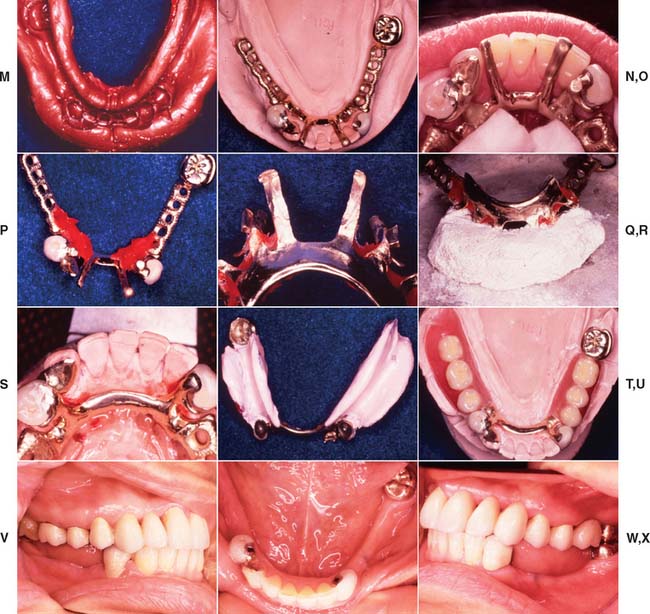
The clinician and laboratory technician must have a good understanding of partial RDP design (Fig. 21-9). An in-depth discussion of the approaches to framework design is beyond the scope of this text. Instead, the modifications that must be incorporated in the cast restoration to accommodate a partial RDP are considered.
Design
Many concepts of partial RDP design have been advocated. Regardless of the concept selected, the operator needs a keen understanding of the requirements placed on fixed retainers. The design should allow the forces developed during placement, removal, and function to be so directed as to cause the least harm to the remaining dentition. The proposed design (Fig. 21-10) should be carefully sketched at the initial treatment planning stage. In general, this reveals any existing problems. Each fixed restoration should be designed to be fully compatible with the removable prosthesis while concurrently meeting all criteria to properly fulfill the functional requirements of mastication and facilitating the performance of oral hygiene. Often, decisions made about the path of place-ment of the partial RDP necessitate removal of additional tooth structure in order to maintain the minimally required material thickness for the fixed prosthesis.

Fig. 21-10 Initial partial removable dental prosthesis design sketched on the diagnostic cast.
(Courtesy of Dr. N. L. Clelland.)
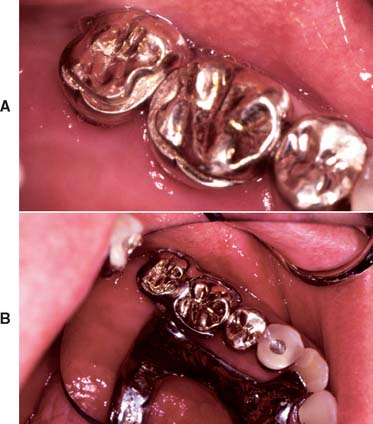
Occlusal rest seat
The rest seat (Fig. 21-11) is the prepared recess in a tooth or restoration created to receive the occlusal, incisal, cingulum, or lingual rest. The occlusal rest of the partial RDP is the rigid extension that contacts the occlusal surface of a tooth or restoration. The occlusal rest of a partial RDP should fit precisely into the corresponding rest seats on the retainers. To reduce laterally directed forces, the rest seats should be spoon-shaped. The junction between the internal aspect of the rest seat and the proximal guide plane should be rounded to minimize stress on the framework and thereby reduce the chance of partial RDP fracture at the occlusal rest–minor connector interface.
Occlusal rest seats are most predictably placed in healthy enamel or cast metal. If they are placed in weaker materials such as amalgam, composite resin, or dental porcelain, fracture or distortion is likely to result. The size of the rest seat has been a matter of controversy. Ordinarily, if crowns are made, a No. 8 round bur produces an ideally sized rest in the wax pattern. On small teeth under normal loading, a No. 6 round bur can provide adequate space (Fig. 21-12). On anterior teeth, a cingulum rest seat should be created to support the removable prosthesis. Rests that are convex mesiodistally and resemble a V-shaped groove labiolingually (Fig. 21-13) have proven successful in clinical practice. This configuration prevents displacement of the abutment while simultaneously assisting in directing forces more parallel to its long axis. Unfortunately, a distinct cingulum rest of adequate size can rarely be placed in the cingulum of an unrestored tooth without penetrating through the enamel.3 Sometimes a pin-retained or resin-bonded restoration4 is used to provide a cingulum rest.* An incisal rest may be used on unrestored mandibular canines (Fig. 21-14). This provides good support for the partial RDP but may be unacceptable esthetically. When a rest is placed on a metal-ceramic restoration, adequate thickness of metal must remain between the lateral walls of the occlusal rest seat and the porcelain-metal junction. About 1 mm is sufficient. Similarly, a minimal metal thickness of 1 mm between the rest seat and the occlusal aspect of the prepared tooth is advisable. To minimize the risk of fracture, an occlusal rest seat should not be placed directly on porcelain.
Minor connectors
The minor connectors of a partial RDP (Fig. 21-15) are the connecting link between the major connector or base of a partial RDP and the other units of the prosthesis, such as the clasp assembly, indirect retainers, occlusal rests, and cingulum rests. They join the rest seats and the clasps to the major connector and should fit intimately against the proximal guide plane on the cast restoration. The guide plane should be as long as possible occlusocervically and should follow the normal configuration of the tooth buccolingually. All proximal guide planes should parallel each other.
Clasp retention
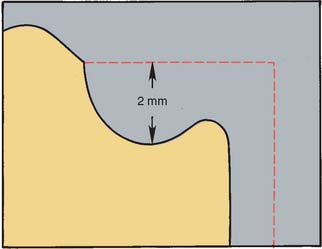
Likewise, the height of contour must not be placed too far occlusally, or binding of the retentive arm may occur during RDP placement. Ideally, it should be within the middle third of the retentive surface of the retainer. A properly contoured surface enables the retentive arm to flex gradually along the path of placement. Only the terminal third of the retentive arm should be placed gingival to the survey line (Fig. 21-16). If more than the terminal third of the retentive arm is placed cervical to the height of contour, this may impede placement and removal of the RDP.
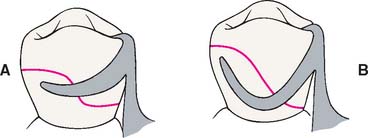
A typical survey line for occlusally approaching clasps has an undulating configuration somewhat reminiscent of the letter S, with its most gingival portion adjacent to the minor connector. If a gingivally approaching clasp is used, the undercut may be immediately adjacent to the proximal guide plane, although with the popular rest, proximal plate, and I-bar (RPI) design it is placed at or mesial to the midline of the tooth.7 Several factors—rest seat location, origin of the clasp, tissue undercuts, and degree of clasp encirclement—influence the actual configuration of the survey line for individual retainers.
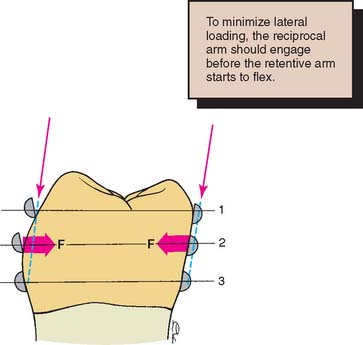
Reciprocation
Reciprocation is the mechanism by which lateral forces generated by a retentive clasp passing over a height of contour are counterbalanced (Fig 21-17). This is usually done by a reciprocal clasp that passes along a reciprocal guiding plane. The reciprocal clasps have two functions: They guide the prosthesis into place upon insertion, and they support the abutments against horizontal forces exerted by the flexing retentive arms. The retentive arms should flex rather than displace the abutments laterally. Guide planes are needed on the crowns to allow for successful reciprocation. These should extend from the proximal guide plane to an area directly opposite the terminal position of the retentive clasp. Reciprocal clasps must contact the guide plane before the retentive arms start to flex, so that the periodontium is protected against excessive lateral loading.
TOOTH PREPARATION
After the proposed path of placement for the partial RDP has been determined and any necessary enamel modifications made, the teeth requiring abutment crowns can be prepared (Fig. 21-18). Making complete crowns is often necessary, but when facial contour does not require modification, partial coverage may sometimes be used.
Path of Placement
Careful planning is required when the path of placement of tooth preparations for RDP retainers is selected. Although conventional crowns generally have a path in the long axis of the tooth, partial RDP retainers may not. Surfaces where both guide planes and reciprocal planes are planned, as well as areas that require survey lines in the gingival third, typi-cally need to be “overprepared” in relation to the ideal conservative technique used on individual teeth. Because of the lingual inclination of mandibular molars, reducing them slightly more in the occlusal two thirds of the lingual axial surface is often necessary to allow the development of lingual guide planes that parallel each other across the dental arch.
Rest Seats
An adequate amount of tooth structure must be removed to allow for a minimum metal thickness of 1 mm in the area of an occlusal rest seat. To achieve adequate reduction, some dentists prepare a rest seat in the tooth before starting the retainer preparation. They then use 1-mm reduction grooves to ensure adequate thickness. Although this approach can work well, problems may occur if it becomes necessary to alter the position of the rest seat during the laboratory phase. Preference therefore should be given to the slightly less conservative approach seen in Figure 21-19 because being able to move the rest seat during the laboratory phase can be extremely helpful. Often esthetic needs, such as the interproximal extent of a cut-back for a metal-ceramic restoration, can be assessed only on the laboratory bench during waxing procedures.
Axial Contours
When a crown is to serve as a partial RDP abutment, modifications may be necessary in the normal axial reduction. The extent of additional axial reduction depends on the RDP design (see Fig. 21-9).
Another possible advantage of providing an abutment crown is the opportunity to shape the axial contours to accommodate the partial RDP clasps within the normal crown contours (Fig. 21-20). Although this allows for a less bulky removable prosthesis contour, it requires additional axial reduction. The use of a precision machine-tool milling device (see Fig. 21-27) is essential for these restorations.
IMPRESSION MAKING
Because of the relative interdependence of partial RDP abutment preparations, a diagnostic irreversible hydrocolloid impression should be made after the preparations have been completed. This is poured in accelerated-setting stone or plaster. The resulting cast is then surveyed and the need for any further modifications is determined; such modifications can then be incorporated with minimum loss of chair time. The same cast can also be used for fabricating the interim restorations (see Chapter 15). A definitive impression is obtained with either an elastomeric or a reversible hydrocolloid technique, as described for conventional restorations (see Chapter 14).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses