Chapter 20 Medical Evaluation of the Dental Implant Patient
The medical evaluation of patients considering implant therapy is an important aspect to consider for every patient. A retrospective analysis of Veterans’ Administration Registry data found that the medical status of patients (i.e., medical history, American Society of Anesthesiologists [ASA] category, and medication history) correlated with implant failure.1 This chapter is specific for an implant candidate and is developed in three sections. The first section focuses on the importance of the patient interview, with primary emphasis on the medical history questionnaire and the physical examination. The medical history includes those medical conditions most likely to influence implant treatment decisions. The physical examination consists of a hands-on evaluation and recording of the patient’s vital signs. The second section (Laboratory Evaluation) reviews those laboratory tests of interest to implant dentistry. The evaluation includes a complete blood cell count (CBC), basic metabolic panel (BMP), comprehensive metabolic panel (CMP), or bleeding disorder tests. The third section relates the medical and dental implications of the most common systemic diseases found in implant patients.
MEDICAL EVALUATION
The medical evaluation remains of paramount importance in implant dentistry, perhaps more so than in other disciplines of dentistry.2 Implant treatment is primarily a surgical, prosthetic, and maintenance discipline for an older segment of the population. The need for implant-related treatment increases with the age of the patient; as a result, the implant dentist treats more elderly patients than do other specialists in dentistry.3,4
An estimated 12% of the U.S. population is 65 years of age or older; this number is expected to reach 21% (64.6 million) in the year 2030.5 A 65-year-old person has a life expectancy of another 16.7 years, and an 80-year-old person can expect to live an additional 8 years.6 These patients often request implant support for their failing fixed restorations or to improve the conditions of their removable prostheses. An increased life span means the number of elderly patients in the dental practice is likely to increase. Therefore it is important to design the medical and physical evaluations to accommodate the special conditions of these patients.
Physiologic Changes in the Elderly
In general, a healthy older person demonstrates only half the lung function of a healthy young adult. The blood flow of an older patient is 80% that of the healthy 30 year old, the cardiac output is only 70%, the renal plasma flow is only 50%, and the glomerular filtration is only 60%. A decrease in the elasticity of the arterial system is illustrated by an increase in systolic blood pressure. The vital capacity is reduced to 70% of a 17-year-old patient and corresponds to a decrease in the arterial partial pressure of oxygen.7 Gastric motility and intestinal absorption are also decreased.
The total body weight of the patient is often reduced, especially if masticatory deficiency from lack of teeth and bone is present; however, there is an increase in body fat. Consequently, any medications administered will follow modified pharmacokinetics and dynamics. Drug kinetics are modified, especially in the distribution phase, as a result of the increased water weight, decreased plasma albumin, and decreased cardiac output. The decreased plasma albumin concentration causes a greater percentage of the drug to remain free and active. The decreased ability to metabolize drugs, related to the decreased renal function, is responsible for the decreased excretion of the drugs. Therefore the intervals between drug administration should be longer and dosages should be decreased, except for liposoluble drugs and antibiotics, to compensate for the increase in body fat and the reduced immune response.
Chronic illness and multiple disease states are characteristics of aging. Patient surveys indicate that 80% of the elderly have at least one chronic disease. Half of the people older than 65 years have arthritis, 42% have hypertension, 34% have other cardiovascular problems, and more than 40% have hearing impairments. Other conditions associated with aging are the increased frequency of diabetes (8.5%), immune response problems, orthopedic (osteoporosis) problems (17%), and sensory deficiencies as well as degenerative diseases.8,9 The influence of chronic disease states doubles for people older than 65 years of age and affects pathologic processes; surgery may increase individuals’ surgical risks and affect prognoses.
Medications and the number of drugs usually increase with age; women usually take more medications than men. At least 75% of patients 65 and older take medications.10–12 Elderly patients receive 25% of all prescription drugs, although they represent only 12% of the total population. They receive an average of 13 prescriptions a year, in addition to numerous over-the-counter drugs, mainly analgesics. The drug categories most often prescribed among the top 50 drugs prescribed in 2004 include: (1) cardiovascular drugs (13 of the top 50), (2) central nervous system agents (10 of the top 50), (3) gastrointestinal and respiratory agents (7 of the top 50), and (4) endocrine agents (6 of the top 50).13
Side effects of cardiovascular drugs depend on the drug category. Digitalis can cause nausea, anorexia, chromatopsia, and arrhythmias. Diuretics cause dehydration, xerostomia, electrolyte imbalance (potassium depletion), and hyperglycemia and predispose to sialoadenitis. Calcium channel blockers may be responsible for edema, constipation, and gingival hyperplasia. Nifedipine, a calcium channel blocker, is known to exacerbate gingival enlargement around both natural teeth and dental implants. To date, the best management is still frequent professional cleanings combined, if necessary, with surgical removal of the hyperplastic tissue to ease daily care and improve esthetics. Angiotensin-converting enzyme inhibitors may produce cough, angioedema, and taste alteration. Anticoagulants and potential risk of hemorrhage are well documented. Care should be taken not to administer erythromycin with terfenadine (Seldane) because of potential cardiotoxic drug interaction. The most common risk of patients on insulin is hypoglycemia.14–17 Therefore dental practitioners may have to address a variety of drug-related adverse effects, the most common being:
In older patients, 30% of drug-induced illnesses are due to interactions between medications. Antimicrobials and analgesics accounted for 40% of these.17 These interactions account for 20% of hospital admissions of senior citizens. Notably, asthmatic patients taking NSAIDs may experience acute bronchospasm. Terfenadine (Seldane) may cause life-threatening ventricular arrhythmias in patients taking ketoconazole or erythromycin.18 Erythromycin can cause nausea, vomiting, and cardiac dysrhythmias in patients on carbamazepine treatment. Patients receiving antiparkinsonian treatment with selegiline (Eldepryl)18–20 may suffer fatal interaction if used with opioids (especially meperidine).18–20 Patients following antihypertensive therapy should not receive long-term NSAIDs therapy because the latter may significantly lower the efficacy of the antihypertensive agents.
Management of Elderly Implant Patients
Even healthy older implant candidates (older than 60 years) should be considered as patients with mild systemic disease, just because of their age.21 As a result of a decrease in physiologic adaptability, the aged patient has less reserve to react to stress. If the limits of homeostatic reserve are reached, the patient can reach a critical condition.22 The elderly patient can follow regular implant therapy provided a typical stress reduction protocol is implemented. Monitoring of vital signs, modified dosage of medications, and special care during sedation because of an increased sensitivity to CNS depressants are indicated. An increased dosage of antibiotics compensates for the less competent immune system and the increased susceptibility to viral and bacterial diseases. An increased dosage of liposoluble drugs is also suggested. Elderly patients are reportedly less sensitive to pain, so a reduced dosage of narcotic analgesics is recommended, especially because gastric motility is reduced in these patients. The doctor should be aware of the eventual adverse drug reactions to the medications already taken by these patients when combined with those later prescribed for implant surgical procedures.
MEDICAL HISTORY
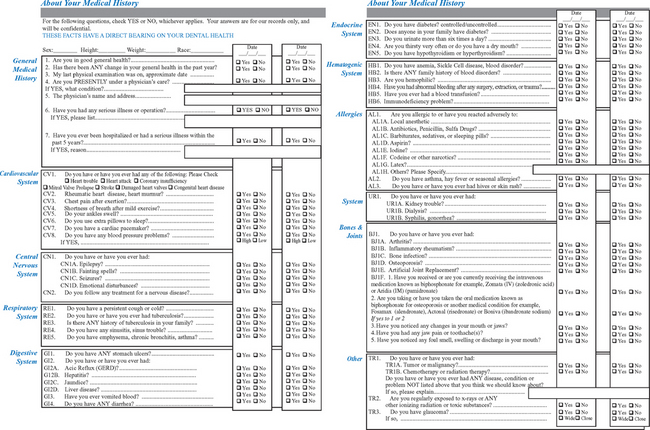
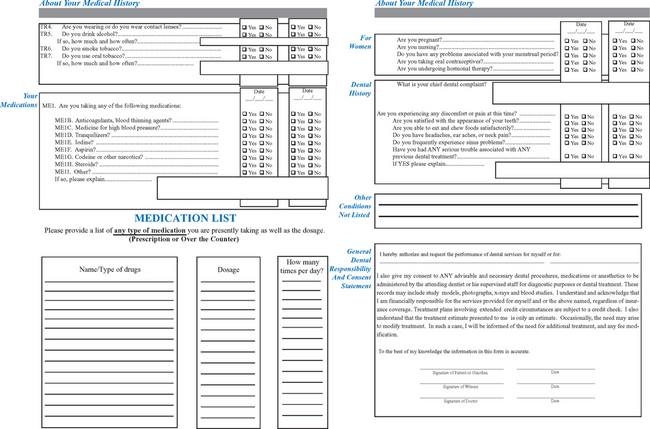
The two basic categories of information addressed during the review of the medical history include the medical history and a review of the patient’s systemic health. The dental office uses a medical evaluation form to obtain most of this information (Figure 20-1).23 Of particular note is medication usage within the preceding 6 months, allergies, and a review of the systems of the body. The pathophysiology of the systems, the degree of involvement, and the medications being used to treat the conditions are evaluated. It is important to review this form with the patient to ensure that comprehension is adequate to answer all questions. The form should include all medical areas of interest to the implant dentist.
Vital Signs
Blood Pressure
Approximately 10% of dental offices record the patient’s blood pressure.24 This proves worthwhile for the implant dentist because surgery and long prosthodontic procedures are frequently required. The importance of obtaining and recording the blood pressure in every implant patient is twofold. First, the initial recording may serve as a baseline measurement, which if too high may contraindicate a surgical procedure. Second, when in an acceptable range, the initial blood pressure acts as a baseline measurement specific for that patient. If the patient has a future problem during treatment, the blood pressure difference between baseline and the current situation may alter the medical risk of the patient.
The blood pressure is measured within the arterial system. The maximum pressure is the systolic, and the minimum pressure is the diastolic. Blood pressure is influenced by the cardiac output, blood volume, viscosity of the blood, condition of blood vessels (especially the arterioles), and heart rate. There is a direct and an indirect determination of blood pressure. The dentist will use only the indirect method. This technique was first developed by the Italian physician Riva-Rocca in the nineteenth century.25 The sphygmomanometer consists of an inflatable bag covered by a cuff and a manometer to register the force and rate of air within the bag. The two most common manometer systems use mercury gravity or aneroid gauges. The mercury system is more accurate in changing climates; after it is calibrated, it is consistent for many years. The aneroid manometer is as accurate as the gravity type, but requires regular calibration.
Blood pressure monitoring should only be completed by trained medical personnel. The operator should be trained and retrained on a regular basis in the standardized technique. Patients should ideally be seated for 5 minutes, with their feet on the floor and arm supported at the level of the heart. Caffeine intake, smoking, and strenuous exercise should be avoided for at least 30 minutes before measurement. At least two measurements should be taken, with the average recorded. An appropriately sized cuff (cuff bladder encircling 80% of the arm) should be used for accuracy.26 The inflatable cuff is positioned over the bare upper arm at the level of the patient’s heart, with the patient’s palm supine. The brachial or radial artery is palpated and the bag is inflated to obliterate the vessel, about 30 mm Hg above the estimated systolic pressure. The cuff is deflated 2 to 4 mm Hg at every heartbeat. Using a stethoscope over the brachial artery, the systolic pressure is recorded at the first tapping sound heard. When the sounds become muffled or inaudible the diastolic pressure is noted.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses