10
Removable Appliances for the Postgraduate in Specialist Orthodontic Training
This chapter will give an overview of the types of removable appliances that may be used as part of the definitive treatment for some of the more severe malocclusions. The treatment of these malocclusions and the use of the appliances discussed should not be undertaken without the appropriate theoretical knowledge and practical experience. Therefore, this treatment is really the preserve of the specialist orthodontist or those treating patients under the close supervision of a specialist orthodontist.
However, it is hoped that this chapter will serve as a useful source of basic information for those just starting on their postgraduate training, and also provide some direction for further reading and learning for those who are less experienced, but wish to develop their knowledge further.
The chapter will be divided into three sections covering:
- Removable appliances for correcting excessive positive overjets
- Removable appliances and their role in correcting Class II molar relationships
- Removable appliances for correcting reverse overjets.
- List several appliances that may be used for the correction of excessive positive and negative overjets and molar relationships
- Describe the effects that the appliances may have on the dentition and facial skeleton, including the potential hazards of headgear wear
- Realise the necessity for significant theoretical knowledge and supervised practical experience before using these appliances without direct supervision by an appropriately trained person
Removable Appliances for Correcting Excessive Positive Overjet
Removable appliances for the correction of excessive positive overjet are commonly referred to as functional appliances in the UK. However, they are also known as orthopaedic or growth modification devices because of their perceived effect on maxillary and mandibular growth.
The term ‘functional’ appliance derives from the initial use of these appliances, which aimed to alter the function of the mandible and its musculature by forcing the patient to posture the mandible forward, so reducing the overjet. The stretching of the muscles caused by this was thought to encourage growth of the mandible.
Certainly, growth of the mandible does occur at the condyles with some remodelling of the glenoid fossa. It is possible to see a change in shape and length of the condyles between pre-treatment and post-functional lateral skull radiographs. Growth of the condyles is required to maintain the mandible in the ‘postured’ position as, once the functional appliance is withdrawn, any change in position of the mandible that was due to ‘training’ of the masticatory muscles will become apparent very quickly as the muscles ‘de-train’ and the mandible returns to its original position. However, it is now thought that functional appliances accelerate and redirect the growth of the mandible, rather than increase its growth beyond what has been genetically predetermined.
Historically, functional appliances were used in the treatment of Class II division 1 malocclusions where the upper and lower arches were well aligned, the upper incisors were proclined and there was a Class II skeletal pattern. However, this was in the days when functional appliances were used in isolation to treat Class II division 1 malocclusions and their use was not followed by a course of fixed appliance treatment. These days, the majority of patients have fixed appliance treatment following an initial phase with a functional appliance to correct the overjet and molar relationship. Crowding and alignment of the teeth can then be corrected during the phase of fixed appliance treatment, with or without extractions of permanent teeth. Furthermore, the residual lateral open bites can be closed. Occasionally, these do not close spontaneously.
A wealth of literature, both in textbooks and journal articles, has been published on the use of and theory behind functional appliances. Unfortunately, it is not possible to draw firm conclusions from many of the older research papers as the methods and statistical analyses are flawed. However, it is imperative that the clinician has a good background knowledge of functional appliances before embarking on any such treatments, as inappropriate/inaccurate provision, design and instructions on wear can have a very deleterious effect on the patient’s malocclusion, facial appearance, treatment time, expectations and co-operation.
Effects of Functional Appliances
A well-worn functional appliance will, relatively rapidly in a growing individual, change the molar relationship and reduce the overjet and overbite. All of these changes are usually desired, but functional appliances also produce some changes that are not always advantageous, e.g. increase in the lower anterior face height and proclination of the lower incisors.
The effects of the use of functional appliances on the correction of a Class II division 1 malocclusion are both dental (70%) and, generally to a far lesser extent, skeletal (30%). A more recent multicentre randomized controlled trial has indicated that these figures vary with the parameter being measured (O’Brien et al., 2003). In this study, 73% of overjet reduction and 59% of molar correction was dental. However, the authors reported significant individual variation in the response to functional appliance therapy and, clinically, variation in response is what is typically seen.
Dental Effects
- Retroclination of the upper labial segment (ULS)
- Proclination of the lower labial segment (LLS)
Leading to:
- Reduction in overjet
- Reduction in overbite
- Mesial movement of lower molars
- Distal tipping of upper molars.
Skeletal Effects
These are generally far less predictable than the dental effects, but include:
- Acceleration of mandibular growth
- Retardation of maxillary growth
- Remodelling of the condyle
- Remodelling of the glenoid fossa
- Increase in lower anterior face height.
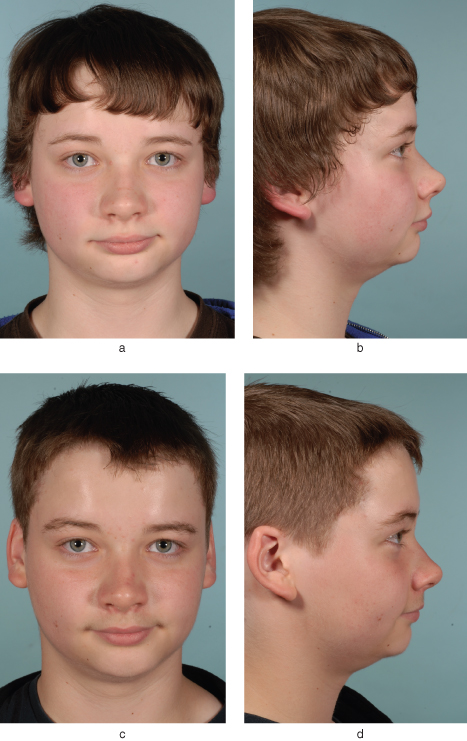
Figures 10.1 and 10.2 show the pre- and post-treatment intra- and extra-oral clinical photographs, respectively, of a patient who underwent 6 months of treatment with a functional appliance (Twin Block). It is apparent that the appliance has corrected the overjet and molar relationship, but has had a lesser effect on the skeletal pattern, although there has been a beneficial increase in lower anterior face height.
Figure 10.1 Pre-treatment (a–e) and post-treatment (f–j) intra-oral views of a patient who underwent 6 months of functional appliance (Twin Block) treatment. Note the correction of the incisor and molar relationship to Class I. Also note the lateral open bites in the post-treatment photographs caused by the posterior biteblocks on the Twin Block appliance. Fixed appliances will now be needed to complete treatment.

Figure 10.2 Pre-treatment (a and b) and post-treatment (c and d) extra-oral views of the same patient as in Figure 10.1, treated for 6 months with a functional appliance. Note that there has been less correction of the Class II skeletal discrepancy than there has of the Class II malocclusion (Figure 10.1). There has been a beneficial post-treatment increase in lower anterior face height and a reduction in depth of the labio-mental fold.
Clark Twin Block
This appliance was introduced by William J. Clark, a specialist orthodontic practitioner working in Scotland, in the 1980s (Clark, 1982). In the last 30 years it has become the most popular functional appliance to be used by orthodontists in the world. Its popularity has arisen due to the perceived ease of wear of this appliance, which comes as separate upper and lower blocks worn as a pair (twin blocks), compared to the more traditional functional appliances, which are fabricated as a single appliance (monobloc).
Indications
- Class II malocclusion with mild/moderate Class II skeletal pattern
- Class II molar relationship
- Increased overjet
- Proclined upper incisors
- Lower incisors that are not already excessively proclined
- Reduced or average vertical proportions
Contra-Indications
- Significant anterior open bite
- Significantly increased vertical proportions
- Excessively proclined lower incisors
Design Features (Figures 10.3 and 10.4)
Since its introduction, there have been a number of designs and modifications of the Twin Block, but one of the most frequently used designs is described below.
Figure 10.3 Laboratory prescription for a Twin Block appliance to reduce the overjet and correct the Class II molar relationship.
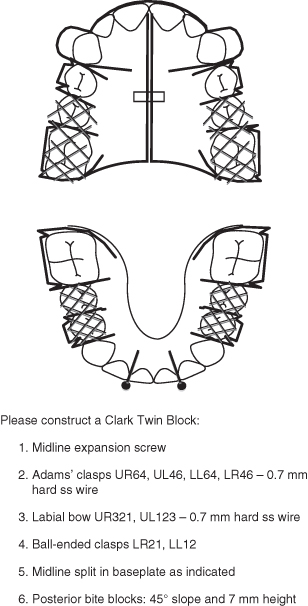
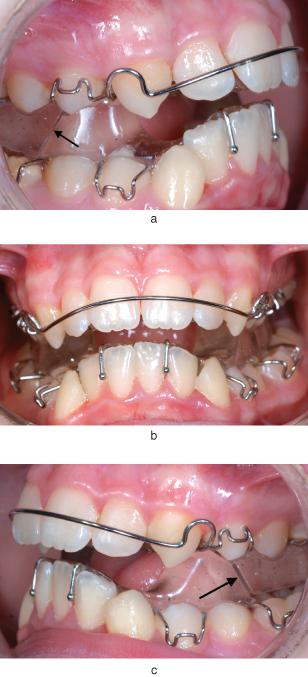
Figure 10.4 Intra-oral views (a–c) of a Twin Block in situ; prescription as indicated in Figure 10.3. Note the 45° slope of the upper and lower posterior biteblocks (arrowed in a and c) as they interlock to keep the mandible in a postured position.
Active:
Midline expansion screw.
Posterior acrylic blocks.
±Labial bow on ULS.
Retention:
Adams’ clasps on all four first permanent molars and all four first premolar teeth.
Ball-ended clasps on lower incisor teeth.
Labial bow on ULS.
Anchorage:
Reciprocal anchorage using posterior acrylic blocks and the mesialising effect on the lower arch and the distalising effect on the upper arch.
Baseplate:
Midline split in upper appliance to allow expansion.
Posterior acrylic blocks with mesial aspect of upper block and distal aspect of lower block angulated at 45°.
Retention is provided by the Adams’ clasps, ball-ended clasps and labial bow. However, if the upper incisors are excessively proclined and spaced, the labial bow can be converted into an active component (see Chapter 4). The midline expansion screw is included as posterior crossbites are often induced as the mandible is positioned more anteriorly and the wider posterior part of the lower arch comes to occlude with the narrower anterior part of the upper arch.
The ‘active’ part of the Twin Block appliance is the acrylic blocks. These were originally designed with a 45° slope on the anterior of the upper block and the posterior of the lower block. As the patient postures forward, the slope on the blocks causes them to interlock, keeping the mandible in the postured position.
If the second permanent molars are erupted, then it is essential to place occlusal stops over these teeth to prevent them from over-erupting. If unerupted, they should be incorporated as soon as they erupt.
Construction
Assuming high-quality impressions, the most important record to collect in order to construct a Twin Block, or any other functional appliance, is the postured bite registration. Although there are a number of different ways of doing this, the principles remain the same:
- The patient should be asked to posture the mandible as far forward as they can achieve comfortably, ideally in an edge-to-edge incisor relationship.
- Assuming that there is no mandibular displacement from the retruded contact position (RCP) into the inter-cuspal position (ICP), care must be taken to ensure that the upper and lower dental centre-line relationship is not altered as the mandible is postured, as a mandibular asymmetry can be induced if the mandible is postured more on one side than the other.
The postured bite may be recorded with either a softened horse-shoe of bite-registration wax at the required thickness or a ProJet® bite-fork, following the manufacturer’s instructions.
Fitting the Appliance
All the principles discussed in Chapter 4 are pertinent to the fitting of functional appliances: checking the appliance before fitting; the advice that should be given to the patient prior to fitting; the way in which the fit of the appliance is checked by the operator, and the adjustments required to increase the retention of the appliance. It is assumed that the reader is already familiar with the content of Chapter 4.
The upper part of the Twin Block should be fitted first, and then removed whilst the lower part of the Twin Block is fitted. Once both parts are fitting well and are retentive, they should both be placed in the patient’s mouth, upper first followed by the lower, and the patient should be advised to posture the mandible forward until the lower block slides up in front of the upper block and is held in this postured position. The patient should be advised that this is the position that they must always bite in when the appliance is in place, because otherwise the appliance will not work. It helps to provide lots of positive encouragement by showing the patient and the parent that, in the postured position, the top teeth no longer stick out and it is easier to get the lower lip in front of them.
It is essential that the overjet, molar relationship and canine relationship are measured without the appliance in place and with the mandible in its most retruded position. It is also essential to check that there is sufficient activation with the appliance in place and that the patient’s mandible is being held in at least a Class I relationship, preferably edge-to-edge.
Instructions/advice to Patient/parent/guardian
The generic advice for the wear of removable appliances detailed in Chapter 4 applies to functional appliances as well, although with some additional information:
- The patient should be warned that not only will the teeth feel uncomfortable for a few days, but the sides of the face will be sore as well. This soreness is due to the stretching of the masseter muscle as the mandible is postured and will continue until the fibres of the masseter muscle have increased in length, which takes a few days. It is important to emphasise to the patient and parent that the soreness will only resolve if the appliance is worn well as the ‘muscles need to get used to the new position’. It will not resolve if the appliance is continuously taken in and out.
- Although difficult, it is poss/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


