6
Anomalies in Growth and Development: The Importance of Consultation with a Pediatrician
Summary
Growth and development of the craniofacial complex can be altered by a number of factors including the presence of harmful habits, pathological conditions, and medical problems. The goal of orthodontic treatment is to promote the most favorable craniofacial growth and development and to restore it to its optimal status. For this purpose, orthodontists must rely on consultation with pediatricians for identification of existing diseases and for tailoring treatment according to their patients’ conditions. We have assumed that the reader has a good knowledge of normal craniofacial growth, and therefore this chapter focuses on the importance of the interaction between healthcare professionals and highlights instances of anomalies of growth and development requiring consultation with a pediatrician.
Introduction
Pediatricians can play an important role in promoting oral healthcare, and their advice regarding dental procedures or therapies may be solicited. However, a large percentage of the lower socioeconomic population does not have access to a regular dentist. Pediatricians have frequent contact with families during routine preventive visits in the childhood years of life and are in a position to advise families about the prevention of oral diseases in their children and to refer them to an adequate professional. It is important to educate pediatricians with knowledge of craniofacial growth, which may enhance the implementation and eventual success of preventive measures.
There are some recognized problems and habits that should be identified early and discouraged, to allow for optimal craniofacial growth and development, and some that require early referral to the orthodontist. These issues will be discussed in detail in this chapter. Conversely, the orthodontist may be in a position of seeing a patient with craniofacial deviations indicative of medical problems. In the latter cases, the orthodontist should understand the implications of the medical problems in order to formulate an optimal, individualized treatment plan. He or she should also work in close relationship with the pediatrician for elimination of possible causes of harmful craniofacial growth and development.
It is usually uncommon for orthodontists to contact their patients’ pediatricians to discuss details of the planned orthodontic treatment. Orthodontists in general rely on parents to disclose their children’s medical history at the time of the initial evaluation. Most of the communication regarding a specific patient is between the orthodontist and the general or pediatric dentist, on issues of a dental nature. If the child presents with a complicated medical history, the orthodontist should contact the pediatrician to discuss the implications of orthodontic treatment on the health of the patient, and vice versa. Every initial evaluation should contain a detailed medical history, including questions about overall and dental health, past diseases, and the patient’s behavior and development. The medical history should be updated every year. When problems of growth and development or diseases (e.g. history of cancer, failure to thrive, cardiac problems, or bleeding disorders) are detected during the medical history, the orthodontist should contact the pediatrician for a discussion of the patient’s needs and a better assessment of the child’s overall health.
The orthodontic treatment plan should take into consideration the risks involved in mechanotherapy in individual patients, in light of their health status, and modify the treatment plan accordingly to achieve optimal results, despite the existence of some health challenges. For example, in patients with bleeding disorders (hemophilia, von Willebrand disease and other bleeding problems) the risk of bleeding must be minimized and thus it is likely that surgery will not be recommended. Extractions should be discussed in detail with all healthcare providers involved, the orthodontist, the pediatrician, the hematologist, and the oral surgeon. If possible, the use of metallic bands should be avoided because of the inevitable soft tissue injuries that occur during band fitting. A lengthy discussion about risks and benefits of treatment should take place with the parents prior to initiating any treatment. When cardiac problems are identified at the time of medical history, it is important to determine if the patient requires antibiotic prophylaxis prior to placement of bands or any procedure that creates a high risk for bleeding. Again, effective communication with the pediatrician is important.
One should not assume that effective communication always occurs naturally. Acquiring effective interpersonal skills requires observational practice and application of interpersonal communication principles (Fallowfield et al., 1998). Even when providers come from the same geographical area, they often have different educational, socioeconomic, and cultural backgrounds. The orthodontist may opt to contact the pediatrician directly by phone to obtain more information and discuss specifics of treatment. Requests for copies of medical records including chart entries and past examinations are helpful for formulating a proper diagnosis and plan of treatment. Written documentation is essential for continuity of care as well as for future reference. If additional healthcare providers are consulted, written letters and referrals should be supplied to the patient, as well as to the pediatrician, with copies kept on the patient’s chart.
The following disorders are easily diagnosed by the pediatrician or parents and represent conditions in which early intervention might be appropriate to prevent possible future orofacial dysfunction: sucking habits and tongue thrusting persisting beyond 3 years of age, speech problems caused by malocclusions, chronic mouth breathing, sleep apnea, significant deviations from tooth eruption norms, early problems with jaw(s) growth and temporomandibular joint disorder (TMD) dysfunction. In general, preventing orofacial dysfunction should be based on promoting normal growth and craniofacial development and the elimination of potential environmental factors that may harm these processes. The following is a discussion of some of these disorders that affect normal growth.
Pervasive Sucking Habits and Tongue Thrusting
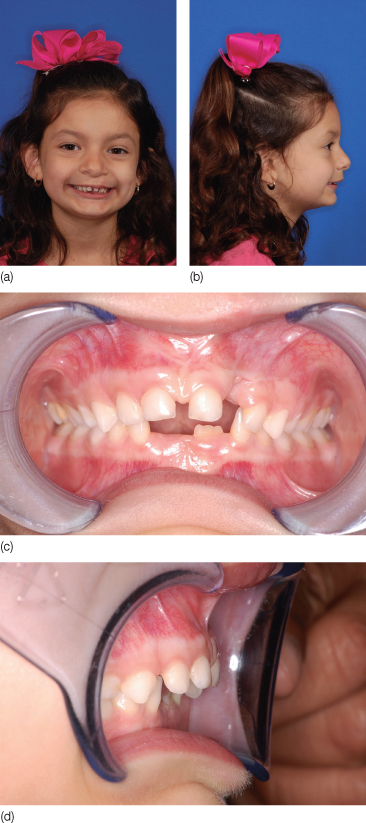
Sucking behaviors are common in infants and young children. Use of pacifiers, blankets, and toys, as well as nutritive sucking, such as bottle feeding and breastfeeding, should be encouraged for normal development. Early premature babies often need to learn how to suck properly prior to being discharged from the hospital, to enable them to receive adequate nutrition at home. However, prolonged sucking habits should be discouraged after the age of 3 years. If there is an existent open bite at this age, it will usually correct spontaneously if the habit is discontinued, and as long as the perioral musculature is intact and with normal tonicity (Figure 6.1). If the sucking habit persists, there may be negative consequences in the developing orofacial structures, with the severity being dependent on the duration, frequency, and intensity of the habit (Ngan and Fields, 1997).
Figure 6.1 Two and a half years old girl with a pacifier habit. (a) A dental anterior open bite localized to the right side, where the pacifier usually rested. (b) The pacifier was removed and the habit stopped. Nine months later the open bite closed spontaneously with help from the perioral musculature.

The literature clearly supports findings of increased severity and frequency of malocclusion, with anterior open bites and posterior crossbites, in children in the late primary dentition period with prolonged sucking habits (Subtelny and Subtelny, 1973; Bishara et al., 2006). It is unlikely that orthodontists will be given an opportunity to evaluate many of these children at this early age. Therefore, it is important to educate pediatricians to recognize these findings for proper referral to a pediatric dentist. Unfortunately, the number of pediatric dentists is inadequate to meet the needs of all children, and many general dentists are not equipped with the skills and training to handle small children. Usually pediatricians see children eight times in the first year of life and 13 times by the age of 3 years and thus have a better chance of recognizing these habits at an earlier age than the dental professionals. Pediatricians can start by discouraging the habit and educating parents on issues such as when to switch from the bottle to the ‘sippy cup’, and removing the pacifier. A pediatric consultation will be useful for older children with thumb and finger sucking habits, and they can suggest a variety of methods to address such habits, including the use of a number of different commercially available products. Regardless of the existence of a habit, a recommendation to see a pediatric dentist should be made by the pediatrician at early stages of dental development for supervision of oral and dental health.
Thumb sucking or finger sucking is perhaps the most common persistent infant habit beyond the age of 3 years. It has been correlated with an increased prevalence and severity of Class II malocclusions and maxillary protrusion, from the deciduous through the mixed dentition periods (Antonini et al., 2005) (Figure 6.2). Moreover, persistent digit-sucking habits create a mechanical obstacle for the eruption of anterior teeth, which in turn can result in an anterior open bite. Cozza et al. (2005) found that the combination of a persistent sucking habit in a child with a vertical growth pattern can increase the chances of developing an anterior open bite. This finding may explain, at least in part, how external factors can influence or exacerbate the already programmed pattern of facial growth.
Figure 6.2 Six-year-old girl with a thumb sucking habit. (a,b) Facial pictures showing protrusion of the upper incisors, and a retrognathic, convex profile. (c,d) Intraoral views showing the dental occlusion with increased overjet and spacing between upper anterior teeth.
Thumb sucking may be an outcome of stress and changes in the child’s emotional status, and treatment should be directed at correcting the underlying problem. Therefore, a consultation with the pediatrician is warranted. A risk of reduced social acceptance among school-age children (7 years old) has been implicated in thumb sucking (Friman et al., 1993). In order to stop the habit, a myriad of treatment methods are available, including behavioral conditioning techniques, positive reinforcement, and oral/dental appliances.
Tongue habits, particularly tongue thrusting, have been implicated in the protrusion of lower incisors, and the creation of an anterior open bite (Subtelny and Subtelny, 1973). It seems evident that problems arise from the postural position of the tongue at rest as opposed to during function (Figures 6.3, 6.4). When planning treatment for correction of malocclusions in these patients, a combined approach with a speech pathologist to help train a new tongue position after treatment is recommended. This training may prevent or minimize future relapse tendencies.
Figure 6.3 Eight-year-old boy with a tongue thrusting habit. (a) Facial picture showing a mild anterior open bite and (b) intraoral view showing the dental occlusion with a mild anterior open bite due to the anterior tongue position, with constricted upper arch and maxilla. (c–e) After expansion treatment, combined with speech therapy to retrain tongue posture, the open bite closed. (f) The patient was followed up for a year, during which no relapse was observed.
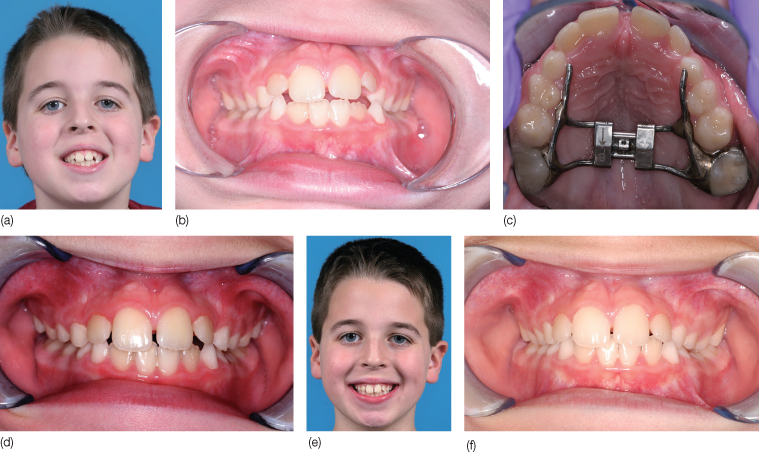
Figure 6.4 Four-year-old girl with enlarged tonsils and adenoids, chronic mouth breathing and lower tongue posture. (a) Facial picture showing an enlarged mandible with a deficient maxilla and (b) intraoral view showing the dental occlusion with an anterior crossbite and increased/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


