20
Paediatric anaesthesia
Anaesthetic management of children
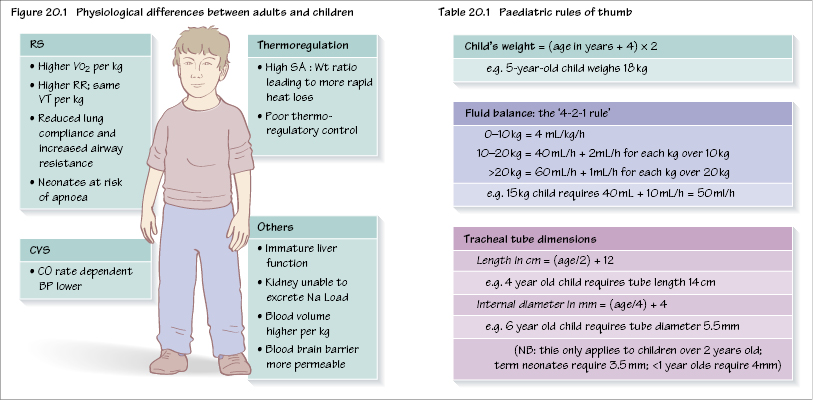
There are a number of differences between adults and children, and in particular neonates (Figure 20.1). Children are not just miniature adults; their body parts have different proportions and their organs are less mature. These differences are most marked in neonates and become less distinct as children get older.
Preoperative assessment
Rapport should be established with the child and his/her parent(s) and a parent should be invited to the anaesthetic room.
Note is made of weight and age, including prematurity. Much of the adult preassessment template may be used, such as previous illnesses, medication and allergies, and teeth. In addition, upper respiratory tract infections (URTIs) are not uncommon in young children and place the child at increased risk of perioperative respiratory problems. Ideally, several weeks should have elapsed following a URTI, although some children have recurrent URTIs and it may not be practical to delay surgery. However, any child with a productive cough, chest signs or a temperature should not be submitted to elective surgery.
Preoperative tests are seldom required, especially for healthy children undergoing minor surgery.
A plan of the anaesthetic should be discussed with the parents and includes the method of induction, postoperative analgesia (including the use of suppositories) and what to expect in terms of i.v. cannulae, infusions, nasogastric tubes, etc.
Fasting for children will be in line with local policy and is typically 2 hours for clear fluids and 6 hours for solids (as in adults). Fasting times for milk is generally taken to be 4 hours, although some advocate only 3 hours for breast milk.
Premedication is usually topical local anaesthetic for venous access. Some centres administer routine preoperative ana/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


