Autoimmune Disorders
➧. Concepts of Immunity and Autoimmunity
Mikulicz’s Disease (Benign Lymphoepithelial Lesion)
Aphthous Stomatitis (Aphthous Ulcers, Canker Sores, Recurrent Aphthous Stomatitis)
Systemic Autoimmune Diseases with Orofacial Manifestations
➧. Epidermolysis Bullosa Acquisita
➧. Systemic Lupus Erythematosus
➧. Autoimmune Polyendocrinopathy–Candidiasis-Ectodermal Dystrophy
Concepts of Immunity and Autoimmunity
Autoimmunity
When the concept of autoimmunity came to be accepted as a pathogenic mechanism, a large number of diseases were suggested to have an autoimmune etiology, based on the finding of autoantibodies in the patients. However, autoantibodies have also been found in the serum or tissues of otherwise normal and healthy elderly individuals. Autoantibodies are also formed following tissue injury and may serve a role in the removal of the products of tissue breakdown. This lead to the need to formulate criteria for diagnosing autoimmune diseases.
Diagnostic criteria for autoimmune disorders
a. Circulating or localized populations of cells sensitized to antigen, or products of immunologically activated cells, active under physiologically conditions should be demonstrated, or
b. Circulating or localized populations of cells sensitized to antigen, or products of immunologically activated cells, active under physiological conditions, should be present
2. Sensitizing antigen should be identified and characterized
3. Antibodies or sensitized lymphocytes should be produced in vitro or in animals against the same antigen
4. Pathological events in vitro or in the experimental animal should correspond to those in human disease
5. Transfer of disease from immunized to normal animal by cells or serum.
Classification of autoimmune diseases
Fergusson (1995) categorized autoimmune diseases as organ specific and non-organ specific.
Sjögren’s Syndrome (Gougerot–Sjögren Syndrome)
Described in Chapter 11 (Diseases of Salivary Glands) on page 265.
Mikulicz’s Disease (Benign Lymphoepithelial Lesion)
Described in Chapter 11 (Diseases of Salivary Glands) on page 265.
Aphthous Stomatitis (Aphthous Ulcers, Canker Sores, Recurrent Aphthous Stomatitis)
Described in Chapter 7 (Vesiculobullous Disorders) on page 174.
Giant Cell Arteritis
Giant cell arteritis is a relatively common form of large vessel vasculitis occurring predominantly in elderly individuals. The mean age of onset is 70 years with a 2:1 female-to-male ratio. Temporal artery is the common artery that is involved in cranial arteritis (Figure 1).

Figure 1 The prominent temporal artery in a patient suffering from temporal arteritis. Courtesy: Dr C Stephen Foster, The Ocular Immunology and Uveitis Foundation, Cambridge, Massachusetts, USA
Muki proposed an autoimmune basis for giant cell arteritis because it occurred more frequently in patients with other autoimmune disorders such as thyroid disease or rheumatoid arthritis.
Periodontal Disease
1. Enhanced presentation of self-antigens through increased expression of the molecule associated with antigen presentation, namely, Ia antigen.
2. Altered T helper or T suppressor cell function.
3. Polyclonal activation of cells which have the ability, for reasons which may not be clear, to produce autoantibodies.
4. Idiosyncrasies of the antigen-idiotype network.
5. Bacterial or viral cross-reactivity with self-antigen leading to the production of cross-reactive antibodies
Rheumatoid Arthritis
Pathogenesis
The involved mechanisms in the causation could be:
1. Genetic susceptibility: Rosenberg and Nuki have shown that 65–80% of the individuals suffering from RA have human leukocyte antigen (HLA)-DR4 and HLA-DR1 or both. Other haplotypes like DW4, DW10, DW13, DW14 and DW15 have also been implicated.
2. Primary exogenous arthritogen: Roudier et al proposed Epstein–Barr virus as the primary microbial agent for the causation of RA. Other microbial agents like retroviruses, parvoviruses, mycobacteria, borrelia and mycoplasma could also initiate the disease.
3. Autoimmune reaction: Warder in 1940 proposed the presence of rheumatoid factor, which was the first human autoantibody described in association with RA.
4. Mediators of tissue damage: Panaji in 1993 reported that the rheumatoid synovium was heavily infiltrated with lymphocytes, most of which were CD4+ helper T cells. They generate cytokines, which in turn could activate other immune cells and macrophages.
Clinical features
 It can occur at any age, but bimodal peaks are seen at 40 and 60 years of age.
It can occur at any age, but bimodal peaks are seen at 40 and 60 years of age.
 Women are two-and-half times more likely than men to develop disease.
Women are two-and-half times more likely than men to develop disease.
 Patients complain of polyarthralgias, fatigue and muscle aches.
Patients complain of polyarthralgias, fatigue and muscle aches.
 Prolonged morning stiffness of joints.
Prolonged morning stiffness of joints.
 Joints of the hands, feet, elbows, shoulders, knees and TMJ are affected.
Joints of the hands, feet, elbows, shoulders, knees and TMJ are affected.
 Within weeks of affliction, the involved joints become tender and marked swelling is seen.
Within weeks of affliction, the involved joints become tender and marked swelling is seen.
Joint manifestations
Katz classified the joint manifestations as:
1. Joints that are usually affected—ankles, cervical spine, elbows, hips, knees, metacarpophalangeal joints, metatarsophalangeal joints, proximal interphalangeal joints, shoulders, tarsal joints, temporomandibular joints and wrists.
2. Unusually affected joints—carpometacarpal joints, cricoarytenoid joint, sacroiliac joints and sternoclavicular joint.
3. Rarely affected joints—distal interphalangeal joints, lumbar spine.
Temporomandibular joint manifestations
Almost 60% of the individuals present with bilateral involvement of joints.
1. Active phase (acute symptoms, synovial effusion, destruction of fibrocartilage and erosion of underlying bone)
2. Healing phase (remodeled and flattened articular surface)
3. Secondary osteoarthrotic phase (marginal proliferations and further destruction of the condyle, predominant clinical finding of crepitus).
Radiographic features of rheumatoid arthritis affecting the TMJ
1. Formation of new bone (marginal proliferation) was described in 1975 by Hugh Ogus. It is reported that the erosions of the articular surface were the most important diagnostic finding of RA in other joints and not the TMJ.
2. Subcondylar cystic destruction and severe destruction of bone eventually lead to complete loss of condyle. Such destruction will give the remaining condylar bone the shape of the mouth piece of a flute.
3. Anterior open bite and reduced joint space (due to destruction of articular cartilage).
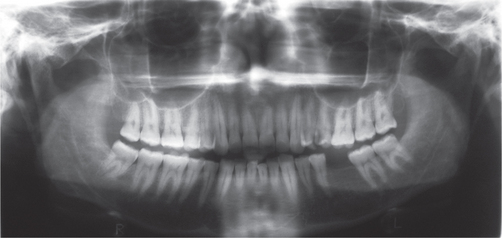
4. The most characteristic radiographic signs of RA in the TMJ are erosions of cortical outline and reduced joint space (Figure 2) as proposed by Akerman et al in 1988.
Kopps in 1995 stated that the radiographic diagnosis of RA in TMJ was difficult. However, absence of radiographic changes in the TMJ will not exclude the possibility of early RA in TMJ.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses