21
Corticotomy and Stem Cell Therapy for Orthodontists and Periodontists: Rationale, Hypotheses, and Protocol
Summary
This chapter is about Professor EO Wilson’s Consilience: the Unity of Knowledge – it synthesizes periodontics and orthodontics, academics and practice, making the ideal practical. The dental specialties, divided by culture, are inseparable in science and justified by art, like the relationship between architects and structural engineers. The interface between these two disciplines focuses on two aspects: what can orthodontics do for periodontology and what can periodontics do for orthodontics? This chapter first reviews salient points of joint management that may have eluded prior papers on the subject and go into some more depth. So orthodontists can use periodontal knowledge and periodontists can answer the needs of the orthodontist. Safe methods of recognizing and avoiding attachment loss are described along with the use of asymmetric eruption when using forced eruption or molar uprighting. The concept of bone morphing is introduced and a rationale is presented that explains gingival recession as a bacterial infection, not tooth movement complication. Finally, a method of quantizing infection, probing efficiently, and assigning infection control management tips is briefly and succinctly presented.
Expanding on this theme, the second part introduces a variation on surgical orthopedics of the alveolus, a previously ignored dental ‘organ’. Then it goes further to describe the theories, rationale, and protocol for stem cell therapy. This pioneering work is an attempt to enlarge the dental arch foundation more quickly, painlessly, and with less tissue morbidity than alternative methods. Finally, the chapter discusses novel ways of thinking that reduce the risk of foundering on the intimidating shoals of new ideas, ideas which seek to eliminate the need for extraction methods.
Then the chapter describes the basic science of stem cell therapy, viz. the introduction of living stem cells in graft form and then moving teeth into the graft with conventional biomechanical protocols. The simplicity of the procedure is explained in step-by-step terms as a synthesis or orchestration of conventional themes in a new and variable score. This takes both specialties into existing biology and new frontiers promised by the twenty-first century. The professional bridge is thus novel and effective, but fortified with logic and taught with helpful themes and analogies. All the while, these data stand firmly on the stable firmament of both traditional and emerging biological science and timeless themes of art.
Introduction
The effects of orthodontic tooth (root) movement on the alveolar bone (at the gross anatomical level) have been well documented in the periodontal literature since the 1970s (Brown, 1973; Ingber, 1974, 1976) and summarized by Mihram in 1997. Recent investigations were conducted in numerous venues, both clinical (Ducker, 1975; Merrill and Pedersen, 1976; Generson et al., 1978; Mostaza et al., 1985; Anholm et al., 1986; Yoshikawa, 1987; Matsuda, 1989; Liou and Huang, 1998; Owen, 2001; Wilcko et al., 2001; Fulk, 2002; Hajji, 2002; Kacewicz et al., 2004; Iseri et al., 2005; Ahlawat et al., 2006; Dosanjh et al., 2006) and experimental (Bell and Levy, 1972; Nakanishi, 1982; Gantes et al., 1990; Kawakami et al., 1996; Twaddle, 2001; Machado et al., 2002; Navarov et al., 2004; Ferguson et al., 2006; Kelson et al., 2005; Oliveira et al., 2006; Sebaoun et al., 2006). Specifically, later papers documented the efficacy of selective alveolar decortication (SAD) to accelerate orthodontic tooth movement, and bone grafts to add volume. An influential clinical description of this successful surgical manipulation was published by Kole in 1959. Interestingly, after the original description by Cunningham in 1894, iterations appeared in the scientific literature (Cohn-Stock, 1921; Bichlmayr, 1931; Ascher, 1947; Neuman, 1955) mostly in German.
The aim of this chapter is to demonstrate how this evolution has opened a frontier to tissue engineering and epigenetic manipulation of the alveolar phenotype. However, first a background summary will build context under the rubric of orthodontic ‘OldThink’ so the unfolding story of twenty-first-century orthodontic theory can evolve with relevance.
Twentieth-Century ‘OldThink’
Bone and Attachment Level in Health and Disease
The periodontium consists of the gingival unit and apical to that, the periodontal attachment apparatus. The gingival unit generally moves with the tooth and contains, when not bleeding on probing, a sulcus of 1–3 mm in health. If everted (prolapsed) by orthodontic force, a sulcus appears as the proverbial ‘red patch of Atherton’ (Figure 21.1). The so-called ‘red patch’ is an eversion (prolapse) of the gingival sulcus, exposing the thin, nonkeratinized epithelium and subjacent connective tissue of the periodontal ligament. This is a potential source of periodontal attachment loss. If the bacterial biofilm around the recession is benign, the everted red patch will mature into marginal gingiva because the marginal gingiva derives from the periodontal ligament and will move with a tooth upon eruption or therapeutic extrusion in health. As Figure 21.1 suggests, recession during tooth movement is caused proximately by the negligence of a patient (despite being well informed) and not necessarily by tooth movement per se. Aleo et al. (1974) showed that destructive endotoxins in dental plaque can inhibit fibroplasia in cell culture. This kind of recession is permanent in the orthodontic patient in the presence of virulent endotoxins and represents the in vivo analog of Aleo et al.’s observation.
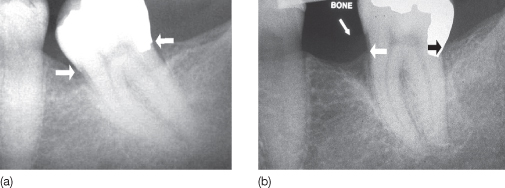
Figure 21.1 Patient VM. (a,b) The red patch (white arrows) noted by British orthodontist JD Atherton (1970). The orthodontist or the assistant usually sees the lesion from perspective (b). (c) Closer inspection reveals a point of vulnerability, or ‘disease-health nexus’, between the white and black arrows. The white arrow marks the coronal extent of a receded periodontal attachment apparatus and the black arrow marks the position it should normally assume in health.
(Source:www.UniversityExperts.com. Used with permission.)

From an orthodontist’s usual incisal and labial views, the everted (prolapsed) sulcus distal to the mesially moving lateral incisor appears curiously benign. But a good clinical scientist cum orthodontist looks beyond the obvious as illustrated in Figure 21.1c. While the clinical recession anteriorly is usually obvious, recession around posterior teeth is not and leads to infected periodontal pockets and permanent bone loss. A vigilant orthodontist will be proactive in looking for such lesions where rapid tooth movement is anticipated and will monitor the patient for any future attachment loss at this vulnerable point. Red patches in posterior sextants are less obvious and thus more pernicious.
These unapparent iatrogenic pockets conceivably would be obscured by hypertrophy and hyperplasia and mark the beginning of progressive periodontitis in the patient’s second or third decade of life. Postoperative periodontal charting and necessary periodontal therapy should therefore routinely follow fixed bracket removal. Moreover, the patient should be followed for 1–2 years to ensure orthodontic and periodontal stability. This subtle but notable phenomenon should be actively looked for in orthodontic cases where sliding or retraction mechanics are aggressively employed and where rapid palatal expansion separates the maxillary incisors rapidly. Recession and progressive disease may be precluded with early diagnosis by the vigilant clinician.
This attachment loss is viewed as ‘bone loss’ in radiographs when about 40% of the alveolar crest bone is decalcified. After decalcification by infection, the organic matrix is lost, usually permanently. The latter event is conveniently called ‘bone loss’ or more correctly, ‘attachment loss’. Sometimes a long junctional epithelial attachment is observed when bone loss has occurred but tissue tonus is firm enough, like a tight collar, to hold onto the root tightly.
Sometimes clinicians are fooled into believing that regeneration has occurred and pockets have disappeared due to gain in regeneration. But actually firm tissue tone and a long junctional epithelium (JE) is only an illusion of regeneration. A long junctional epithelium is faulty because it breaks down suddenly during orthodontic fixed appliance therapy, often to the chagrin of the hapless orthodontist, who believes it may be caused by inferior supportive care or, more naïvely, the orthodontic tooth movement per se. Such ‘unzipping’ can reveal a true pocket that had pre-existed but was treated with ‘deep cleaning’, a nonscientific term for subgingival root planing. Orthodontists should not be fooled into thinking that they are periodontally safe enough to ignore interactive supportive care from professional team members (including the patient). Tooth movement can indeed exacerbate progressive active attachment loss that is uncontrolled.
A shallow sulcus after ‘cleaning’ can be misleading because diagnostic probing of the ‘bottom’ of the sulcus is never achieved with the recommended diagnostic probing force of 20–25 g. (As a practical guide the Hu-Friedy Michigan-O probe weighs about 17 ± 3 g, so excessive force to negotiate a pocket is rarely necessary.) The ‘long JE attachment’ is thought by some periodontists to be less resistant to bacterial breakdown because the root–epithelial interface, a mucopolysaccharide, and hemidesmosomal attachment, is a less formidable defense to bacterial toxins. Other clinicians view it as an acceptable, albeit compromised, anatomical entity which should be maintained as esthetic compromises for surgery around anterior teeth. In health, the crest of the alveolar bone is usually about 1.3–2 mm apical to the bottom of the sulcus; this is called ‘biologic width’, an inviolable anatomical landmark. If the biologic width is encroached upon by an orthodontic band, the level of the bone will re-establish the width as the gingivae recede in response to the new bone level and that can form a nidus for future periodontal pocket formation. Therefore all orthodontic bands should be festooned. The bone crest will follow the movement of the teeth and its gingival unit when the periodontium is healthy.
In disease, however, the tooth moves independent of the crestal bone. Because of this relationship, orthodontic therapy can inadvertently extrude a tooth out of an infected socket and accelerate attachment loss if periodontal infection is not treated (Sanders, 1999). This is why periodontal health is essential during orthodontic therapy and also explains why recession is often evident when inflammation is resolved after debonding. The hypertrophy of tissue edema during therapy often hides the attachment loss and latent recession. This is why the orthodontist’s index of suspicion should always make the entire staff vigilant to occult attachment loss and supportive of collaborative therapy by a periodontist or referring dental professional.
Morphing Bone with Orthodontic Tooth Movement
The orthodontist usually sees fixed appliances simply as ortho-dontic apparati for moving tooth crowns for cosmetic advantage. But, increasingly, they are seen as ortho-pedic devices for restructuring the malleable alveolus bone to more physiological form. This second use is employed for so-called ‘crown lengthening’, i.e. the exposure of more anatomical crown and/or root to facilitate restorative care. This therapy makes use of the independent movement of roots out of the bone. Crown lengthening is achieved in a healthy periodontal attachment apparatus if transseptal, gingival, and superficial crestal periodontal fibers are periodically severed during tooth extrusion. However, this can be a complicated protocol and deserves some concentrated study.
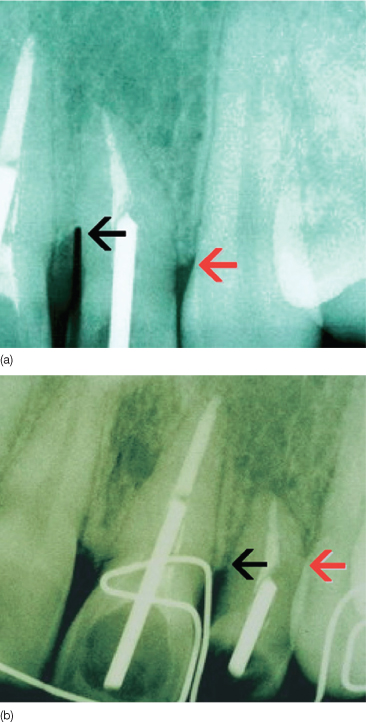
Note that when a molar is uprighted to evert a mesial periodontal pocket, an iatrogenic distal pocket can be created if the molar is not extruded symmetrically and the coronal surface reduced in the process (Figure 21.2). When Ingber (1974) first published the idea of ‘forced eruption’ in 1974, little was known about how to manage the mesial and distal bone level when a pocket appeared on one interproximal side and the other was healthy. That is, how can one unilaterally (e.g. distally) extrude a root orthodontically while maintaining periodontal attachment on the opposite proximal surface. This was explained in subsequent articles and illustrated by Mihram and Murphy (2008). This relationship of the crestal alveolar bone to the root is a critical concept to understand, because it allows correct intuitive judgments by the orthodontist about periodontal health when challenged by a full day of patient demands and biomechanical problems.
Figure 21.2 Note how the attachment level (white arrows) on the mandibular second molar stays at the cementoenamel junction in health (a) but transforms to a gingival (pseudo) pocket of pathological depth on the distal aspect when the mesial pocket (white arrow, (a)) is eliminated by orthodontic uprighting (white arrows, (b)).
(Courtesy of Elsevier. Source: Dr William L. Mihram, Santa Ana, CA USA in Seminars in Orthodontics, December, 2008. Used with permission.)
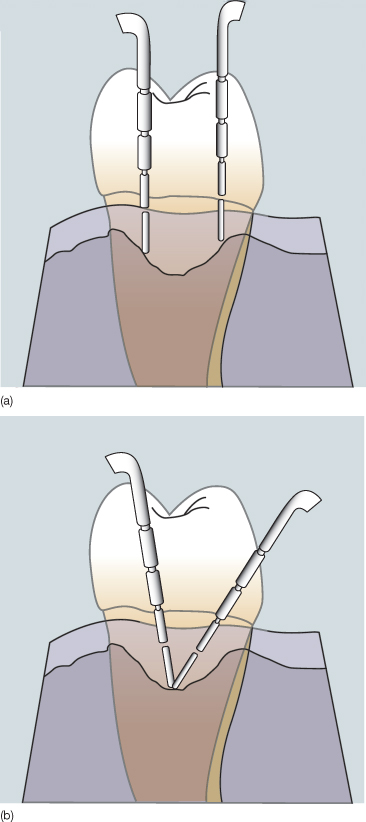
Psychosocial compliance issues unique to orthodontic offices, especially in an adolescent-based practice, are often more daunting in this regard than the pastoral environment of a surgeon’s office. In the orthodontic clinical environment, maintaining a quick wit, born of serious study, is paramount in cases that have asymmetrical bone loss. With a pocket on one proximal side and healthy sulci on the other, only an ‘asymmetrical forced eruption’ can produce a symmetrically ‘lengthened’ crown, and the key to successful molar uprighting. Figures 21.3–21.5 illustrate this phenomenon nicely.
Figure 21.3 No treatment better exemplifies the need for so-called ‘integrated clinical orthodontics’ than molar uprighting. If orthodontic therapy is not employed in a conservative treatment plan, then unnecessarily excessive amounts of bone must be removed during periodontal osseous surgery. Bone coronal to the red line in (a) represents the amount of bone that is removed by standard osseous resection when no orthodontic treatment is used to upright the molar. The coronal and apical white lines in (a) and (b) represent the cementoenamel junction and alveolar osseous crest. The dramatic alteration of alveolar bone phenotype in this iconic representation shows how simple orthodontic aligning and leveling can eliminate the need for osseous surgery. This forms the conceptual basis for alveolar phenotype modification by selective alveolar decortication, periodontally accelerated osteogenic orthodontics, human mesenchymal stem cell placement or viable cell allograft surgical manipulation of the future.
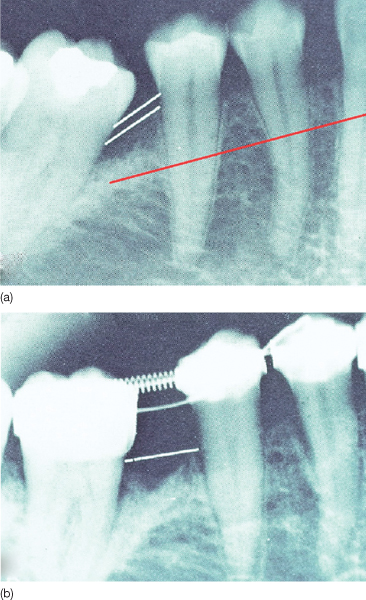
Figure 21.4 (a,b) This image is the clinical correlate of the radiographs in Figures 21.3 and 21.5. Note how the mesial aspect (black arrow (b)) of the molar is now clinically available for preparation, instead of hidden by bone (black arrow (a)). Caries on the mesial surface is often subgingival, even apical to the alveolar crest (blue arrow in (a)) which makes restoration impossible without facilitative (prerestorative) orthodontic therapy. The surgical flap was replaced at the white arrow in b.
(Courtesy of Elsevier. Source: Dr William L. Mihram, Santa Ana, CA USA in Seminars in Orthodontics, December, 2008. Used with permission.)
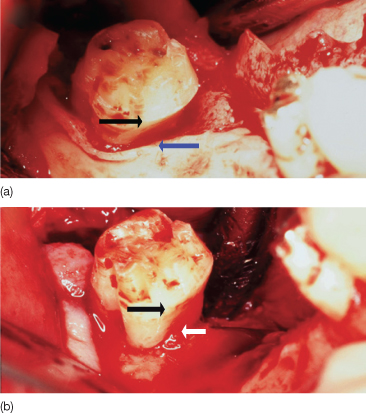
Figure 21.5 (a) Illustrations from JS Ingber’s definitive articles (1974) demonstrating the relationship between the alveolar crest attached to the root in a one-walled infrabony defect (vertical or angular bone loss) and the effect of facilitative extrusion (upper left panel). In the upper right panel, A indicates normal side and B indicates the side with vertical bone loss. In the lower left panel A1 indicates the area where there was no bone loss before and B1 indicates the symmetrical bone level obtained after facilitative extrusion of teeth (combined with fiberotomy or subsequent osseous surgery as needed). Note the occlusal equilibration carried out on the tooth to maintain the occlusal plane. The lower right panel shows the prosthetic crown in situ. The interdisciplinary synergy between the periodontal and orthodontic specialties has made this low morbidity treatment feasible. (b) To eliminate the vertical defect (dotted line) the surgery must involve four more teeth (solid line) to blend the architecture.
(Courtesy of Elsevier. Source: Dr William L. Mihram, Santa Ana, CA USA in Seminars in Orthodontics, December 2008. Used with permission.)
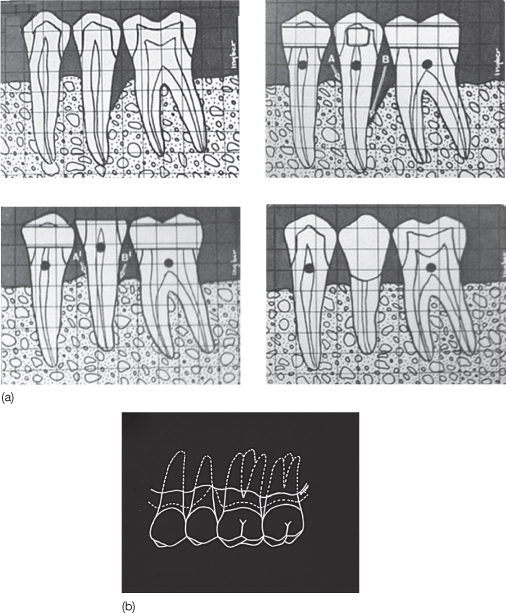
The interdisciplinary synergy between the periodontal and orthodontic specialties has made this low morbidity treatment feasible. The vertical (or angular) bony defect that forms the periodontal pocket on the schematic second premolar must be surgically recontoured (reshaped by removal of healthy bone) if orthodontic forced eruption is not performed. This unnecessary removal of healthy adjacent alveolar bone can be most dramatic. The pathological alveolar crest topography (architecture or shape) is represented by the dotted line in Figure 21.3b. Surgical bone removal must involve four teeth (solid line) to blend the architecture of the alveolar crest into a physiological shape because any abrupt change in the topography of the alveolar crest can cause coronal gingival ‘rebound’ after surgical apical positioning. When the crestal topography is gently sloping, the gingiva stays at its physiological position next to the bone crest and periodontal pockets do not re-form. The morbidity of extraction of the second premolar or periodontal osseous surgery is much greater than simple orthodontic forced eruption as illustrated in Figure 21.3. Another example of asymmetrical forced facilitating proper restoration of the tooth, is shown in Figure 21.6.
Figure 21.6 Note how the arrows match in (b) but are asymmetrical in (a) before asymmetrical forced eruption. As the lateral incisor was forcibly erupted with fixed orthodontic appliances, the soft tissue fibers were severed periodically to the crest of the alveolar bone between the canine and the lateral incisor distal surface. This allowed full eruption of the attachment apparatus (black arrow, (a)) fixed to the mesial surface of the lateral incisor while the distal root surface was therapeutically moved ‘out of the bone’ to provide symmetrical levels of attachment prior to restoration of the lateral incisor. All this complicated treatment could be obviated by the Holy Grail of attachment gain to the cementoenamel junction by stem cell reconstructive surgery in situ at the lateral incisor mesial surface.
(Courtesy of Elsevier. Source: Dr William L. Mihram, Santa Ana, CA USA in Seminars in Orthodontics, December 2008. Used with permission.)
In summary, where infrabony periodontal defects present, asymmetrical forced eruption, producing symmetrical crown lengthening, can also be seen as the simple use of partial fiberotomies. A partial fiberotomy on opposite proximal surfaces keeps bone at consistent level (Figure 21.6, red arrows). The reader is encouraged to read about further techniques and complications by consulting the original journal article by Mihram and Murphy in Seminars in Orthodontics, December 2008, where more orthodontic–periodontic treatments and complications are discussed.
Asymmetrical forced eruption is achieved by periodically severing the attachment on the healthy side of the root, say the distal, while merely scaling and root planing the tooth surface on the side of the infrabony defect, in our example, the mesial in Figure 21.6. Asymmetrical forced eruption therapeutically everts the periodontal pocket on coronal movement of the bone and the creation of an artifactual infrabony defect on the other proximal side, e.g. in Figure 21.6, the mesial and distal aspects, respectively.
The Infected Orthodontic Patient
The essence of periodontal–orthodontic management comes down to understanding alveolus physiology and managing infection even if that management is as mundane as recommending a modern floss holder designed for orthodontic patients (see www.platypusco.com). But the periodontal–orthodontic interface is often more complicated than that and the modern, erudite orthodontist ignores this scientific realm only to his or her detriment since excellent reviews of salient issues are replete in the literature and have been authoritatively summarized as recently as 2008 by Palomo et al. (2008). What these particular authors implicitly argued was that the human mouth is impossible to sterilize, so in the spirit of ‘universal precaution’, all patients are considered always infected, more or less. So the most important issue is this: given the ubiquitous and constant field of infected tissue in which the orthodontist operates, how does one minimize irreversible tissue damage? Since the authors published their survey, a number of pharmacological agents and periodontal ‘friendly’ accoutrements have become more widely accepted by practicing orthodontists.
The in situ pharmacologic agents are particularly noteworthy. When used prudently they are legitimate and effective, but short-acting, therapeutic adjuncts to scaling and root planing. Over time they represent an excellent investment, because they are effective in preventing or mitigating severe exacerbations of latent disease. When using any pharmacological anti-infective medium, it is critical to remember that the ultimate goal of any antibacterial therapy is to make a niche for commensal organisms which will ‘crowd out’ more virulent pathogens. But long-term reliance on pharmaceuticals risks the development of bacterial strains resistant to any pharmaceutical. Because of this limitation, most periodontists prefer that patients use mechanical methods of dental plaque (bacterial biofilm) removal, daily and assiduously.
Benign commensal bacteria are relatively welcomed residents when they limit their reversible damage to the gingival unit. But virulent pathogenic forms and commensal organisms cannot be well distinguished in oral bacterial biofilms. Therefore, it is argued that universal precaution, similar to that used in other infection-prone environments should be employed with all orthodontic patients. The key to success is to keep bleeding on probing (BOP) to a minimum. Since the task of infection control rests on undependable patient compliance, every orthodontic patient should be informed of the risks of periodontal damage and explicitly encouraged to participate in ‘infection control’ by a periodontist, dentist, dental hygienist, and other trained para-professionals during fixed appliance therapy. Even prior to bracket placement an ‘oral infection control’ consultation should be made with an informed and competent professional for scaling and root planing, comprehensive charting, continually supportive oral hygiene instructions and the application of a labial fluoride varnish. (Note how the word ‘infection’ is used instead of trivializing euphemisms such as ‘a little inflamed’ or ‘slight swelling’.)
During all orthodontic treatment with fixed appliances, fluoride therapy should continue every 3–6 months depending on the degree of infection and fluoride varnish should be reapplied every 6 months around the bracket perimeters. Also, there is little need to remove archwires if the treating professional is well trained and experienced. Generally, taking off archwires and replacing them just for oral hygiene prophylaxis or oral hygiene method instruction is inconvenient to patients and interferes with compliance. To modulate infection control, usually a bleeding index (percentage of provoked sulci that bleed on probing) of less than 25% will keep patients safe.
Bone loss, or technically attachment loss, is the hallmark of periodontitis and may not be amenable to regeneration depending on the pattern of destruction, the patient’s individual biological capacity for regeneration, preference, and personal compliance. Individual patients may demonstrate sudden bone damage during orthodontic care so periodontal probing should be done every 6 months, but preferably not by a preoccupied orthodontist as illustrated in Figure 21.7.
Figure 21.7 Probing at arbitrary points such as line angles (a) may miss defects such as two-walled infrabony defects, commonly referred to as ‘craters’ (b).
(Courtesy of Elsevier. Source: Palomo L, Palomo JM, Bissada NF [2008] Salient periodontal issues for the modern biologic orthodontist. Seminars in Orthodontics 14: 229–45. Used with permission.)
A common error, which misses the craters, is measuring at the line angle of the tooth and not advancing the probe far enough interproximally, directly apical to the contact point. The periodontal probe is ‘walked’ on the bottom of the sulcus or pocket and angled approximately 20–30° from the vertical axis (Figure 21.7b) between the teeth. This allows the clinician to follow the attachment around the tooth and reach the depth of the pocket that may be more clinically occult and dangerous to future periodontal health. Probing error is 1 mm, making an interexaminer calibration necessary, periodically. For the busy orthodontist, a screening by probing only interproximal surfaces will take less than 2 minutes, enjoys a high correlation with comprehensive probing techniques, and lends a laudably sober note to any orthodontic regimen.
Gingival Enlargement
Orthodontists should take a collaborative approach to treatment planning, to achieve periodontal health and maximum esthetic outcomes, because altered passive eruption, hypertrophy, gingival hyperplasia, and true attachment loss may conspire to complicate treatment in the presence of inflammation and compromise the final esthetic result. Note that even a pseudopocket (gingival pocket) produced by gingival enlargement is a pathological entity that can lead to true attachment loss and periodontal bone loss, long after an adolescent is dismissed from orthodontic therapy. Therefore, the orthodontist should delegate a ‘post-debonding inspection’ to a responsible colleague or scrutinize the orthodontic patient’s periodontal health during the retention period. Although the patient often does not make the connection between gingival pocket formation as a teenager and bone loss in the late 20s–30s, the ethical obligation remains with the referring doctor, the orthodontist and the periodontist to maintain periodontal and gingival health as best as possible during and after fixed appliance therapy.
Increased public awareness and the introduction of clear aligners have helped reduce iatrogenic risk in the child and adolescent in recent years. But at the very least, the orthodontist has both an ethical and legal duty to inform the patient of the risks. Then the proximate cause of any attachment loss is the patient’s negligence in not following directions. To this end, the American Board of Orthodontics (ABO) under the visionary leadership of Dr Grubb (2008), recommended a full periodontal charting and radiographic diagnostic series for patients of 18 years or older, in order to pass the board certification examination. In some American regions, managed care companies even compete by also requiring orthodontists to record periodontal and gingival pocket depth before, during, and after orthodontic therapy, in children, adolescents, and adults. Despite the criticism about the incursion of corporate insurance companies into traditional diagnostic and treatment prerogatives of orthodontists, they can hardly be criticized when such forward-thinking policies are established by the managed care stakeholders. But such leadership and visionary standards should rightfully be initiated by orthodontists, not corporations.
In a recent landmark study, Waldrop (2008) assessed the prevalence of gingival enlargement (altered passive eruption, hypertrophy, and hyperplasia), a harbinger of pocket formation in orthodontic patients. The same patients were studied 5 years after treatment, and the need for periodontal plastic surgery and esthetic crown lengthening was documented. Waldrop discovered over 60% of treated patients had inferior smiles due to gingival enlargement.
When the gingival margin fails to secure the cementoenamel junction of all teeth, surgical correction should be employed with a flap procedure. We contend that the case illustrated in Figure 21.8 is not finished according to twenty-first century standards of periodontics or even orthodontics until the gingival problems are addressed. In this case, one cannot distinguish whether the gingival enlargement is due to a transient hypertrophy, permanent hyperplasia, or altered passive eruption (gingiva and alveolar bone crest). Moreover, the gingival pockets created by this enlargement cannot be distinguished from the incipient attachment loss (even with radiographs) that follows it. Even negligent patients, concerned only about superficial cosmetics, can understand that cases such as Figure 21.8 are not finished and will commonly complain about ‘showing too much gum’. With sophisticated twenty-first century patients making such observations, it is necessary for the modern orthodontist to treat with a team of supporting professionals during mechanotherapy. That is the essence of multidisciplinary care and ‘integrated orthodontics’, both administratively and intellectually. The case is ‘finished’ when the gingival margin approximates the cementoenamel junction (Figure 21.9). Only then is the patient fully informed of all treatment options and collaborative supportive therapy.
Figure 21.8 An unfinished finished case from an orthodontic as well as a periodontic perspective. Please note that the occlusion is not well settled and there are inconsistent gingival margins along with hypertrophic areas.
(Courtesy of Elsevier. Source: Waldrop TC (2008) Gummy smiles: The challenge of gingival excess, prevalence and guidelines for clinical management. Seminars in Orthodontics 14: 260–71. Used with permission.)

Figure 21.9 (a–d) The proper method of re-establishing the physiological biological width and reducing gingival enlargement associated with orthodontic fixed appliance therapy. This precise tissue manipulation and management of underlying bone tissue cannot be achieved with a laser.
(Courtesy of Elsevier. Source: Waldrop TC (2008) Gummy smiles: The challenge of gingival excess, prevalence and guidelines for clinical management. Seminars in Orthodontics 14: 260–71. Used with permission.)
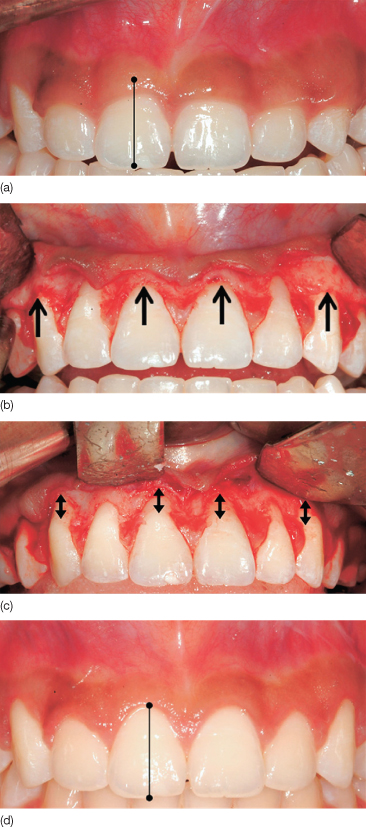
Naïve, but well-intentioned, doctors may use a gingivectomy to solve this problem, but even with hand-held lasers, this is unwise because few understand how ablative a gingivectomy really is. Laser therapy relies on ill-conceived notions that only soft tissue is redundant or misplaced. However, one cannot know for sure if the enlargement is a singular hyperplastic phenomenon or combined with altered passive eruption. In the latter case, lasers cauterize, can destroy biological width, and even alveolar crestal bone. Then pockets or recession can manifest years after debonding.
As a matter of fact, gingivectomies have very little role in modern periodontology, especially with infrabony defects, and have not been routinely used by enlightened periodontists for over 50 years. This is because of reconstructive limitations and the ablative nature of the surgery. The wise orthodontist is ill-advised to undertake such surgeries, to ‘remove redundant tissue’ or ‘take off scar tissue’, without first consulting a certified periodontist familiar with these biological phenomena, and fully informing patients. Shared knowledge ensures shared risk. Once these salient periodontal–orthodontic issues are realized and well managed, the twenty-first century orthodontist is competent to enter the stage of dentoalveolar tissue engineering and the burgeoning realm of stem cell and gene therapy.
Orthodontic ‘NewThink’: the Age of the Stem Cell
In the past decade, professional societies and international academic workshops have witnessed advancements in both genetics and cell biology, which, conjoined, open spectacular vistas for biologists and clinicians alike. The entire human species is producing a kind of ‘perfect storm’ of intellectual growth with a plethora of historic opportunities, literally the dream of humankind. The new generation of orthodontists is positioned perfectly to become the specialists of facial tissue engineering, carrying on the legacy bequeathed to us by selfless educators and financial patrons. It is within this vision that the proposals for stem cell therapy are posited, the protocols are explained, and a new legacy is dedicated.
Definitions
Stem cells are generally defined as primitive cells that mature into specific-function cells. They are components of the viable cell-allograft, discussed in this chapter, with other types of bone forming cells in a processed bone matrix. The collection of precursor cells in the matrix provides many types of potentials which in fact contribute to a collective ‘stem cell’ function. While the definitions below are generally accepted, stem cell therapy (SCT) is young and definitions may take on new connotations in the future. So the astute clinician should be intellectually vigilant to the nuances of meaning.
The term ‘stem cell’, like the words ‘love’ and ‘nice’ has, unfortunately been so over-used that it has lost precise universal meaning. In one strict sense, the only ‘true’ stem cell is the fertilized ovum or one subjected to parthenogenesis. And more informally, a preosteoblast is, in a sense, a ‘stem cell’ because it can differentiate further into an irreversibly mature osteoblast. So, one must make a distinction between cells that undergo maturation and those which can give rise to more daughter cells as well as differentiated forms. Given this state of syntactical affairs, for the purpose of this reading, the terms of ‘stem cell’ therapy will be used as follows:
- Totipotent is the ability to give rise to all the cell types of the body plus all of the cell types that make up the extraembryonic tissues such as the placenta.
- Pluripotent is the ability to give rise to all of the various cell types of the body except extra-embryonic tissues such as placenta components.
- Multipotent is the ability to develop into more than one cell type of the body.
- Stem cells are cells with the ability to divide to produce a fully functional mature cell capable of specific functions in tissue. Generally stem cells have the ability to divide to give rise to both daughter cells and more specialized function cells. In contrast, osteocytes and fibroblasts do not change into more specialized cells naturally. SCT can be local or systemic.
- Mesenchymal stem cells (MSCs) are non-blood adult stem cells from a variety of tissues. Although it is not clear that MSCs from different tissues are the same, they are multipotent for mesenchymal tissues derived embryologically from mesoderm. hMSCs are human MSCs.
- Osteoprogenitor cells (OPCs) are cells dedicated to producing osteoblasts but with more surface markers that allow them to be distinguished from MSCs.
Background and Rationale
SCT rests upon methods of alveolar bone preparation that induce a temporary, reversible, non-pathological osteopenic state. These are collectively referred to with the term ‘surgically-facilitated orthodontic therapy’ (SFOT). It specifically refers to alveolar surgery that achieves an optimal response to orthodontic therapy, by selective decortication and grafting.
This is a temporary reduction of the organic and mineral content of the alveolus around the moving tooth root. Generally this alveolus manipulation will safely ensure that the tooth moves 200–400% faster than with conventional orthodontic methods, with more stability, and less inflammation. The exact nature of histological, cytological, and intracellular orthopedic effects from SFOT in the alveolus remained enigmatic until controlled studies of tissue behavior appeared in the 1980s. Further validations of historical anecdotal claims of efficacy were added at the beginning of the twenty-first century and continue to emerge in the osteology literature.
Critical analysis of selective alveolar decortication (SAD) was formally published through the pioneering work of the gifted Professors Wilcko and Ferguson at Case Western Reserve University, St Louis University and Boston University at the turn of the twenty-first century. Then, by the addition of a bone graft to selective alveolar decortication (SAD), periodontally accelerated osteogenic orthodontics (PAOO) extended the scope of orthodontics into the world of clinical tissue engineering (note: where periodontal considerations are not relevant, the truncated term accelerated osteogenic orthodontics (AOO) is often substituted for PAOO. PAOO and AOO are trademarks of Wilckodontics Inc., Erie, Pennsylvania, USA.). PAOO demonstrates that one may re-engineer a stable alveolar bone phenotype to accommodate dental arch expansion with impunity. We translate this legacy into the science of hMSC therapy merging the clinical biomechanics of SFOT with the mechano-biologics of modern osteology and medical orthopedics.
Figure 21.10 demonstrates how progressive improvement in engineered facial growth can have dramatic effects with simple periodontal surgery even when orthognathic surgery is rejected for mandibular retrognathism. Although it is doubtful that the mandibular corpus has been altered, tissue engineering changed the form of the alveolus bone. These surgeries provided not only more stable dental alignment but also satisfactory facial form alternation. The patient was treated with two PAOO surgeries sequentially over a total treatment time of 18 months. The surgery did not involve orthognathic surgery, hospitalization, or general anesthesia, but rather outpatient periodontal surgery under intravenous sedation.
Figure 21.10 (a–c) Patient MK demonstrates progressive improvement with engineered facial growth. Orthognathic surgery was rejected as an alternative for this case of mandibular retrognathism.
(Source: Images courtesy of the surgeon, Professor M Thomas Wilcko, Case Western Reserve University, School of Dental Medicine, Cleveland, Ohio, USA. Used with permission.)
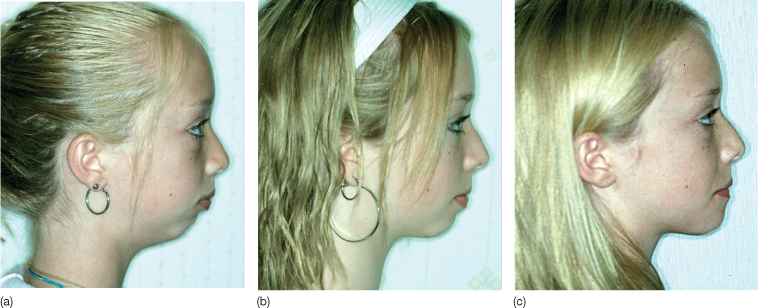
PAOO protocols reduce the need for premolar extraction with phenotype alteration but can also alter facial form without orthognathic surgery. This is done by epigenetic manipulation, effectively validating the tenets of the functional matrix hypothesis (FMH) (Moss, 1997a–d). The FMH explains that the root of a tooth acts as a template or ‘functional matrix’ for neo-morphogenesis of the alveolus bone.
After pioneering research at Loma Linda University, worldwide popularity of the Wilcko–Ferguson–Moss theses in the first decade of the twenty-first century had grown so quickly that the periodontal departments of some American universities, such as Case Western Reserve University in Cleveland, Ohio, and the University of Southern California, in Los Angeles, California, have incorporated PAOO into their standard postdoctoral curricula. This scholastic elevation challenged established therapies with a more cost-effective, healthier, and more benign outpatient science. By extrapolating these data and clinical impressions, what the future holds is not merely faster, better, and safer smile design, but rather nothing less than the intraoral, scarless, designer ‘face engineering’.
Epistemological Issues: Choice and Clinical Styles
Slowly, as the dogma of alveolar immutability surrenders to modern concepts of phenotype plasticity, the alveolus is emerging as a malleable entity requiring new theories of morphogenesis and mechano-transduction. This paradigm is defined by the dynamics of bone healing and genetic expression to a pre-selected form, depending on root position (Murphy, 2006). This ‘NewThink’, a novel way of studying what orthodontics may become, evokes doubts in the minds of some who defend categorical mandates for premolar extraction. In contrast, other contemporary clinicians propose that the rationale for routine premolar extraction should be seriously reassessed. In many North American orthodontic practices, the percentage of extraction cases is dropping to less than 10%. Besides providing good science to non-extraction treatment plans, other biological advantages to PAOO and SCT are the reduction of bacterial damage caused by prolonged orthodontic care, and the notorious relapse potential of fixed appliance therapy (Little, 1993; Little et al., 1998; Oliveira et al., 2006).
Since conventional biomechanics does not alter bony phenotype, innovations are slowly replacing old paradigms with a new epistemology. Conventional dental techniques will always have their place, but cannot totally define the specialty due to the severe limitations mentioned above. SCT prevents or mitigates the severity of side effects and thus earns its place in the pantheon of legitimate care. Even modern periodontal regeneration cannot match these achievements of orthodontic SCT. Periodontal bone grafting merely re-establishes the original phenotype, passively. But, orthodontic tissue engineering and SCT achieve permanent phenotypic change, pro-actively with viable cell dynamics and local immunosuppression. Thus, the challenges of molecular biology are making the study of orthodontic tooth movement at one time more difficult and yet vastly more interesting. Regardless of the perceived difficulties, SCT at least minimizes the unfortunately narrow ‘arts and crafts’ stigma carried by many orthodontic practices.
The ideas in this chapter are a natural extension of ongoing research efforts, and a synthesis of both manifest clinical need and contemporary hMSC science. Ironically, despite the sophisticated rationale, the actual procedures necessary to attain these vaunted goals can be achieved with a simple periodontal surgery, which is often performed by first-year postdoctoral dental students.
The key to success lies not in a particular material or surgical procedure, but rather in the orchestration and timing of traditional protocols, viz. simply moving dental roots in a field of healing tissues and mechanically strained bone. In wound healing, it appears that strained bone reacts differently from the steady-state bone, which the orthodontist usually encounters. Healing wounds recapitulate regional ontogeny and that ontogeny responds to local environmental (epigenetic) perturbations, e.g. optimal orthodontic force, to define phenotype change via stem cell differentiation. Some orthodontists may criticize SCT as unnecessarily morbid. However, considering the ablative nature of tooth extraction and its deforming effects on facial form, the minor side effects of superficial periodontal surgery (1–2 mm beneath the mucosal surface) compare most favorably for facial esthetics enhancement as in Figure 21.10.
Interestingly, the evolution of thought driving the synthesis of orthodontic tissue engineering is not the dogma of new autocratic professional authorities, but rather sensitivity to patient preference, respect for modern dental standards, and contemporary global definitions of facial esthetics. Specifically the use of living stem cells to regenerate original phenotype damaged by infection or to change phenotypic form and mass, presents new evidenced-based and positive options to any prudent clinician who contemplates dental arch advancement or expansion. Hence it is an educational imperative (Nowzari et al., 2008).
/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


