Chapter 2
How Does Plaque Cause Disease?
Aim
The concept that plaque causes gingivitis is a fact, proven by a series of studies in the 1960s. Whether plaque causes periodontitis is a different debate. Without plaque bacteria, inflammatory periodontitis would not occur, but in the presence of plaque bacteria, periodontitis often does not occur. This chapter aims to explain the mechanisms by which periodontal microorganisms may cause disease in a susceptible host, given the right circumstances.
Outcome
The outcome of reading this chapter will be that the reader will understand the microbial basis for contemporary and future periodontal therapies. The reader will also appreciate the complexities of a poly-microbial infection, as opposed to mono-infections like HIV or TB, and why the use of systemic antibiotics in periodontal management is of limited benefit for all but a limited number of patients.
A Model for Periodontal Disease Pathogenesis
Whether periodontitis develops in an individual depends upon a myriad of complex issues collectively called “risk factors” (see Chapter 4). Unlike gingivitis, which develops in the majority of, if not all, humans, periodontitis is multi-factorial and cannot be regarded as a pure infection like HIV disease or TB. It is polymicrobial (Fig 2-1) and there are many “host factors” (see Chapter 3), some genetically determined and some environmentally determined, which impact on the following clinical issues:
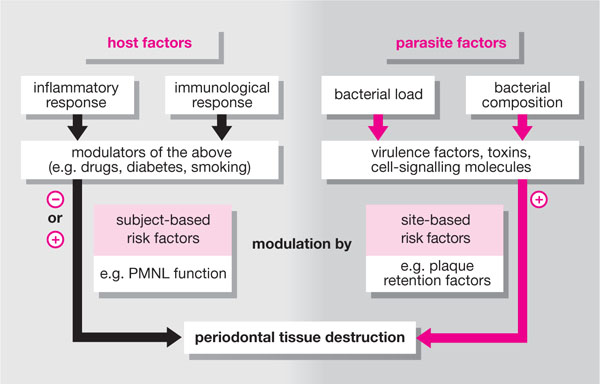
Fig 2-1 Schematic diagram showing how a delicate balance can exist between periodontal bacteria and the host. Tissue damage can result from bacteria overpowering the immune response or from products of the host’s own inflammatory-immune response, if this is exaggerated. On top of this are a large number of modifying or risk factors which can exist at the individual patient or systemic level, or at the individual periodontal site level (Chapter 4).
-
Will periodontal disease develop in this patient?
-
If so, at what age will it develop?
-
What type of disease will develop? (“classification” – see Chapter 6)
-
At what rate will the disease progress?
-
What pattern of disease progression should we look for? (see Chapter 5)
-
How will this patient respond to therapy?
-
What is the most appropriate therapy for this case?
-
Will teeth be lost? And if so, how many?
-
May there be systemic consequences of the disease process or its treatment?
Without bacteria there would be no periodontal disease, but bacteria are essential to maintain health and of the 700-plus species already known to exist in the oral cavity (some 400–500 colonising the periodontal tissues), only a few cause disease.
A “pathogen” is an organism that causes disease.
A “commensal” is a non-disease-forming organism; part of the resident flora.
“Opportunist pathogens” are normally not pathogenic, but are able to become so if their local environment is changed (e.g. by antibiotic therapy eliminating competing bacteria, or in an immunocompromised host). They can overgrow and the “microbial load” that results can cause disease.
How Do Bacteria Cause Disease?
Bacteria normally cause disease when the following basic sequences occur:
-
acquisition
-
adherence or retention
-
initial survival
-
prosperity and longer-term survival
-
avoidance of elimination
-
multiplication
-
elaboration of “virulence factors”.
Acquisition of oral bacteria occurs at birth from parental (called vertical transmission) and other environmental sources. This has led to the concept of endogenous organisms (already present in the host when the disease develops) and exogenous organisms (those acquired from other individuals or the environment, which may initiate the disease process or enable its progression). In 1993, Van Steenbergen and colleagues used genetic fingerprinting methods to demonstrate that periodontal pathogens like Actinobacillus actinomycetem-comitans (Aa) and Porphyromonas gingivalis (Pg) can be transmitted between individuals within families. In one study in 1988 by Preus and Olsen, transmission between an adolescent and the family dog was demonstrated. However, in chronic periodontitis it is likely that causative organisms are endogenous. If exogenous sources become involved, chronic exposure is necessary for colonisation of the new host. Whilst periodontal disease is not thought to be transmitted by kissing, it is worth remembering that repeated failure of periodontal therapy in an individual may be due to re-infection from chronic contact with a partner.
Adherence/retention describes the ability of an organism to attach to a surface, and is essential for bacterial survival unless the bacteria are plank-tonic (able to swim and survive in a dynamic manner). It is for this reason that the eruption of teeth in mammals provides a non-shedding, stable surface for organisms to adhere to. The first organisms to adhere to the glyco-protein pellicle that forms on crown surfaces within minutes of removal are called “pioneer” organisms. Gram-positive cocci like “streptococci” have this ability via production of mucopolysaccharides, and gram-negative organisms possess cell wall components called lipoteichoic acids, which facilitate adhesion. Such mechanisms also assist the retention of organisms in environments where physical adhesion is not an absolute requirement for colonisation, e.g. habitats not exposed to physical forces such as salivary flow.
Initial survival of an organism not only requires adhesion to a static surface, but also requires the acquisition of essential nutrients. The production of an extracellular matrix (comprising dextrans and levans) facilitates attachment to the tooth surface. Additionally, plaque adhering at the gingival margin and interproximally is more resistant to physical removal by the forces of the oral musculature, food particles and washing by saliva. Within the gingival crevice, GCF is rich in all serum components, including glucose (raised in GCF in hyperglycaemic individuals) and iron. The crevice is, nevertheless, a hostile environment since GCF also contains iron-binding proteins like transferrin, haptoglobin and haemoglobin, as well as antibody and complement.
Prosperity and longer-term survival within the gingival crevice requires the bacteria to be able to survive relatively harmoniously with their neighbours in a “biofilm”. A biofilm is a complex structure within which there are areas of high and low bacterial mass, interlaced with aqueous channels. Biofilms (Fig 2-2) function like multicellular organisms characterised by shedding of bacterial surface components (e.g. antigens, which can activate a host immune response) and release of various toxins (e.g. endotoxin, which activates a host inflammatory response). Within this environment, bacteria are capable of an activity called “quorum sensing”, which is simply being able to respond to products or signals from other biofilm organisms, or the host, and to use these to grow and prosper; some organisms physically adhere to each other (Fig 2-3).
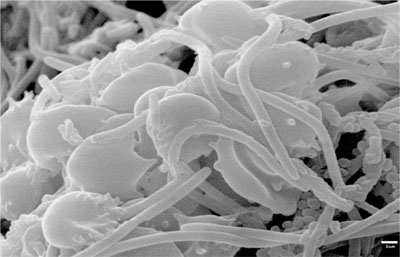
Fig 2-2 A scanning electron micrograph (SEM) of a microbial biofilm demonstrating the intimate relationship of motile organisms with static organisms. Rod-shaped organisms can be seen along with cocci, filamantous bacteria and spirochaetes and blood cells from the host.
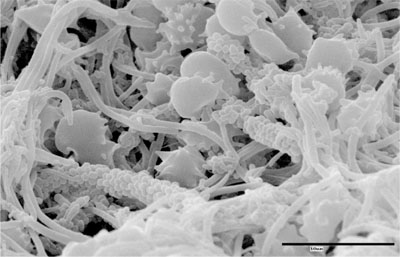
Fig 2-3 SEM showing intimate relationship of bacteria within a biofilm. The alignment of cocci along the length of a filament is called a “corn-on-the-cob” relationship.
Avoidance of elimination by the host defence system is a key strategy of all pathogens. Bacterial capsules can facilitate this and some organisms undergo genetic “shift and drift” whereby certain surface antigens mutate such that host antibodies can no longer recognise and bind to them. Aa produces:
-
leucotoxin (an exotoxin) that destroys polymorphonuclear leucocytes (PMNLs or neutrophils)
-
epitheliotoxin
-
/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


