2
Upper Removable Appliances: Indications and Principles of Design
Upper removable appliances (URAs) are ‘removable braces’ that fit on the upper arch only. In the past, URAs were used for many malocclusions, including severe Class II division 1 cases. However, this is no longer seen as appropriate because removable appliances can only achieve very simple movements, i.e. simple tipping of teeth, and the vast majority of malocclusions that warrant treatment require far more complex movements (using fixed appliances) to achieve an adequate outcome. Fixed appliances can also tip teeth, but in complete contrast to removable appliances, they can also achieve bodily movement (including rotations, intrusion and extrusion) as well as torque. Therefore, regarding active treatment, this book will mostly confine itself to interceptive treatment where the types of malocclusion to be intercepted are very limited; if tooth movement is required, it is confined to tipping movements. The exceptions are covered in Chapters 10 and 11.
- The indications for the use of URAs
- The importance of anchorage
- The advantages and disadvantages of removable appliances
- What the components of URAs are
- What the components of URAs look like
- The design principles and steps to consider when designing URAs
- The importance of the timing of appointments
Prerequisites for Orthodontic Treatment
It must be understood that for any patient seeking any form of orthodontic treatment, dental health (including dietary control) and oral hygiene must be excellent prior to treatment. Therefore, before any referral is made, the referring dentist must ensure that their patient is dentally fit, i.e. no active caries, gingivitis or periodontal disease, and that they have a standard of oral hygiene that is excellent – this is the level required to support appliance therapy. A number of recent audits in the UK have indicated that 30% of patients have undiagnosed/untreated caries on referral to an orthodontist. This wastes a great deal of everyone’s time as, obviously, the orthodontist cannot accept a patient for treatment if the patient is not dentally fit and/or has poor oral hygiene/diet control. This is because significant damage, e.g. caries, will be caused to the teeth and supporting structures by any appliance used under the wrong conditions. Damage will also occur far more quickly and severely than under normal conditons. Furthermore, restoration of teeth is more difficult once appliances are in place.
If, as the referring clinician, your patient cannot meet these conditions, but wants orthodontic treatment, you will need to explain to the patient/carers why referral is inappropriate and what the consequences of poor dental health are for their orthodontic treatment prospects. Treatment may be harder or more complicated if treatment has to be delayed until growth is (nearly) completed. Indeed, treatment may not be feasible unless dental health improves.
Oral hygiene that is less than optimal may lead to demineralisation of the enamel surface around or under any appliance, including the attachments of a fixed appliance. Such demineralisation can actually occur within a few weeks of an appliance being placed and, if severe, can lead to cavitation. The benefit of orthodontic treatment in providing a good occlusion and smile aesthetics is thus undone by the marking on the labial surfaces of the teeth in the case of fixed appliances (see Figure 5.20). However, around URAs damage may be hidden palatally from the patient and unwary clinician.
Moving teeth through bone in the presence of gingival inflammation and/or active periodontal disease will lead to very rapid destruction of the alveolar bone. Therefore, tooth movement should never be undertaken until the disease has been successfully treated; there is no bleeding from the gingival margins or the base of the periodontal pockets, and the patient has demonstrated that they are able to maintain the necessary level of oral hygiene.
It should be emphasised that before any appliance is fitted, a full orthodontic assessment (including appropriate radiographs) and diagnosis must have been performed. A problem list derived from the case assessment will then form the basis of a proper treatment plan. It is assumed that readers are able to undertake these tasks appropriately and the details of these steps are not covered here. To refresh your memory on any aspects of assessment, diagnosis or treatment planning, readers are referred to other textbooks.
Anchorage
Before discussing how to design URAs, we need to briefly remind ourselves about one very important aspect of orthodontic treatment – anchorage. Unless anchorage is given appropriate consideration, orthodontic treatment cannot only easily fail, but the original malocclusion can be made much worse.
What Is Anchorage?
Anchorage is most easily defined as the resistance to unwanted tooth movement. In other words, it is what stops the wrong teeth from moving. Newton’s Third Law of Motion states that: ‘To every action there is an equal and opposite reaction’.
In orthodontics, because of Newton’s Third Law, we can all too easily find that unwanted tooth movement takes place. In order to minimise such movement, it is generally accepted that during URA treatment, only one or two teeth should be moved at a time. This means that the movement of a few teeth (or a tooth) is being pitted against the movement of many or the majority of teeth. This works because generally, the larger number of ‘anchoring’ teeth will have a larger root surface area than the smaller number of teeth to be moved (see Figure 2.1 for examples). Whilst the equal and opposite reaction will be ‘experienced’ by all the teeth in contact with the appliance, this force will be distributed according to root surface area. Thus, large rooted teeth will ‘experience’ a larger force than small rooted teeth, but if there are many teeth in contact, then each tooth will ‘experience’ relatively low force levels – levels that will not lead to significant tooth movement. Pitting a larger number of teeth against a smaller number of teeth actually being moved, thus provides increased anchorage. However, where for example a crossbite is to be corrected, it may be appropriate to pit one upper quadrant (e.g. URCDE6) against the opposite buccal quadrant using a screw as the active component. Turning the screw results in equal buccal movement of both sets of upper buccal teeth in a reciprocal movement since the root surface areas of both sets of teeth are roughly equivalent.
Figure 2.1 Anchorage. Larger teeth have larger root surface areas than smaller teeth. The groups of teeth that are pitted against each other will determine the anchorage balance.
(Reproduced from Nelson-Moon ZL (2007) Craniofacial growth, cellular basis of tooth movement and anchorage. In: L Mitchell (ed) An Introduction to Orthodontics, p. 46, Figure 4.20, by permission of Oxford University Press.)
Image not available in this digital edition
Causes of Anchorage Loss
In circumstances where anchorage is not controlled, it can be lost very easily.
Operator Factors
- Incorrect diagnosis/treatment plan
- Over activation of springs
- Incorrect URA prescription, e.g. if wire dimensions are too thick, these apply too much force when activated
- Inappropriate spring design or inadequate/ambiguous spring prescription on the laboratory card
Patient Factors
- Failure to wear appliance as instructed
- Distortion of spring(s) causing excessive force to be applied
- Appliance breakages, allowing uncontrolled tooth movement
- Failure to return for appliance checks, allowing uncontrolled tooth movement
Laboratory Factors
- Failure to follow prescription
- Prescription unclear, leading to errors in manufacture
Results of Anchorage Loss
In the worst case scenario, treatment can make the original malocclusion far worse. For example, if one or more teeth is/are retracted distally along the arch using excessive forces, the other teeth, via the equal and opposite reaction, will move mesially. Especially if the force levels are sufficient to reach optimum levels (25–50 g), the ‘anchorage’ teeth will ‘experience’ forces leading to forward movement of all the anchorage teeth. This will appear as a visible and measurable increase in overjet. This increase in overjet will continue for as long as the excessive force is applied. In other words, it is possible for a patient who has a normal overjet to end up with an increased overjet as a result of poor management or incompetence by the dentist. To put it bluntly, they could end up complaining of ‘goofy teeth’ – a problem caused by orthodontic treatment. Such problems can be very hard to correct. As can be seen from the lists above, operator causes of anchorage loss outnumber those caused by patients.
Sources of Anchorage
Anchorage is gained from all teeth in contact with the URA and from contact with the palate. Well-fitting appliances are thus crucial. Rarely, anchorage can be re-inforced using extra-oral sources, i.e. headgear. In addition, in a relatively new development that is beyond the remit of this book, anchorage may be gained in some circumstances using temporary anchorage devices (TADs; also known as mini-screws). These are now being used in conjunction with fixed appliances.
The remit of this book is limited. Therefore, readers are strongly advised to consult other textbooks for more detailed discussions of how anchorage can be gained and its management. However, anchorage will be discussed briefly in connection with the examples of appliance design given in Chapter 3.
Components of URAs
URAs always comprise an acrylic baseplate with various stainless-steel (ss) wire components. These wire components may have the following functions:
- To retain (or ‘clip’) the appliance to the upper teeth. All URAs will have these.
- To move the teeth. These active components are springs. Only active appliances will have these.
- To prevent movement of some teeth. These passive components simply hold the teeth still. These may be made of wire or acrylic and, whilst they will always be present on passive appliances, they may also be present on active appliances.
For some URAs, active components may use a screw rather than a spring to move teeth.
An example of a URA is shown in Figure 2.2. URAs are orthodontic appliances which, if active, only tip teeth or, if passive, maintain tooth position. That is all they do. This is in contrast to fixed appliances which, as we have already said, can perform all tooth movements (including tipping of teeth).
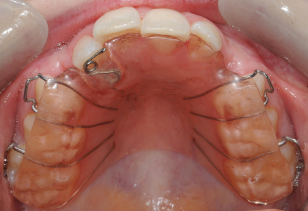
Figure 2.2 Example of an upper removable appliance (URA). This shows a Z-spring used for correcting incisor crossbites.
Passive URAs are of two types:
- Space maintainers: these aim to prevent the movement of teeth into a space where another tooth is to erupt.
- Retainers: these aim to maintain teeth in their new positions following active tooth movement. They may also be used to hold open spaces that have been created during active treatment for restorative purposes, e.g. in patients with hypodontia. Retainers will be discussed separately in Chapters 7–9.
With the exception of some retainers (e.g. vacuum-formed retainers; see Chapters 7 and 8) and space-maintaining appliances, the components of all other URAs are:
- Retentive components: These are usually wire clasps, most commonly either Adams’ clasps (for posterior or anterior teeth, hence their other name of ‘universal’ clasps) or Southend clasps (for one or two adjacent anterior teeth). Occasionally ‘C’-clasps or some types of labial bow may be useful, but labial bows are mostly used in retaining appliances (retainers). Other types of retentive components also exist but are generally infrequently used. For instance, ball clasps can be used but generally only in quite specialist situations such as in the Twin Block functional appliance around the lower incisors (see Figure 10.3 and 10.4).
- Acrylic baseplate: This will be unmodified if the appliance is passive, but in active appliances may sometimes usefully include posterior capping or a biteplane.
- Active components: These are most frequently wire springs or occasionally screws; rarely a labial bow is used, but the indications (see Chapter 3) are very limited so it is better to dismiss bows for active tooth movement in most cases.
When tipping teeth with a URA, only light forces (25–50 g; 50 g maximum) per spring must be applied. The force applied by an activated spring can be measured with spring gauges as shown in Figure 2.3. URAs that incorporate springs as the active component rely on being activated by the clinician; this contrasts with screw appliances which have to be activated by the patient. The latter are therefore only used where a spring cannot/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


