Chapter 4
Risk Assessment
Aim
Risk assessment has become a fundamental strategy employed when assessing any disease process and its subsequent management. This chapter aims to explain what risk factors are and how they differ from risk markers and risk patients. The most important risk factors for periodontitis will be discussed and a simple protocol outlined that will enable practitioners to account for risk factors in their periodontal patients, when formulating diagnoses, treatment plans and maintenance regimes.
Outcome
Having read this chapter the reader will appreciate the importance of the role of risk factor analysis in periodontal assessment and how such information informs diagnostic, treatment planning and maintenance strategies. It is hoped that the reader will also understand the key risk factors for periodontal disease and be able to implement a simple, rapid system of assessment within their daily practice.
Risk Assessment
Risk management is a term used in many working environments to describe the formalisation of a series of safety protocols that put common sense into practice. For example, the presence of a step at the threshold of a doorway leading from the waiting area to the surgery is likely to increase the risk of a patient tripping as they enter the surgery. Risk management would involve the practitioner identifying the risk during a formal risk assessment for their practice, and erecting a sign to draw patients’ attention to it. Failure to do so could result in injury to a patient and a claim against the practice. The situation in periodontology is similar, since failure to identify proven risk factors for periodontitis results in failure to inform and educate the patient in fundamental issues relating to the disease process in their mouths. Furthermore, given that some risk factors can be modified or eliminated by the patient, e.g. smoking habit or level of diabetic control, practitioners have a duty of care to counsel patients appropriately about their role in the management of their periodontal disease. Management of periodontitis is a contract between the dental surgeon and the patient in which the successful outcome of therapy is dependent equally upon the patient doing “their bit” as it is on the dental team performing their duties to the highest possible standard.
Risk Factors
A risk factor is a factor that increases the probability that a disease may develop in an individual. Risk factors are biologically related to the occurrence of the disease, but they do not necessarily imply cause and effect: i.e. just because a patient possesses a risk factor does not mean that they will definitely develop the disease. Equally, absence of a risk factor does not mean that the disease will not develop. The majority of scientists advocate a two-stage model for disease development, in which a subject must possess genetic risk factors for a disease and then acquire environmental risk factors capable of exploiting that individual’s inherent susceptibility to the disease. In periodontitis, risk factors are believed to modify the basic pathogenic process (Fig 4-1) and such risk factors result in a direct increase in the probability of acquiring the disease. They may be broadly categorised as:
-
Systemic risk factors (or “subject-based”) – factors affecting one of the subject’s “systems”, which essentially affect the host-response to the plaque biofilm, upsetting the host-microbial balance (Fig 3-2).
-
Local risk factors (or “site-based”) – factors local to the oral cavity, which may influence plaque accumulation or occlusal forces.
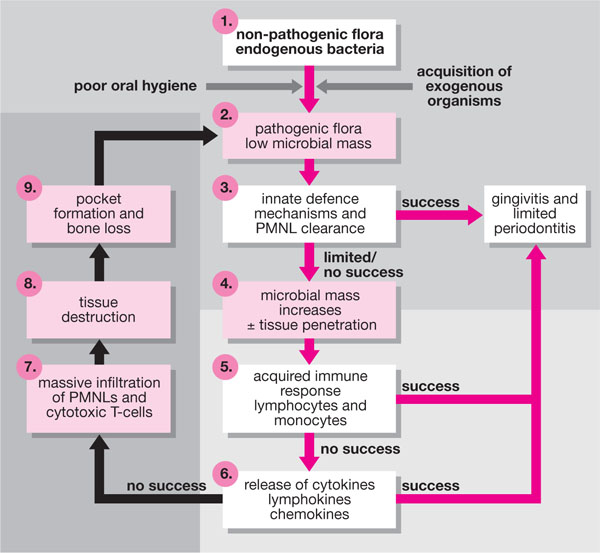
Fig 4-1 The “critical pathway model” for periodontal disease pathogenesis modified from Salvi et al. 1997.
Risk Markers
Risk markers or predictors are not linked to “causation”, but their presence is more a consequence of the disease being present. Risk markers imply the presence of disease and are often used to detect early stages of disease, before overt clinical signs become apparent. Examples would be the sign of bleeding on probing (BOP), tooth mobility, recession, suppuration, past disease experience, etc. (see Chapters 6 and 8).
Risk Patients
A risk patient is one who has a high probability of developing a disease over a specific period of time. Such patients either possess or have been exposed to “risk factors” for that disease. Therefore, a patient who smokes 30 cigarettes per day and has poor oral hygiene must be regarded as a risk patient for the development of periodontitis or necrotising ulcerative gingivitis (NUG) (see Chapter 6).
To help understand the role of risk factors, a model of disease pathogenesis that has been termed the “critical pathway model of pathogenesis” was developed by Offenbacher in 1996 (Fig 4-1). The model encompasses both the microbial and host components that contribute to periodontal destruction (Fig 2-1), but identifies nine key or critical stages in the process which must occur for disease development and progression. Each cycle of the closed loop represents further tissue destruction and risk factors may either lead to progress from one stage to the next within the loop, or to additional turns of the cycle. Equally, any critical stage may be reversed by successful host responses, or by elimination of risk factors.
Multi-Level Risk Assessment
One of the problems with risk assessment in periodontal disease is that the diseases are multifactorial and assessment should therefore be at multiple levels. The presence of pathogenic bacteria alone is not sufficient to cause the disease. In simple terms, there are four levels to consider:
-
The patient level Perform at initial examination.
-
The whole mouth level Perform at initial examination and post-initial therapy.
-
The tooth level Perform post initial/definitive therapy and maintenance.
-
The site level Perform post definitive therapy and during maintenance.
This approach also allows the clinician to separate risk factors that may initiate periodontal disease from those responsible for its progression or for the failure of initial therapy. A practical view to the application of the above is illustrated in Fig 4-2.
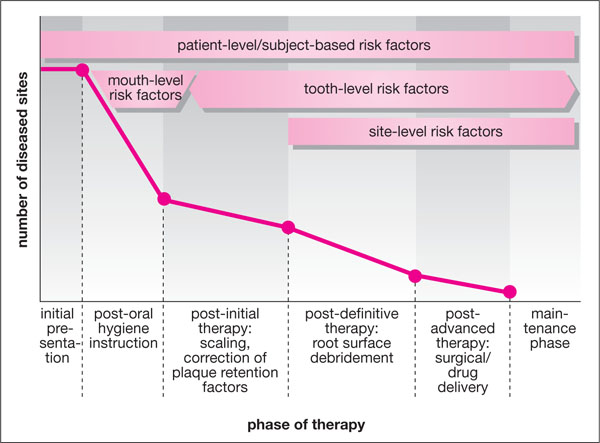
Fig 4-2 The potential effectiveness of different stages of periodontal therapy, and how levels of multiple risk assessment can apply to each stage.
Patient-level risk assessment
Patient-level risk assessment can be determined at the initial consultation by performing the following:
-
Family history (for hereditary/inborn/genetic risk factors). “Is there a history of gum disease or pyorrhoea in the family – parents/grandparents – or early tooth loss?”
-
Medical history (for systemic diseases, e.g. diabetes).
-
Present dental history (assess motivation to oral hygiene, etc.).
-
Social history (smoking – current or former smoker).
-
Habits (bruxism).
The majority of practitioners routinely collect such information, but its formal recording is recommended, perhaps alongside the diagnosis. For example, the use of a tick-box system with four key systemic risk factors would formalise this process (Fig 4-3).
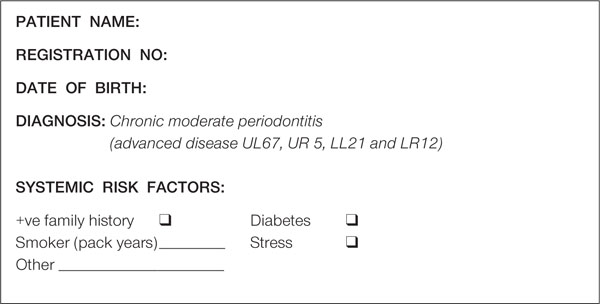
Fig 4-3 A simple tick-box system, which can be incorporated into an ink stamp and stamped in a susceptible patient’s notes formally to record risk factors.
Mouth-level risk assessment
Mouth-level risk assessment would be performed at the initial examination, after a Basic Periodontal Examination (BPE) for susceptibility – as recommended by the British Society of Periodontology (Chapter 7) – and would include:
-
Examination of attachment loss relative to age. This gives a very good idea of previous/current rates of progression and thus the likelihood of future rates of progression. It is important to remember that rapid progression of local lesions may still occur, despite a low age-related disease experience.
-
Occlusal examination in static relationship (occlusal class, tooth wear, etc). A class 2 division II malocclusion with retroclined lower incisors can create hygiene problems for lingual surfaces of those teeth.
-
Occlusal examination in dynamic relationship (patterns of guidance). Secondary occlusal trauma is trauma to a tooth that is already periodontally diseased, and can accelerate the disease process, but does not initiate it (Fig 4-4).
-
Examination of levels of oral hygiene (Fig 4-5). A subject with periodontitis but excellent oral hygiene represents a greater risk of further disease progression than a subject with periodontitis and poor oral hygiene.
-
Examination of levels of plaque-retentive factors (heavily restored mouth, quality of restorations, levels of calculus).
-
Presence of removable prosthesis. A well-designed bridge is less plaque retentive and more desirable than a removable partial denture (Fig 4-6).
-
Levels of recession. The greater the degree of recession, the greater the surface area to clean and hence the greater risk of leaving plaque (Fig 4-7).
-
Gingival tissue quality and extent of pocketing relative to levels of plaque in the mouth (Fig 4-8). Some patients appear resistant to periodontitis.

Fig 4-4 (a) A tooth subject to secondary occlusal trauma, as demonstrated by “crescentic” pattern of bone loss. In this situation, treatment of the periodontitis must take priority.
(b) A tooth subject to primary occlusal trauma demonstrates widening of the periodontal ligament space and early “funnelling”. Elimination of the trauma will result in total bony resolution.

Fig 4-5 Some formal recording of hygiene levels is important medicolegally, but from a patient motivation standpoint, disclosing is essential and dichotomous chart recording of “presence/absence” is essential.
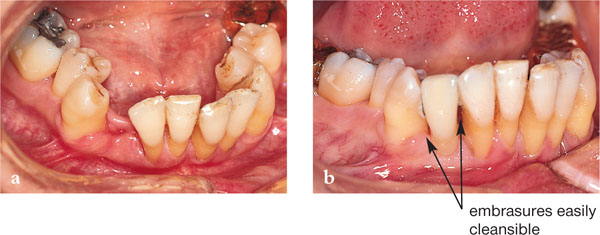
Fig 4-6 An adhesive bridge designed to enable good inter-proximal plaque control in a periodontitis patient, currently on successful maintenance having quit a smoking habit and after full-mouth-open debridement.

Fig 4-7 This subject has no pocketing or BOP, but excessive force during oral hygiene has resulted in attachment loss and a very large surface area to retain plaque free. The UL 6 has required root canal therapy.

Fig 4-8 This subject demonstrates extreme oral neglect, but has no periodontal bone loss or pocketing. He/she is apparently resistant to periodontitis.
Tooth-level risk assessment
Tooth-level risk assessment may or may not be carried out at the initial examination, once a BPE screen had identified a susceptible patient. In the latter situation, detailed periodontal charts and a detailed radiographic assessment and radiological report should be performed (Chapters 8 and 9). Part of this assessment would include:
-
Individual tooth mobility (mobility index). Excessive mobility may compromise patient function or make a tooth susceptible to sub-luxation.
-
Tooth movement or drifting. Periodontally compromised teeth may move under parafunction, a situation often seen with maxillary anterior teeth and a common presenting complaint.
-
Residual tooth support (radiographically). The ext/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


