Endodontics
Chapter Contents
Overview
The field of endodontics has experienced rapid growth over recent years. In particular, there has been a dramatic evolution in the technology available to help in treatment. These developments have, however, not changed the fundamental reasons for treatment, that is pulpal and periradicular disease which is principally bacterial in origin. The aim of treatment therefore is to eliminate these bacteria from within the complex anatomy of root canal systems and seal the canal space to prevent re-entry.
This chapter on endodontics initially provides an overview of pulpal and periradicular disease and the methods used in its diagnosis. This is followed by a review of both traditional and some of the more recent treatment developments that have proved useful in day-to-day practice. Root canal treatment is not always successful; thus, there is a requirement for knowledge of reroot canal treatment procedures and periradicular surgery. The chapter concludes with a review of some of the key aspects of restoration of the endodontically treated tooth.
2.1 Pulpal and periradicular pathology
Pulpal or periradicular inflammation results from irritation or injury usually from bacterial, mechanical or chemical sources.
Bacteria
Bacteria, usually from dental caries, are the main sources of injury to the pulpal and periradicular tissues and these enter either directly or through dentine tubules. The link between bacteria and pulpal and periradicular disease is well established as periradicular pathology does not develop in the absence of bacteria. Modes of entry for bacteria other than caries include periodontal disease (dentine tubules, furcal canals, lateral canals), erosion, attrition and abrasion (dentinal tubules), trauma with or without pulpal exposure, developmental anomalies and anachoresis (the passage of micro-organisms into the root canal system from the bloodstream).
Mechanical irritants
Examples of mechanical irritation include trauma, operative procedures, excessive orthodontic forces, subgingival scaling and overinstrumentation using root canal instruments.
Chemical irritants
Pulpal irritation may result from bacterial toxins or some restorative materials/conditioning agents. Periradicular irritation may occur from irrigating solutions, phenol-based intracanal medicaments or extrusion of root canal filling materials.
Pulp disease
Irritation from any of the above sources causes some degree of inflammation. The response of the pulp depends on the severity of the insult and may result in a transient (reversible) inflammatory response or an irreversible one, which will eventually proceed to pulp necrosis.
Classification of pulp disease
There is an inconsistent correlation between clinical symptoms and histological findings in pulpal disease. Diagnoses are, therefore, usually based on patient symptoms and clinical findings. Pulpal disease may result in changes to both the soft and hard tissues.
Soft tissue changes
Reversible pulpitis
Reversible pulpitis is a transient condition that may be precipitated by caries, erosion, attrition, abrasion, operative procedures, scaling or mild trauma. The symptoms are usually the following:
• Pain does not linger after the stimulus is removed.
• Pain is difficult to localise (as the pulp does not contain proprioceptive fibres).
• Normal periradicular radiographic appearance.
• Teeth are not tender to percussion (unless occlusal trauma is present).
Treatment involves covering up exposed dentine, removing the stimulus or dressing the tooth as appropriate. Reversible pulpitis may progress to an irreversible situation.
Irreversible pulpitis
Irreversible pulpitis usually occurs as a result of more severe insults of the type listed above; typically, it may develop as a progression from a reversible state. The symptoms are, however, different:
• Pain may develop spontaneously or from stimuli.
• In the latter stages, heat may be more significant.
• Response lasts from minutes to hours.
• When the periodontal ligament becomes involved, the pain will be localised.
• A widened periodontal ligament may be seen radiographically in the later stages.
Treatment involves either root canal therapy or extraction of the tooth.
Hyperplastic pulpitis
Hyperplastic pulpitis is a form of irreversible pulpitis and is also known as a pulp polyp. It occurs as a result of proliferation of chronically inflamed young pulp tissue. Treatment involves root canal therapy or extraction.
Pulp necrosis
Pulp necrosis occurs as the end result of irreversible pulpitis; treatment involves root canal therapy or extraction.
Hard tissue changes
Pulp calcification
Physiological secondary dentine is formed after tooth eruption and the completion of root development. It is deposited on the floor and ceiling of the pulp chamber rather than the walls and with time can result in occlusion of the pulp chamber. Tertiary dentine is laid down in response to environmental stimuli as reactionary or reparative dentine. Reactionary dentine is a response to a mild noxious stimulus whereas reparative dentine is deposited directly beneath the path of injured dentinal tubules as a response to strong noxious stimuli. Treatment is dependent upon the pulpal symptoms.
Internal resorption
Occasionally, pulpal inflammation may cause changes that result in dentinoclastic activity. Such changes result in resorption of dentine; clinically, a pink spot may be seen in the later stages if the lesion is coronal. Radiographic examination reveals a punched out outline that is seen to be continuous with the rest of the pulp cavity. Root canal therapy will result in arrest of the resorptive process; however, if destruction is very advanced, extraction may be required.
Classification of periapical disease
Acute apical periodontitis
Causes of acute apical periodontitis include occlusal trauma, egress of bacteria from infected pulps, toxins from necrotic pulps, chemicals, irrigants or overinstrumentation in root canal therapy. Clinically, the tooth is tender to biting. Widening of the periodontal space may be seen on a radiograph. Treatment depends on the pulpal diagnosis; it may range from occlusal adjustment to root canal therapy or extraction.
Chronic apical periodontitis
Chronic apical periodontitis occurs as a result of pulp necrosis. Affected teeth do not respond to pulp sensitivity tests. Tenderness to biting, if present, is usually mild; however, some tenderness may be noted to palpation over the root apex. Radiographic appearance is varied, ranging from minimal widening of the periodontal ligament space to a large area of destruction of periapical tissues. Treatment involves root canal therapy or extraction.
Condensing osteitis
Condensing osteitis is a variant of chronic apical periodontitis and represents a diffuse increase in trabecular bone in response to irritation. Radiographically, a concentric radio-opaque area is seen around the offending root. Treatment is only required if symptoms/pulpal diagnosis indicate a need.
Acute apical abscess
An acute apical abscess is a severe inflammatory response to micro-organisms or their irritants that have leached out into the periradicular tissues. Symptoms vary from moderate discomfort or swelling to systemic involvement, such as raised temperature and malaise. Teeth involved are usually tender to both palpation and percussion. Radiographic changes are variable depending on the amount of periradicular destruction already present; however, usually there is a well-defined radiolucent area, as in many situations an acute apical abscess is an acute exacerbation of a chronic situation. One well-recognised event (although not a diagnosis) is that of a phoenix abscess, which refers to an acute exacerbation of a chronic situation during treatment. Initial treatment of an acute apical abscess involves removal of the cause as soon as possible. Drainage should be established either by opening the tooth or incision into a dependent swelling. An antibiotic may need to be prescribed, depending on the patient’s condition. Once the acute symptoms have subsided, then root canal therapy or extraction may be performed.
Chronic apical abscess
In a chronic apical abscess, the abscess has formed a communication through which it discharges. Such communications may be through an intraoral sinus or, less commonly, extraorally. Alternatively, the discharge may be along the periodontal ligament; such cases mimic a periodontal pocket. Usually, these communications or tracts heal spontaneously following root canal therapy or extraction.
Lesions of non-endodontic origin visualised radiographically
Although lesions noted on radiographs are usually of endodontic origin, this is not always the case. Other causes may be normal anatomic structures, benign or malignant lesions. (The following list is not exhaustive and readers should refer to an appropriate text on oral pathology.)
Certain normal anatomic structures may mimic radiolucencies (e.g. maxillary sinus, mental foramen, nasopalatine foramen). In these situations, the associated teeth will respond normally to pulp sensitivity tests and a radiograph taken from a different angle will reveal that the lesion is not so closely related to the root.
Benign lesions that may mimic endodontic pathology include cementoma, fibrous dysplasia, ossifying fibroma, primordial cyst, lateral periodontal cyst, dentigerous cyst, traumatic bone cyst, central giant cell granuloma, central haemangioma and ameloblastoma. Usually, in such situations, the lamina dura will be intact around the teeth and final diagnosis relies on appropriate biopsy.
Malignant lesions to be aware of include squamous cell carcinoma, osteosarcoma, chondrosarcoma and multiple myeloma. These lesions are usually associated with rapid hard tissue destruction.
2.2 Patient assessment
Successful endodontic diagnosis requires a systematic approach to the history and clinical examination, followed by the use of appropriate diagnostic aids. Finally, careful planning of the treatment strategy is essential.
The most common cause of orofacial pain is pulpal or periradicular disease. However, it should be remembered that the periodontium, sinuses, temporomandibular joints, muscles of mastication, ears, nose, eyes and blood vessels may also be affected by lesions that can mimic pain of pulpal origin.
History
Presenting complaint
The aim of this stage is to record the patient’s symptoms or problems, preferably in their own words.
Medical history
An up-to-date medical history should be taken for each new patient or be updated for previously registered patients, dated and signed.
Dental history
The purpose of the dental history is to summarise current and past dental treatment. Such information may provide clues as to the source of the patient’s complaints. It is also an opportunity to establish the patient’s attitude towards dental health and treatment as these findings may affect treatment decisions/planning (Section 1.2).
Pain history
Initially, information on pain is obtained by asking questions regarding the current problem(s). This examination is subjective; frequently asked questions include the following:
Provisional diagnosis
The history and identification of signs and symptoms may help the clinician to reach a provisional diagnosis. The clinical examination gathers the information necessary to confirm or modify this diagnosis.
Clinical examination
Extraoral examination
The patient’s general appearance and wellbeing are assessed. A note is made of any swelling, redness or extraoral sinuses. Lymph nodes are palpated for enlargement and/or tenderness. Muscles of mastication and temporomandibular joints are also palpated for tenderness and a note made of the degree of mouth opening.
Intraoral soft tissues
The oral mucosa and gingival tissues are examined for discoloration, inflammatory change and sinus tract formation. A basic periodontal examination is performed (Section 1.2).
Intraoral hard tissues
Teeth are examined for caries, large restorations, crowns, discoloration, fracture, attrition, abrasion, erosion and restorability.
Special tests
All special tests have their limitations and require care in the way they are performed and interpreted. The objective is to find the tooth that is causing the discomfort. In general, healthy (control) teeth are tested first.
Percussion
Percussion refers to gently tapping or pressing the occlusal or lateral surface of a tooth. A painful response indicates periradicular inflammation. The region over the apices of teeth may also be palpated. Tenderness may be an indication of inflammation, although care should be taken in interpretation when apices are close to the surface.
Mobility
A mirror handle is placed on one side of the tooth and a note made of the degree of movement: up to 1 mm scores 1, over 1 mm scores 2 and vertically mobile teeth score 3.
Occlusal analysis
It is important to examine suspect teeth for interferences on the retruded arc of closure, intercuspal position and lateral excursions. Interferences in any of these positions could result in a degree of occlusal trauma and institute acute apical periodontitis.
Pulp sensitivity tests
Pulp sensitivity tests determine the response to stimuli and may identify the offending tooth. It is usual to try to mimic the stimulus that initiates the pain. Pulp sensitivity testing may help to distinguish between an infection of periodontal or endodontic origin when a periodontal–endodontal communication is present. Thermal tests are usually the most useful as they give an indication not only as to whether the pulp is alive but also how healthy it is.
Cold test
Dry ice, EndoIce or ethyl chloride spray on a cotton pledget or ice sticks may be used to mimic cold stimuli.
Hot test
Hot gutta-percha or hot water after the application of rubber dam may be used to mimic hot stimuli.
Electric pulp test
Electric instruments can provide an indication as to whether or not there is vital nerve tissue in the tooth; they do not give an indication of different stages of degeneration.
Sinus tract exploration
Where a sinus tract is present, it may be possible to insert a small gutta-percha point. A radiograph is then taken to see which root the tract/point leads to.
Transillumination
Transillumination with a fibre-optic light can be useful in the diagnosis of cracks in teeth.
Periodontal probing
Detailed periodontal probing around suspect teeth may reveal a sulcus within normal limits. However, on occasions, deeper pocketing will be noted. A narrow defect may be an indication of a root fracture or an endodontic lesion draining through the gingival crevice. Broader-based lesions are usually an indication of disease of periodontal origin.
Radiographs
Radiographs should be taken using film holders and a paralleling technique and be viewed using an appropriate viewer with magnification as necessary. They will not show early signs of pulpitis as there is no periodontal widening at this stage of pulpal degeneration. Radiographs may provide much important information to help to confirm a diagnosis, but they should not be used alone. Radiographic findings may include the loss of lamina dura (laterally or apically) or a frank periradicular radiolucency indicative of pulp necrosis. Alternatively, radiographs may show pulp chamber or root canal calcification, which may explain reduced responses to pulp sensitivity testing. This emphasises the need for considering using more than one test. More rarely, radiographic examination may reveal tooth/root resorptive defects.
Checklist for radiographic assessment
All the following can be assessed:
• caries
• proximity of restorations to pulp chamber
• quality of restorations, including coronal seal
• the size of the pulp chamber ± calcifications
• root end proximity to important structures
• presence of lesions of endodontic origin periradicularly or furcally
Test cavity
Occasionally, as a last resort, an access cavity is cut into dentine without local anaesthesia as an additional way of sensitivity testing.
Selective anaesthesia
Selective anaesthesia can be useful in cases of referred pain to distinguish whether the source of pain is mandibular or maxillary in origin. It is less useful for distinguishing pain from adjacent teeth, as the anaesthetic solution may diffuse laterally.
Diagnosis
Following this systematic approach to history taking and the application of appropriate special tests, it will usually be possible to make a diagnosis of the pulpal or periradicular problems. Such diagnoses are covered in Section 2.1 and include reversible pulpitis, irreversible pulpitis, pulp necrosis, resorptive changes, acute apical periodontitis, chronic apical periodontitis and acute and chronic apical abscesses.
After taking a thorough history and performing appropriate special tests, the clinician may be unsure as to whether the pain is of dental origin. Endodontic treatment should not be performed on an ad hoc or ‘hit and miss’ basis. In cases of difficult diagnosis, a referral to an orofacial pain clinic, a neurosurgeon or an ear, nose and throat specialist may be considered.
Cracked tooth syndrome
Cracked teeth appear to be an increasing clinical problem. Cracks may not be visible initially and the use of a piece of rubber dam between the teeth may aid diagnosis. A plastic bite stick (tooth sleuth) has been introduced to allow each cusp tip to be checked in turn; typically, the pain occurs on release of biting pressure. Small cracks may be treatable, although communications through the floor of the pulp chamber usually result in tooth loss.
Case selection and treatment
Once a diagnosis has been reached, a plan needs to be formulated as to how to deal with the problem. The fact that an endodontic procedure is feasible is not sufficient justification for performing it. Endodontic treatment must be considered as part of an overall treatment plan in such a way that it represents the patient’s best interests and wishes. The past dental history will have provided much information as to the patient’s attitude towards treatment. Good endodontic treatment takes time, requiring a commitment from both clinician and patient.
Treatment planning
Sequencing of treatment involves the management of pulpal or periodontal pain as a priority, and the extraction of unsaveable teeth. Large carious lesions should be stabilised and a preventive regimen including periodontal therapy instituted. Endodontic and restorative procedures can then be performed in a healthier environment and more predictable results can be obtained.
Indications for root canal therapy
Pulpal and periradicular disease
The most common indication for root canal therapy is pulpal or periradicular pathology. Elective root canal therapy may be performed for endodontic reasons: for example, teeth for which extensive restorative dentistry is planned and the subsequent tooth preparation would further stress a pulp of dubious prognosis. Alternatively, radiographs may show progressive calcification of the pulp space. This itself is not an indication for root canal therapy. However, such treatment may be performed if it is thought likely the pulp space will be required for restorative purposes.
Restorative requirements
Occasionally, it may be decided to root treat a tooth electively for restorative reasons. Such situations include teeth that have fractured at the gingival level and for which post space is required for their restoration, and teeth that are going to be used as overdenture abutments.
Periodontal disease
If the periodontal lesion is of primary endodontic origin then reattachment will usually occur provided the lesion has not been longstanding. If resolution is only partial, then periodontal therapy will be required if a successful result is to be obtained. In cases of advanced periodontal disease, one or more roots may require resection after root canal therapy (Ch. 1).
Reroot treatment
Reroot treatment is an increasing clinical problem and is considered in detail in Section 2.7.
Contraindications to treatment
General factors
The patient’s medical history or general wellbeing may preclude treatment. Lack of patient interest or restricted opening may preclude endodontic treatment. Access to posterior teeth may be difficult, with a minimum of two fingers opening being required. Remember that any degree of opening may reduce as the patient’s jaw muscles become fatigued.
Restorative factors
The clinical examination may have revealed the tooth to be unrestorable, to be of little functional use or to have a hopeless periodontal prognosis. Such situations preclude root canal therapy. Other forms of pathology may be present, such as extensive internal or external resorption. Although internal resorption will cease once the pulp is removed, consideration must be made as to the strength of the remaining root in function.
Trauma
Root fractures may be present either horizontally or vertically. Horizontal root fractures in the middle to apical third can have quite a good prognosis as the apical segment frequently remains vital with root canal therapy only being necessary to the fracture line. Fractures involving the gingival crevice, however, rapidly become infected as there is a continuation of the fracture line and the periodontal space. This includes vertical root fractures and many oblique fractures resulting from trauma.
Complex internal or external anatomy
Other contraindications include anatomy that is too complex to treat. Such variations may be internal (dens in dente) or external (root grooves). Palatal root grooves on upper incisors have a poor prognosis, as again there is a continuum along the root side that, like a root fracture, cannot be adequately cleaned and represents a constant nidus of infection.
2.3 Root canal morphology
Radiographs give some idea of basic root canal anatomy, although the reality is far more complex. Studies of cleared extracted teeth have shown that all roots enclose at least one root canal system, which frequently consists of a network of branches. Communications with the periodontal ligament also exist either in the furcation (furcal canals) or laterally (lateral canals). In addition, the root canal may frequently terminate as more than one opening with an array of accessory canals forming an apical delta. These furcal, lateral and apical communications have been termed ‘portals of exit’ from the root canal system. Furcal, lateral and accessory canals are created during tooth formation either when there is a break in the sheath of Hertwig or the sheath grows around an existing blood vessel. On occasions, such canals can be as large as the apical constriction. Their significance is not fully understood; however, it would seem sensible to use a preparation technique that aims to clean as much of the root canal system as possible.
The pulp chamber and root canal orifices may be reduced in size as a result of the deposition of secondary and tertiary dentine. If the irritation is severe with extensive destruction of pulpal cells, then further inflammatory changes involving the rest of the pulp will take place and could lead to pulp necrosis. Such pulpal degeneration starts coronally and progresses apically. Necrotic pulpal breakdown products may leach out of the root canal system to form lesions of endodontic origin around the portals of exit. Frequently, these changes in the periodontium will be visible lateral to the root before they are apparent apically. It is, therefore, extremely important to examine roots periradicularly as opposed to periapically as such examination may provide an early indication of pulp degeneration.
Important general considerations of pulpal anatomy
Shape
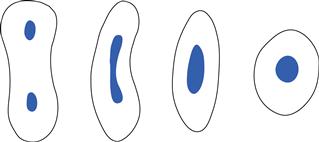
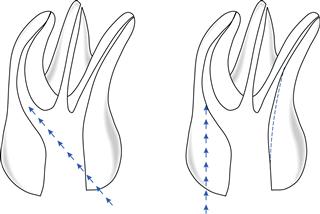
The shape of the coronal pulp and the outline of the canals is a reflection of the outline of the crown and root surfaces (Fig. 2.1).
Pulp morphology
This alters with age, irritants, attrition, caries, abrasion and periodontal disease.
Root anatomy
Over 90% of roots are curved. The only roots that rarely, if ever, contain two canals are maxillary anteriors, maxillary premolars with two roots and the distobuccal and palatal roots of maxillary molars. All other (note this includes all mandibular) roots may contain two canals.
Apical anatomy changes with age
The apical constriction is variable and usually cannot be detected by tactile sense, especially early in preparation, as dentine laid down in the coronal third of root canals will frequently cause files to bind coronally before they reach the apical third of the root canal.
Planes of curvature
Radiographs from a labial/buccal projection show only two planes of curvature. Many curvatures are towards or away from the film.
Access
Access to the root canal system involves both coronal access to the pulp chamber and radicular access to the root canals.
Coronal access
The coronal access preparation in root canal therapy serves several important functions:
• It provides an unimpeded path to the root canal system.
• It eliminates the pulp chamber roof in its entirety.
• It has divergent walls to support a temporary dressing between visits.
The ideal access cavity will achieve the above objectives but will preserve as much sound coronal and radicular tissue as possible. Occasionally, however, it may be necessary to enlarge and deflect the access to enhance the preparation of roots that are especially curved in their coronal thirds. In these situations, access preparation is dynamic, developing as instrumentation progresses.
Radicular access
The principle of straight-line radicular access cannot be overemphasised as it allows instruments to flow down the cavity line angles into the apical third of the root canal system without interruption and provides maximum tactile feedback while instrumenting the most delicate apical portion of the root canal. Adequate straight-line access reduces the angle of curvature in the coronal third of the root canal where it exits from the floor of the pulp chamber and thus reduces the overall canal curvature. Further advantages are discussed later.
Access to the root canal system is aided by examination of:
• tooth position and angulation
• the preoperative radiograph (or preferably more than one taken at different angles).
Examination of the tooth will provide guidance as to the position, size and angulation of the access cavity as many teeth are tilted in one or more planes relative to the arch and adjacent teeth.
Examination of the radiograph affords information on:
Endodontic access openings
Incisor and canine teeth
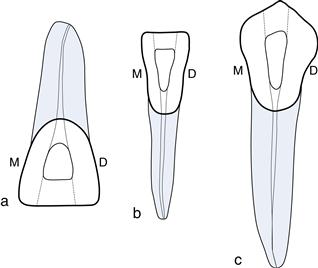
The access cavities for maxillary central and lateral incisors are similar and generally triangular in shape (Fig. 2.2). Access cavities for maxillary and mandibular canines are almost identical and more ovoid in shape (Fig. 2.3). Access for mandibular central and lateral incisors are triangular in shape and a second canal may be present in 40%. In general, extend the access in anterior teeth towards the incisal edge and under the cingulum (Fig. 2.2).
Premolar teeth
The maxillary first premolar in most individuals contains two canals and is extended more buccolingually than in single-rooted premolars. Approximately 5% may have a third root/canal placed buccally. In such situations, the access will be triangular in outline with the base towards the buccal side (Fig. 2.3).
The maxillary second premolar and both the mandibular first and second premolars usually have one centrally located root canal. However, if the canal appears to be situated under either the buccal or lingual cusp, look carefully for a second canal under the opposite cusp. The opening is a narrow oval shape. The maxillary second premolar access is centred over the central groove. Access for mandibular premolars is buccal to the central groove (Fig. 2.3).
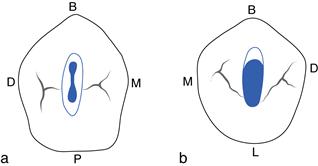
Maxillary molars
The maxillary molar access is generally triangular in shape with the base to the buccal and the apex to the palatal. Usually, one palatal and two buccal canals are identified. However, two canals may be present in the mesiobuccal root in 90% of cases with approximately half ending in two foramina (Fig. 2.4).
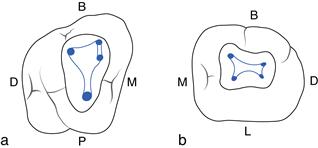
Mandibular molars
The mandibular molar access is more trapezoid in shape with its base to the mesial and apex to the distal. They usually have two roots with two canals in the mesial root and one in the distal root. There is a possibility of a second canal in the distal root (33%) (Fig. 2.4).
Access: prior considerations
A number of steps should be taken to prepare for access (Box 2.1).
Rubber dam
The rubber dam is essential for root canal treatment and affords the following advantages:
On occasions, it may be deemed appropriate to initiate access prior to placement of rubber dam as this allows better appreciation of external root contour and tooth position. The rubber dam should be placed as soon as the pulp chamber is identified for the above reasons.
Access technique
Box 2.2 describes the technique used to achieve access.
2.4 Root canal preparation
Any root canal preparation technique should be simple, safe and predictable. Many techniques have been described over the years. In principle, these can be split into methods of instrument manipulation (reaming and filing) and preparation philosophies, the most recent one being a crown-down approach with apical preparation being developed throughout the procedure and completed at the end. New developments extend or facilitate the process.
Reaming infers rotating the root canal instrument clockwise, this motion draws the instrument into the canal and cuts dentine. Filing infers a linear motion of the instrument in a push–pull manner. Filing may be performed around the perimeter of a root canal especially if it is oval or dumbell shaped; such instrument manipulation is termed circumferential filing.
Root canal preparation has both biological and mechanical objectives. The biological objectives are to eliminate the pulp, bacteria and related irritants from the root canal system. The mechanical objectives are directed at producing a continuously tapering preparation with the original anatomy and foramen position maintained. The apical foramen should also be kept as small as practical.
In summary, the aim of root canal preparation is to debride the pulp space, rendering it as bacteria free as possible, producing a shape amenable to irrigation and obturation. This apparently straightforward task is complicated by the anatomy of root canal systems, which is complex and makes cleaning them in their entirety a clinical challenge.
Current trends in canal preparation
Current thinking on canal preparation emphasises the development of shape in a crown-down manner removing infected dentine as it is encountered. Further cleaning of the canal is provided by correct choice and use of root canal irrigants (in particular, sodium hypochlorite because of its antimicrobial and tissue-dissolving properties), with the combination being termed chemomechanical debridement.
Instrument manipulation
The two most commonly used motions are watchwinding and balanced force.
Watchwinding refers to the gentle side-to-side rotation of a file (30° each way). This motion is useful for all stages of canal preparation, especially initial negotiation and finishing the apical third.
Balanced forces (in many ways a development from watchwinding) involves rotating the instrument 60° clockwise to set the flutes and then rotating it 120° anticlockwise while maintaining apical pressure sufficient to resist coronal movement of the file. Balanced forces is an efficient cutting motion and has been shown to maintain a central canal position even round moderate curvatures while allowing a larger size to be prepared apically (compared with other hand instrumentation techniques).
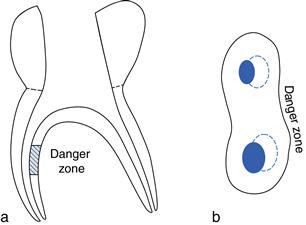
Coronal interferences influence the forces a file will exert within a canal. This is of particular importance in curved canals where files may prepare more dentine along the furcal (danger zone) as opposed to the outer canal wall. It is important to be aware of this, to limit the size of enlargement in curved canals and direct files away from the furcal wall to avoid a strip perforation (Fig. 2.6).
Irrigation
Irrigating solutions are usually delivered using a syringe with a 27- or 28-gauge needle. Care should be taken to ensure that the needle does not bind in the canal and that irrigating solution does not pass into periapical tissues. The role of the irrigant is to remove debris and provide lubrication for instruments. Specifically, an irrigant such as sodium hypochlorite will dissolve organic remnants and, most importantly, also has an antibacterial action. It may be used in a range of concentrations (0.5–5.25%), with 2.5% being popular. It is important that the irrigant is changed frequently; ideally irrigation should be performed between each file, at least every two to three files being the minimum. If removal of the smear layer is desired, then an irrigation solution containing ethylenediamine tetra-acetic acid (EDTA) should be used. There is no clinical consensus as to whether or not the smear layer should be removed although there is a suggestion that its use may have a positive effect on the outcome of retreatment cases.
A most effective way of delivering irrigating solutions is through an ultrasonic handpiece. Ultrasonic agitation (acoustic microstreaming) has been shown to be effective at removing debris from canals.
Canal preparation
Several methods of canal preparation exist. The method described here encompasses current thought:
Canal exploration
Root canals are infinitely variable in their shapes and sizes. Larger canals allow easy placement of instruments and irrigating solutions whereas smaller ones require pre-enlargement coronally prior to the canal exploration. Preliminary assessment of the canal can be made with the smallest and most flexible instruments. It is unlikely that the operator will be able to determine the working length initially as files may be binding coronally.
Pre-enlargement and straight-line radicular access
Pre-enlargement is achieved by watchwinding file sizes 10–35 in series, gradually opening up narrow canal orifices to a size sufficient to take a Gates–Glidden bur. The pre-enlargement can then be developed further to produce straight-line radicular access taking care to work the bur away from furcal regions of roots. A file should stand upright in the tooth and pass undeflected deep into the canal once adequate straight-line radicular access has been achieved.
Gates–Glidden burs may be used to relocate a canal away from the danger zone; however, care should be taken to avoid overenlargement. Gates–Glidden Nos 6 and 5 should only be used on the walls of the access cavity, and No. 4 no deeper than the canal orifice. The No. 3 may be used to the mid-canal region and the No. 2 to the beginning of the canal curvature, or to near full length in a straight canal. The No. 1 is quite fragile, but may be used at ultraslow speeds provided it is loose in the canal.
Advantages of pre-enlargement and establishment of straight-line access
There are a number of advantages from achieving straight-line access:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses