CHAPTER 21 Management of Trauma to the Teeth and Supporting Tissues
Atrauma with accompanying fracture of a permanent incisor is a tragic experience for the young patient and is a problem whose management requires experience, judgment, and skill perhaps unequaled by any other portion of the dentist’s practice. The dentist whose counsel and treatment are sought after a trauma is obligated either to treat the patient with all possible means or to immediately refer the patient to a specialist. The oral and emotional health of the young patient is involved, and the child’s appearance, marred by an unsightly oral injury, must be restored to normal as soon as possible to relieve the consciousness of being different from other children. Slack and Jones observed that the progress of children in school and their behavior elsewhere, as well as their psychological well-being, can be adversely influenced by an injury to the teeth that causes an unsightly fracture.1 In addition, the short- and long-term costs associated with managing trauma to the oral and perioral structures can be large. Borum and Andreasen estimate that the yearly cost from traumatic dental injuries in Denmark ranges from US $2 million to US $5 million per 1 million inhabitants per year.2
The treatment of fractured teeth, particularly in young patients, is further complicated by the often difficult but extremely important restorative procedure. Although the dentist may prefer to delay the restoration because of a questionable prognosis for the pulp, often a malocclusion can develop within a matter of days as a result of a break in the normal proximal contact with adjacent teeth. Adjacent teeth may tip into the area created by the loss of tooth structure. This loss of space will create a problem when the final restoration is contemplated. There must often be a compromise of an ideal esthetic appearance, at least in the initial restoration, because the prognosis is questionable or because the tooth is young and has a large pulp or is still in the stage of active eruption.
The International Association of Dental Traumatology reports that one out of every two children sustains a dental injury, most often between the ages of 8 and 12. They suggest that in most cases of dental trauma a rapid and appropriate treatment can lessen its impact from both an oral and an esthetic standpoint. To that end, the association has developed guidelines for the evaluation and management of traumatic dental injuries, which is available at the following website: http://www.iadt-dentaltrauma.org.
HISTORY AND EXAMINATION
The routine use of a clinical evaluation sheet for injured anterior teeth is helpful during the initial examination and subsequent examinations of an injured tooth (Fig. 21-1). The form, which becomes a part of the patient’s record, serves as a checklist of important questions that must be asked and observations that must be made by the dentist and the auxiliary personnel during the examination of the child.
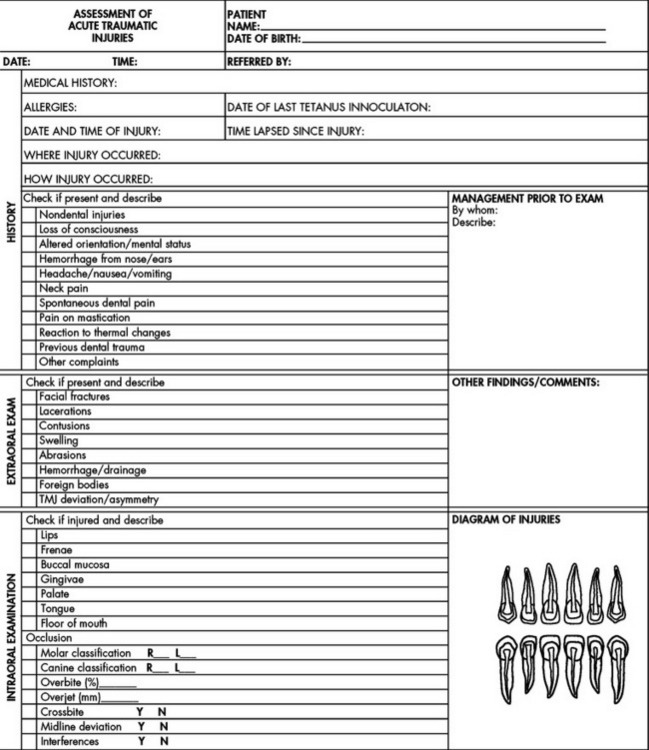
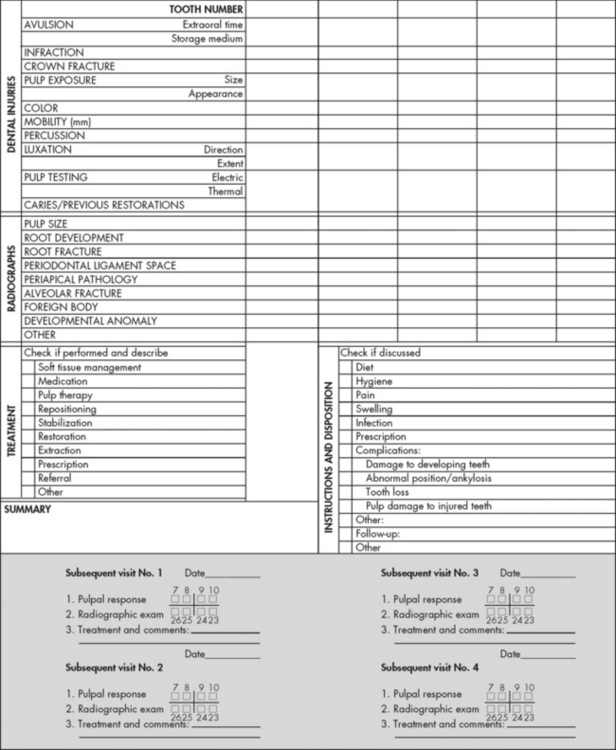
Figure 21-1 Clinical evaluation sheet for injured anterior teeth.
(Adapted from American Academy of Pediatric Dentistry. Pediatr Dent 24(7 suppl):95-96, 2002.)
HISTORY OF THE INJURY
The time of the injury should first be established. Unfortunately, many patients do not seek professional advice and treatment immediately after an injury. Occasionally the accident is so severe that dental treatment cannot be started immediately because other injuries have higher priority. Davis and Vogel emphasized that a force strong enough to fracture, intrude, or avulse a tooth is also strong enough to result in cervical spine or intracranial injury. The dentist must be particularly alert to such potential problems, be prepared ahead of time to make a neurologic assessment, and make appropriate medical referral when indicated without delay.3 The patient should be assessed for nausea, vomiting, drowsiness, or possible cerebral spinal fluid leakage from the nose and ears, which would be indicative of a skull fracture. In addition, the patient should be evaluated for lacerations and facial bone fractures. Obtaining a baseline temperature, pulse, blood pressure, and respiratory rate should be considered as information to be gathered before addressing the dental needs of the patient. Finally, Davis4 recommends a quick cranial nerve evaluation involving the following four areas:
The prognosis of an injured tooth depends logically, often to a great extent, on the time that has elapsed between the occurrence of the accident and the initiation of emergency treatment. This is particularly true in cases of pulp exposure, for which pulp capping or pulpotomy would be the procedure of choice. Rusmah treated 123 traumatized permanent incisors and monitored them over a 24-month period. His findings suggest that the interval between trauma and emergency treatment is directly related to the severity of the injury and the dental awareness of the patients.5 Furthermore, the prognosis of the injured teeth maintaining pulpal vitality diminished when treatment was delayed. The loss of vitality of some injured teeth occurred as early as 3 months and as late as 24 months after the injury, which justifies a long follow-up period after injury.
For practical and especially economic reasons, Andreasen and colleagues have attempted to classify pulpal and periodontal healing of traumatic dental injuries based on the effect of treatment delay.6 They developed three major categories of treatment timing: acute treatment (i.e., within a few hours), subacute treatment (i.e., within the first 24 hours), and delayed treatment (i.e., after the first 24 hours). Unfortunately, there is limited knowledge of the effect of treatment delay on wound healing available in the literature.
Trauma to the supporting tissues may cause sufficient inflammation to initiate external root resorption. In instances of severe injury, teeth can be lost as a result of pathologic root resorption and pulpal degeneration.
CLINICAL EXAMINATION
The clinical examination should be conducted after the teeth in the area of injury have been carefully cleaned of debris. When the injury has resulted in a fracture of the crown, the dentist should observe the amount of tooth structure that has been lost and should look for evidence of a pulp exposure. With the aid of a good light, the clinical crown should be examined carefully for cracks and craze lines, the presence of which could influence the type of permanent restoration used for the tooth. With light transmitted through the teeth in the area, the color of the injured tooth should be carefully compared with that of adjacent uninjured teeth. Severely traumatized teeth often appear darker and reddish, although not actually discolored, which indicates pulpal hyperemia (Fig. 21-2). This appearance suggests that at some later time the pulp may undergo degenerative change terminating in pulpal necrosis.
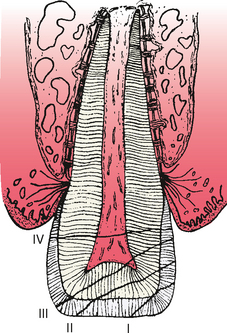
Historically, the Ellis and Davey classification of crown fractures is useful in recording the extent of damage to the crown.7 The following is a modification of their classification (Fig. 21-3):
Laser Doppler flowmetry has been reported to be a significant aid in determining vascular vitality of traumatized teeth by Olgart and associates8 and more recently by Mesaros and Trope.9 Although this technology is not yet affordably priced for dental offices, it may be in the future.
RADIOGRAPHIC EXAMINATION
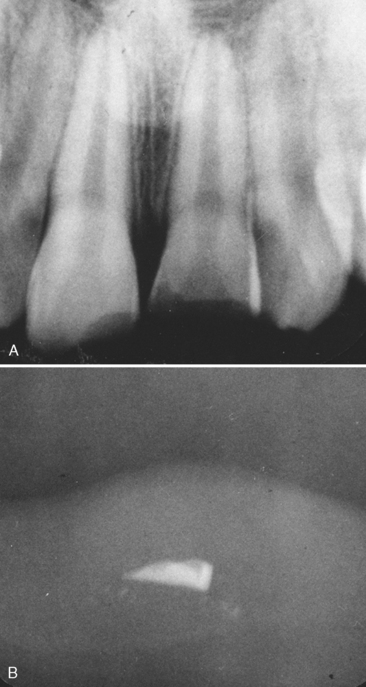
The examination of traumatized teeth cannot be considered complete without a radiograph of the injured tooth, the adjacent teeth, and sometimes the teeth in the opposing arch. It may even be necessary to obtain a radiograph of the soft tissue surrounding the injury site in search of a fractured tooth fragment (Fig. 21-4). The relative size of the pulp chamber and canal should be carefully examined. Irregularities or an inconsistency in the size of the chamber or canal compared with that of adjacent teeth may be evidence of a previous injury. This observation is important in determining the immediate course of treatment. In young patients, the stage of apical development often indicates the type of treatment, just as the size of the coronal pulp and its proximity to the area of fracture influence the type of restoration that can be used. A root fracture as a result of the injury or one previously sustained can be detected by a careful examination of the radiograph. However, the presence of a root fracture may not influence the course of treatment, particularly if the fracture line is in the region of the apical third. Teeth with root fractures in this area rarely need stabilization, and a fibrous or calcified union usually results. If teeth have been discernibly dislocated, with or without root fracture, two or three radiographs of the area at different angles may be needed to clearly define the defect and aid the dentist in deciding on a course of treatment.
EMERGENCY TREATMENT OF SOFT TISSUE INJURY
Injury to the teeth of children is often accompanied by open wounds of the oral tissues, abrasion of the facial tissues, or even puncture wounds. The dentist must recognize the possibility of the development of tetanus after the injury and must carry out adequate first aid measures.
EMERGENCY TREATMENT AND TEMPORARY RESTORATION OF FRACTURED TEETH WITHOUT PULP EXPOSURE
FRAGMENT RESTORATION (REATTACHMENT OF TOOTH FRAGMENT)
Occasionally the dentist may have the opportunity to reattach the fragment of a fractured tooth using resin and bonding techniques. Tennery reported the successful reattachment of tooth fragments for eight teeth in five patients.10 One reattached fragment was subsequently lost as the result of a second traumatic episode. Starkey reported successful reattachment of one tooth fragment on a lower central incisor 2 days after the injury.11
It is not often that the fractured tooth fragment remains intact and is recovered after an injury, but when this happens, the dentist may consider the reattachment procedure. The tooth requires no mechanical preparation because retention is provided by enamel etching and bonding techniques. If little or no dentin is exposed, the fragment and the fractured tooth enamel are etched and reattached with bonding agents and materials. Farik and colleagues have tested the use of the new single-bottle dentin adhesives with and without unfilled resins in the fragment-bonding technique.12 Their hypothesis was that the amount of resin in single-bottle dentin adhesives might not be sufficient to secure an adequate fragment bond. The results of their study showed that all but one of the seven dentin adhesive systems tested should be used with an additional unfilled resin when fractured teeth are restored by reattachment.
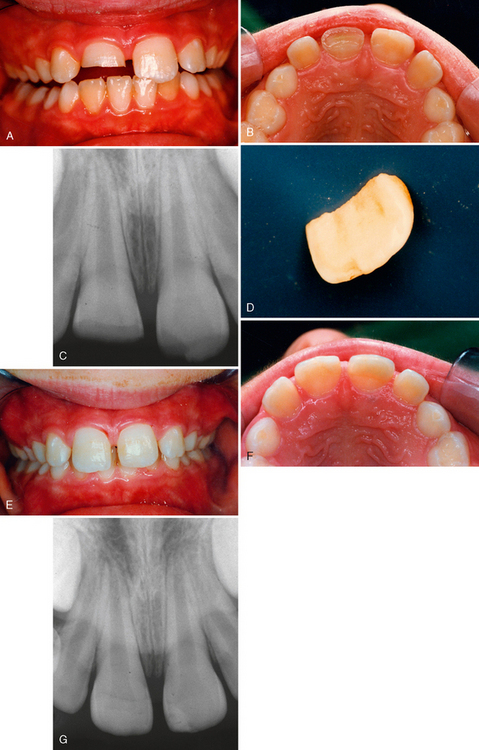
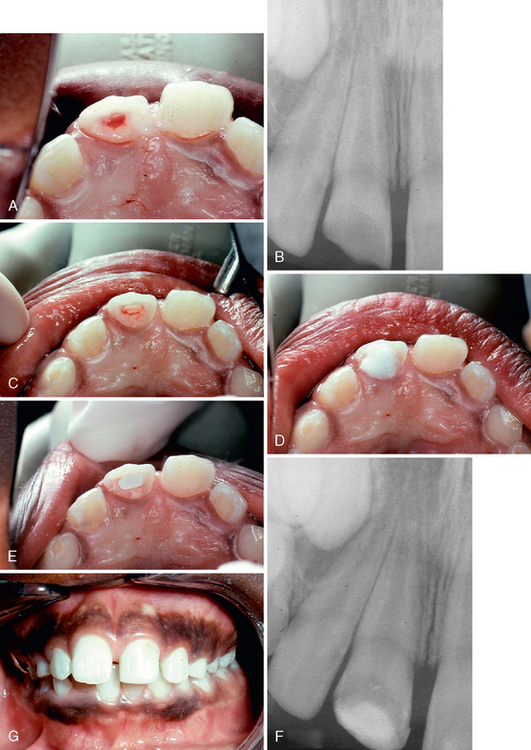
Fig. 21-5 illustrates the successful management of a class II fracture of the maxillary left central incisor in a 6-year-old boy who was treated approximately 1 hour after the injury. After the fragment was trial-seated to confirm a precise fit, the exposed dentin of the fractured tooth was covered with a thin layer of hard-setting calcium hydroxide that was allowed to remain as a sedative dressing between the tooth and the restored fragment. A portion of the dentin in the fragment was removed to provide space for the calcium hydroxide. The fragment was then soaked in etchant, and the fractured area of the tooth was also etched well beyond the fracture site. After thorough rinsing and drying of all etched enamel, the fragment and the etched portion of the tooth were painted with a light-curing sealant material. Although no bonding agent was used here, its use is currently recommended. The selected shade of composite resin was used to fill the prepared void in the fragment, and it was then carefully seated into its correct position and held firmly while the material was cured with the light. Subsequent radiographs and vitality tests indicated that the tooth had probably responded favorably. Croll has reported successfully using light-hardened glass ionomer material for reattaching fragments.13 Kanca reported reattachment of a fragment that successfully capped the pulp using the total-etch technique.14 The restoration was more than 5 years old (replaced once) and was still in place at the time of the report.
Ludlow and LaTurno have reported the success of a fragment restoration for a 13-year-old patient in which essentially the entire clinical crown of a maxillary incisor was fractured away (class IV fracture).15 The remaining tooth was first treated with a root canal filling, and then the pulp canal of the tooth and the enlarged pulp chamber in the fragment crown were used as retentive internal cavities to strengthen the reattached crown.
TEMPORARY BONDED RESIN RESTORATION
The restorative resin material is applied as a protective covering at the fracture site using conventional bonding procedures. As a short-term temporary restoration, it requires little or no finishing and does not need to restore the tooth to normal contour. However, the restoration should cover the fractured surfaces and maintain any natural proximal contacts the patient may have had before the injury (Fig. 21-6). After an adequate recovery period, an esthetic resin restoration may be completed, often without removing all the temporary resin material. However, the outer surfaces of the temporary restoration should be removed superficially before the new material is applied. The margins of the new restoration should extend beyond the margins of the temporary restoration and onto newly etched enamel. The esthetic bonded resin restoration is discussed and illustrated later in this chapter.
TREATMENT OF VITAL PULP EXPOSURES
DIRECT PULP CAP
If the patient is seen within an hour or 2 after the injury, if the vital exposure is small, and if sufficient crown remains to retain a temporary restoration to support the capping material and prevent the ingress of oral fluids, the treatment of choice is direct pulp capping (Fig. 21-7). If the final restoration of the tooth will require the use of the pulp chamber or the pulp canal for retention, a pulpotomy or a pulpectomy is the treatment of choice.
As mentioned in Chapter 19, numerous pulp-capping materials have been studied. Pulp capping with conventional bonding materials is now accepted by many, although the procedure is also considered inadvisable by others. Reports of the use of both mineral trioxide aggregate (MTA) and bone morphogenetic proteins are significant not only for pulp capping but also for general use in endodontic therapy for vital and nonvital teeth.
The prime requisite of pulpal healing is an adequate seal against oral fluids. Therefore a restoration should be placed immediately that will protect the pulp-capping material until the healing process is well advanced (Fig. 21-8). A thin layer of dentin-like material should cover the vital pulp tissue in at least 2 months.
PULPOTOMY
If the pulp exposure in a traumatized, immature permanent (open apex) tooth is large, if even a small pulp exposure exists and the patient did not seek treatment until several hours or days after the injury, or if there is insufficient crown remaining to hold a temporary restoration, the immediate treatment of choice is a shallow pulpotomy or a conventional pulpotomy (Fig. 21-9). A shallow or partial pulpotomy is preferable if coronal pulp inflammation is not widespread and if a deeper access opening is not needed to help retain the coronal restoration.16 Pulpotomy is also indicated for immature permanent teeth if necrotic pulp tissue is evident at the exposure site with inflammation of the underlying coronal tissue, but a conventional or cervical pulpotomy would be required. Yet another indication is trauma to a more mature permanent (closed apex) tooth that has caused both a pulp exposure and a root fracture. In addition, a shallow pulpotomy may be the treatment of choice for a class III fracture of a tooth with a closed apex when definitive treatment can be provided soon after the injury (Fig. 21-10).
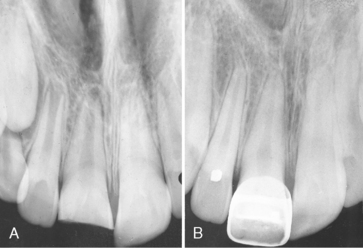
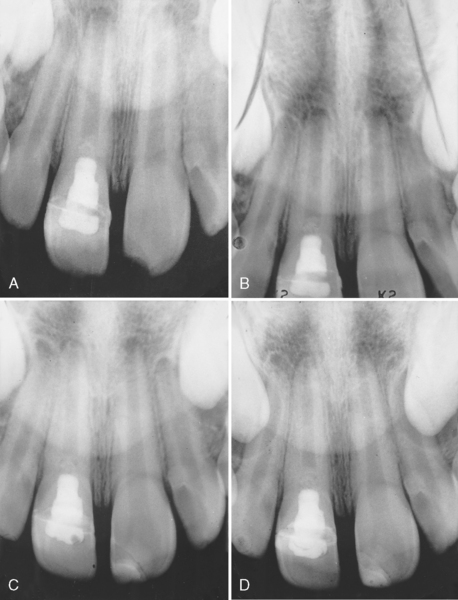
We have observed this calcific degenerative response and agree that it should be intercepted with root canal therapy if possible after apical closure (Fig. 21-11). However, long-term successes after calcium hydroxide pulpotomy in which no calcific metamorphosis has been observed can be documented. We have followed such successful cases for more than 10 years without seeing any adverse results. McCormick has reported one case of a tooth successfully treated with a calcium hydroxide pulpotomy that was observed for more than 19 years and never required further pulp therapy.17
PULPECTOMY WITH ENDODONTIC TREATMENT
In instances of class III or class IV fractures of young permanent teeth with incomplete root growth and a vital pulp, the pulpotomy technique (as just described) is the procedure of choice. The successful pulpotomy allows the pulp in the root canal to maintain its vitality and also allows the apical portion to continue to develop (apexogenesis). For class IV fractures, the eventual restoration may require a post in the root canal. Before this type of restoration is completed, the dentinal bridge that has formed after the pulpotomy can be perforated and routine endodontic procedures can be undertaken in a now completely developed root canal.
THERAPY TO STIMULATE ROOT GROWTH AND APICAL REPAIR SUBSEQUENT TO PULPAL NECROSIS IN ANTERIOR PERMANENT TEETH (APEXIFICATION)
The conventional treatment of pulpless anterior teeth usually requires apical surgery if the teeth have open apices. Many young teeth have been saved in this manner. However, a less traumatic endodontic therapy called apexification has been found to be effective in the management of immature, necrotic permanent teeth. The apexification procedure should precede conventional root canal therapy in the management of teeth with irreversibly diseased pulps and open apices.
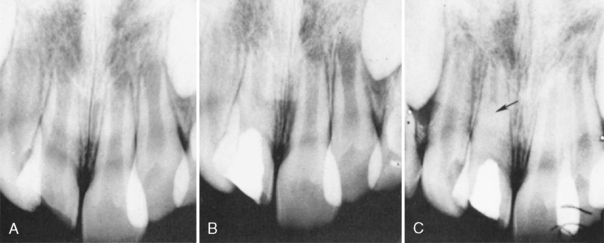
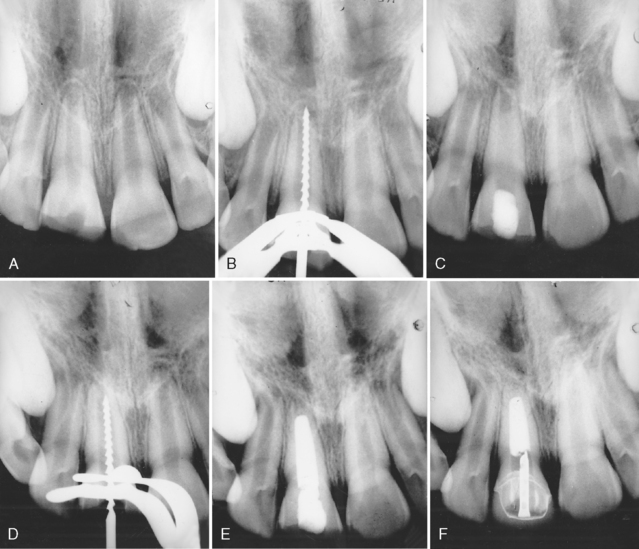
Frank has described a technique based on the normal physiologic pattern of root development that brings about the resumption of apical development so that the root canal can be obliterated by conventional canal- filling techniques.18 The procedure described by Frank and demonstrated to be successful in repeated clinical trials stimulates the process of root end development, which was interrupted by pulpal necrosis, so that it continues to the point of apical closure (Fig. 21-12).18 Often a calcific bridge develops just coronal to the apex. When the closure occurs, or when the calcific “plug” is observed in the apical portion, routine endodontic procedures may be completed; the possibility of recurrent periapical pathosis is thus prevented.
The following steps are included in the technique:
Weine recommends that the apexification procedure be completed in two appointments.19 After instrumentation, irrigation, and drying of the canal during the first appointment, he advises sealing a sterile, dry cotton pellet in the pulp chamber for 1 to 2 weeks. Placing a calcium hydroxide dressing in the canal is optional at the first appointment. During the second appointment, the débridement procedures are repeated before filling the canal with a thick paste of calcium hydroxide and CMCP or calcium hydroxide in a methylcellulose paste.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses