Periodontium
Anatomic Characteristics and Host Response
Dorothy A. Perry and Phyllis L. Beemsterboer
• Identify the tissues of the periodontium.
• Describe the anatomy and clinical characteristics of the tissues of the periodontium.
• Differentiate among the three types of oral epithelial surfaces: keratinized, parakeratinized, and nonkeratinized.
• List the functions of the periodontal ligament.
• Describe clinically normal gingivae in terms of color, size, contour, texture, and consistency.
• Describe the interactions of the major elements in the host response.
Gingival and periodontal diseases are infectious diseases by nature. The changes these infections bring to the periodontal tissues can best be understood with a basic background in the unique anatomy of the periodontium and knowledge of the response the human body undertakes to protect itself. As will be further explained in Chapter 4 on microbial plaque biofilm and Chapters 6 and 7 devoted to gingival and periodontal diseases, the effects and damage caused by these microbe-induced diseases are complex. They can result in irreversible changes to the normal architecture, loss of teeth, loss of function, and changes in appearance.
Anatomic Characteristics of the Periodontium
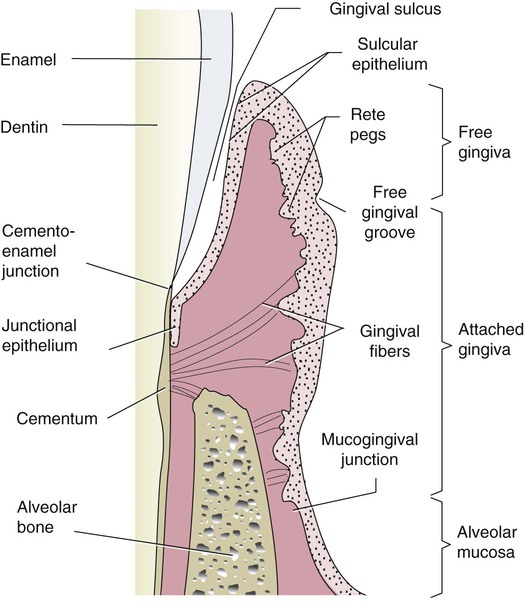
The periodontium is defined simply as the tissues that surround, support, and attach to the teeth. These include the gingiva, periodontal ligament, cementum, and alveolar bone.1 These tissues support the teeth and oral structures. Maintaining the health and function of the periodontium is the most significant factor in the longevity of the dentition.
Gingiva
The gingiva is the visible component of the periodontium inside the mouth. It is described as coral pink,2 pink,3 or pale pink.4 In clinical appearance the color can vary and can appear much darker when melanin pigmentation is present. The gingiva is distinguished from the oral mucosa at the mucogingival junction. This line indicates the transition from the loosely attached and movable oral mucosa to the attached gingiva, which is more firmly attached to the bone by collagen fibers. The attached gingiva is the portion that extends coronally from the mucogingival junction. The width of the attached gingiva varies from individual to individual and from tooth to tooth in the same mouth. The range of widths is 1 to 9 mm,5 with an average of 3.5 to 4.5 mm in the maxilla and 3.3 to 3.9 mm in the mandible. There is usually a thinner band of attached gingiva in the posterior regions. The palatal attached gingiva blends into the palatal gingiva without demarcation.2
Frenum and muscle attachments are present in the gingiva, and those located coronally in the attached gingiva are associated with narrower widths of attached gingiva. The gingiva is keratinized or parakeratinized (discussion follows) tissue on the oral surface, and it is commonly stippled. Nonstippled gingiva is also seen in healthy mouths.2,6 The degree of keratinization varies throughout the epithelium in the mouth, with the palatal gingiva being the most keratinized and the cheek the least. The tongue is also covered with keratinized epithelium. The location of the gingival margin, the edge of the gingiva next to the teeth, in fully erupted healthy teeth is 0.5 to 2 mm coronal to the cementoenamel junction of the teeth (Figure 2-1).3
The free gingiva, or free marginal gingiva, surrounds the tooth and creates a cuff or collar of gingiva extending coronally about 1.5 mm. The surface of the free gingiva next to the tooth forms the gingival wall of the sulcus.2 The free gingiva may be distinguished from the attached gingiva by a free gingival groove, a slight depression on the gingiva corresponding to the depth of the sulcus. This groove varies from tooth to tooth, occurring about 50% of the time, most commonly in the mandibular anterior and premolar areas.6 The free gingiva on buccal and lingual surfaces is often described as ending in a knife-edged tip next to the tooth surface; microscopically the coronal termination of the free gingiva appears more rounded (Figure 2-2).
The papillae are gingivae that fill the embrasures—proximal spaces created below the contact areas of the teeth. They are also referred to as the interdental gingiva. The papillae between anterior teeth are commonly described as pyramidal.4 When the papilla is broad, as is often the case between posterior teeth, there is a nonkeratinized area called the col. This area is a slight depression of tissue between the buccal and lingual interdental papillae. It indicates a fusion of two papillae to cover a wide space. The col is not usually present between anterior teeth. When adjacent teeth do not contact each other, whether they are anterior or posterior teeth, attached gingivae form between the teeth and the papillae and col are absent.2
The gingival epithelium is joined to the underlying connective tissue by a basal lamina, 300 to 400 Å thick. The basal lamina is joined to the connective tissue by fibrils. The connection between the free and attached gingiva and the underlying connective tissue occurs in ridges of epithelium called rete pegs.2
Epithelium
The surface tissue of the oral cavity is made up of stratified squamous epithelium, primarily consisting of cells called keratinocytes, but also including Langerhans cells, Merkel cells, and melanocytes. The function of the epithelium is to protect the underlying structures while allowing some selective interchange with the oral environment.2
The process of keratinization occurs as the keratinocyte migrates from the basal layer to the surface. The cells become increasingly flattened, develop keratohyaline granules in the subsurface, and produce a superficial layer that is similar to skin where no cell nuclei are present. In some cases, the epithelium shows signs of being keratinized, yet the cells of the superficial layers retain their nuclei. This surface is called a parakeratinized epithelium. If no signs of keratinization are present, the epithelial surface is considered nonkeratinized.3 Keratinized, parakeratinized, and nonkeratinized gingivae are all found in the oral cavity.
Langerhans cells are considered to be part of the phagocytic system, and Merkel cells contain nerve endings and are associated with tactile sensitivity. Melanocytes are located in the basal layers of the epithelium and contain substances that convert to melanin. Melanin is phagocytized and remains within the cells of the epithelium, giving a pigmented appearance to the epithelium.2 Figure 2-3 is an example of a normal gingiva with extensive melanin pigmentation.
Oral or Outer Epithelium
The oral epithelium is also called the outer gingival epithelium.4 It is composed of the attached gingiva, the papillae, and the outer surface of the free gingiva. It covers the crest of the gingiva, the free gingiva, and the attached gingiva. This can be clearly seen in Figure 2-2. Microscopic rete pegs project into the connective tissue below. The oral epithelium’s function is protective, and the epithelium is typically parakeratinized.2
Sulcular Epithelium
The sulcular epithelium is the thin nonkeratinized, or parakeratinized, epithelium extending from the outer epithelium into the gingival sulcus. It may be parakeratinized near the opening to the oral cavity. The sulcular epithelium is found from the height of the gingiva along the inner surface of the sulcus extending to the junctional epithelium; it forms the gingival wall of the sulcus (Figure 2-4). In a healthy state, the epithelium lining the sulcus is smooth and intact; there are no rete pegs projecting into the connective tissue. The sulcular epithelium is also permeable and gingival crevicular fluid, made up of the components of the serum and other cells, is secreted through it into the sulcus.
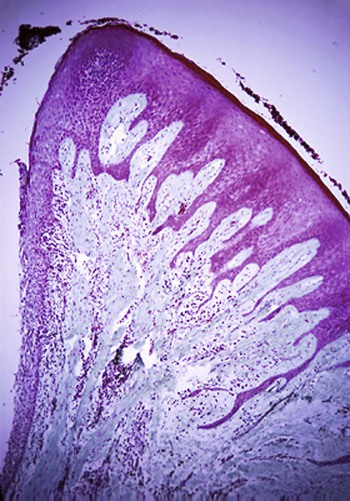
Rete pegs are seen subjacent to the oral epithelium but not the sulcular epithelium. (Courtesy of Dr. Gary C. Armitage.)
The healthy sulcus is generally 1 to 3 mm deep. However, the sulcus depth determined clinically by measurement with a periodontal probe may be considerably different than the histologic sulcus depth. Probe measurements are subject to variation as a result of several influences: the probe insertion pressure, the ability of the probe tip to penetrate tissue, and the accuracy of the clinician reading the probe measurements.5 For this reason, Löe and colleagues3 suggested that the use of the term sulcus depth in reference to probe readings is misleading. A more accurate term would be probing depth or probable depth of the gingival sulcus.
Sulcular or Gingival Crevicular Fluid.
Gingival crevicular fluid, also referred to as sulcular fluid or simply gingival fluid, flows from the underlying connective tissue into the sulcus. The amount of flow is related to the permeability of the connective tissue capillaries beneath the surface of the sulcular epithelium. The fluid escapes from the capillaries and seeps out between the epithelial cells into the sulcus. The amount of fluid flow is small, considered to be minimal to none in the healthy state.4 Gingival fluid is believed to perform several functions: cleansing the sulcus, improving epithelial cell adherence to the tooth surface, and possessing antimicrobial and immune properties.2,6
Junctional Epithelium
The junctional epithelium separates the periodontal ligament from the oral environment. It is composed of nonkeratinized, stratified, squamous epithelial cells that adhere organically to tooth structure, and its function is considered to be protection of the attachment of the tooth to the surrounding tissues. It forms a layer that is 15 or 20 cells thick at the coronal end and narrows to a few cells thick at the apical termination. Its length in the healthy state ranges from 0.25 to 1.35 mm.4,6 This epithelium continually renews itself, and its most coronal portion determines the histologic base of the gingival sulcus.7,8 The attachment of the junctional epithelium to the root surface is enhanced by fibers from the connective tissue. This attachment supports the free marginal gingival and it is considered to be a functional unit, called the dentogingival unit.2,6
Gingival Connective Tissue
The connective tissue beneath the gingiva is called the lamina propria. The lamina propria is made up of two layers: the papillary layer that is immediately beneath the epithelium, which consists of papillary projections between the rete pegs, and the reticular layer, which extends to the periosteum.6 Approximately 60% of the lamina propria is made up of connective tissue that is composed of collagen fibrils that form discrete fiber bundles.8 Other elements include cells such as fibroblasts, undifferentiated mesenchymal cells, mast cells, and macrophages as well as blood vessels and nerves.3
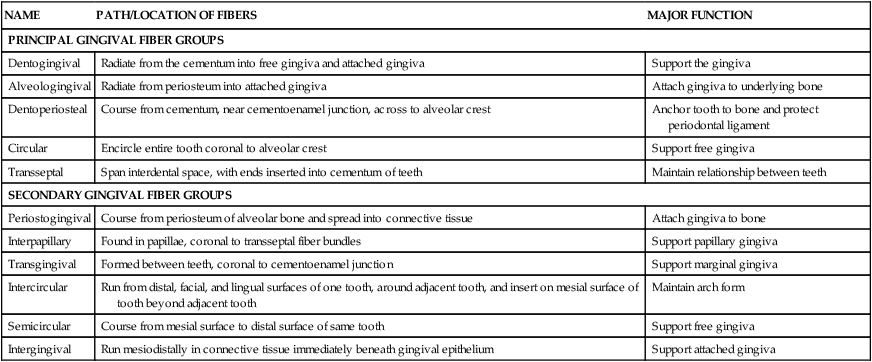
The fiber bundles are known as the gingival ligament.8 These are not individual fibers, but fiber bundles, although they are commonly referred to as fibers. Their functions include protecting and supporting the junctional epithelium, maintaining the tone of the attached gingiva, and protecting the periodontal ligament. There are five principal fiber groups and six minor groups. All bundles are discrete, although fibrils often intertwine so that the gingival ligament supports its components. The bundles are best described by their orientation and attachment. These characteristics suggest the function of the specific bundle, although all are interdependent and no doubt share functions. The gingival fiber bundles are very important because they provide the most coronal connective tissue attachment for the teeth. Both principal and secondary fiber bundles have been described. Their locations and functions are listed in Table 2-1.
TABLE 2-1
| NAME | PATH/LOCATION OF FIBERS | MAJOR FUNCTION |
| PRINCIPAL GINGIVAL FIBER GROUPS | ||
| Dentogingival | Radiate from the cementum into free gingiva and attached gingiva | Support the gingiva |
| Alveologingival | Radiate from periosteum into attached gingiva | Attach gingiva to underlying bone |
| Dentoperiosteal | Course from cementum, near cementoenamel junction, across to alveolar crest | Anchor tooth to bone and protect periodontal ligament |
| Circular | Encircle entire tooth coronal to alveolar crest | Support free gingiva |
| Transseptal | Span interdental space, with ends inserted into cementum of teeth | Maintain relationship between teeth |
| SECONDARY GINGIVAL FIBER GROUPS | ||
| Periostogingival | Course from periosteum of alveolar bone and spread into connective tissue | Attach gingiva to bone |
| Interpapillary | Found in papillae, coronal to transseptal fiber bundles | Support papillary gingiva |
| Transgingival | Formed between teeth, coronal to cementoenamel junction | Support marginal gingiva |
| Intercircular | Run from distal, facial, and lingual surfaces of one tooth, around adjacent tooth, and insert on mesial surface of tooth beyond adjacent tooth | Maintain arch form |
| Semicircular | Course from mesial surface to distal surface of same tooth | Support free gingiva |
| Intergingival | Run mesiodistally in connective tissue immediately beneath gingival epithelium | Support attached gingiva |
Periodontal Ligament
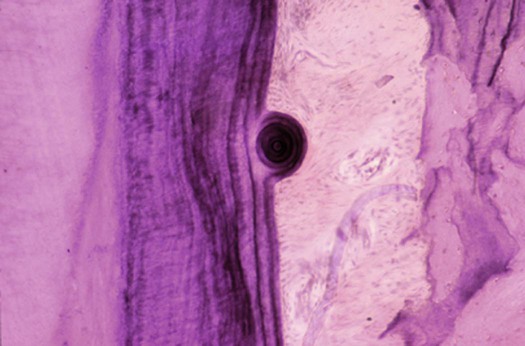
Teeth are not attached rigidly to the bone in humans and other mammals. The periodontal ligament provides a suspensory cushion in the 0.4- to 1.5-mm space between the surface of the tooth and the bone. The periodontal ligament is a connective tissue complex primarily filled with fiber bundles and cells.8 The cells in the ligament perform an important formative function for the tissues; they generate a pericementum for the cemental surface of the root and a periosteum for the bone.9 Unusual formations of cementum, called cementicles, can also occur in the periodontal ligament (Figure 2-5). These develop from calcified material in the periodontal ligament or from traumatically displaced bits of cementum or bone.10
The specific functions of the periodontal ligament include the following8,10:
• Fibrous tissue development and maintenance
• Calcified tissue development and maintenance
• Nutritive and metabolite transport
• Sensory functions, including touch, pressure, pain, and proprioception (displacement sensitivity)
Fiber Bundles
The fiber bundles in the periodontal ligament are made of collagen, arranged in bundles, and are spread throughout the periodontal ligament with the other cellular, vascular, and nerve tissues. In addition to attaching the tooth to the bone, they are believed to transmit occlusal forces to the bone, resist occlusal forces (the “shock absorber” effect), and protect the vessels and nerves from injury.10
Five principal fiber bundles in the periodontal ligament are summarized in Table 2-2. The principal fiber bundles are attached to the cementum with brush like fibers called Sharpey’s fibers, course from the cementum across the periodontal ligament, and terminate in the alveolar bone as Sharpey’s fibers.8,10
TABLE 2-2
Periodontal Ligament Fiber Bundle Groups
| PERIODONTAL LIGAMENT BUNDLE GROUP | PATH and LOCATION OF FIBERS | MAJOR FUNCTION |
| Alveolar crest | Runs from cementum, just apical to cementoenamel junction, to crestal bone | Retains tooth in socket; opposes lateral forces |
| Horizontal | Directly across periodontal ligament space | Attaches root surface to alveolar bone |
| Oblique | Courses in oblique direction across periodontal ligament space and into alveolar bone | Largest group of fiber bundles; transfers occlusal stresses to bone |
| Apical | Runs from apex of root into alveolar bone, both apical and lateral to root apex | Probably suspensory because it does not occur in erupting teeth |
| Interradicular | Spreads apically into bone, from furcation | Probably suspensory and protection of interradicular bone; present only in multirooted teeth |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses