2
Diagnosis: Chief Complaint and Problem List
Introduction
Work-up of a problem list – the interview – chief complaint
General health
Clinical examination
Extraoral examination
Extraoral photographs
Function of the masticatory system
Intraoral analysis – oral health
Evaluation of dental casts – arch form
Occlusal analysis
Space analysis
Cephalometric analysis
Final problem list
Indication for treatment
The presentation of the problem list – the tip of the iceberg
Concluding remarks
References
Introduction
The patient’s chief complaint when first encountering the orthodontist is often far from the objective problem list envisioned by the clinician. In a recent comment Bowman (2005) asked: Have you ever had a patient asking ‘Can you just fix this tooth that is crooked?’ (Fig. 2.1). Or they ask: ‘Do you have to put braces on all my teeth?’ Independent of the reason for the consultation, treatment options can only be discussed following the work-up of a comprehensive problem list (Table 2.1).
Table 2.1 Chief complaint – ‘My upper front tooth is sticking out and catching my lower lip. It is getting worse’
| Problem list | Solution |
| Extraoral examination | |
| Straight profile with a lip trap related to the upper right lateral incisor | Alignment of the lateral incisors following distalization of 23 and 24 |
| Functional analysis | |
| Traumatic occlusion on the incisors. The mandible forced back to a deep bite with impingement Muscle tenderness |
Intrusion of upper incisors and proclination of lower incisors for reduction of the overbite. Coordination between structural position and intercuspation |
| Intraoral analysis | |
| Missing teeth 17, 27 | Have to be accepted |
| Total periodontitis 16, 15 | Extraction 16, 15 |
| Gingival dehiscence generally | Motivation and oral hygiene instruction |
| Irregular position and crowding of upper and lower front teeth | Distalization of 14, 13, 12 |
| Proclination and distal rotation 22 | Retroclination of 22 and proclination 12, 11, 21 |
| Distal canine relationship right side | Retraction of 14, 13 |
| Deep bite with impingement | Levelling and intrusion of upper and lower incisors |
Fig. 2.1 (1,2) This patient was referred from the general dentist to the orthodontist for correction of flaring of the upper right lateral incisor. It is obvious that the flared incisor cannot be corrected without taking into consideration other problems such as the crowding and the deep bite.

Orthodontists generally perceive the problem list as the diagnosis. Whereas a diagnosis within other areas of medicine include information regarding aetiology, pathogenesis and prognosis, this is not the case within orthodontics, as the signs and symptoms related to a specific malocclusion can have a large variety of causes. For example, increased overjet may be a sign of a skeletal discrepancy (maxillary prognathism or mandibular retrognathism) or a dentoalveolar condition. All of these can contribute to an increase in overjet. A problem list in contrast, is the compilation of positive findings obtained from the interview, the clinical examination and the analysis of the diagnostic records.
Work-Up of a Problem List – the Interview – Chief Complaint
Before compiling the problem list, the patient should be allowed to express in his or her words, their problem and the stimulus or motivating factor that led to the consultation. Letting patients express themselves freely allows the orthodontist to get a better impression of the priority that the patient gives to their problem. Proffit and Ackerman (2000) recommended the use of a questionnaire for a parent accompanying a child to the orthodontist. In the case of an adult patient, a personal interview prompted by a few open-ended questions is preferable to a standard questionnaire. The way in which a patient explains their problem gives an indication of whether poor dental aesthetics or function ranks higher in their perception of the problem. The orthodontist should not try to influence the patient during this part of the interview.
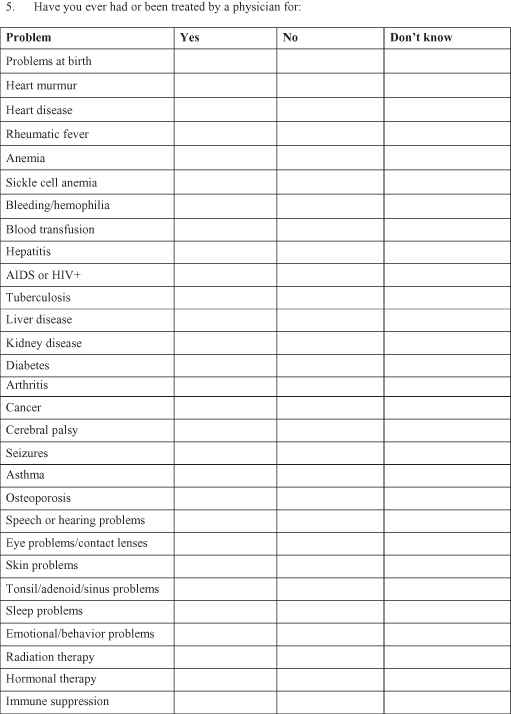
In the case where the malocclusion is described as developing over time, it is advisable to ask the patient to bring in an earlier photograph from which the smile can be evaluated. The gradually occurring changes demonstrated by means of the photographs can then be used while explaining the development of the malocclusion and when discussing the consequences of no intervention with the patient (Fig. 2.2).
Fig. 2.2 (1–5) A patient with a major need for occlusal rehabilitation presented with this series of family photographs that clearly illustrated the gradual deterioration of his dentition. The patient had seen a family dentist regularly but only at the last visit was he referred for an orthodontic consultation.
If the patient is referred by a general dentist or a colleague within another discipline, it would be important to know the attitude of the referring dentist to orthodontics. How has the dentist presented the problem to the patient? Why was the patient not referred before? Has the family dentist made any comments? Does the family have a ‘new’ dentist? If yes, why did the patient look for a new dentist?
Once patients have expressed their perceived problems, the orthodontist can start gathering the information required to propose a solution to the problem.
General Health
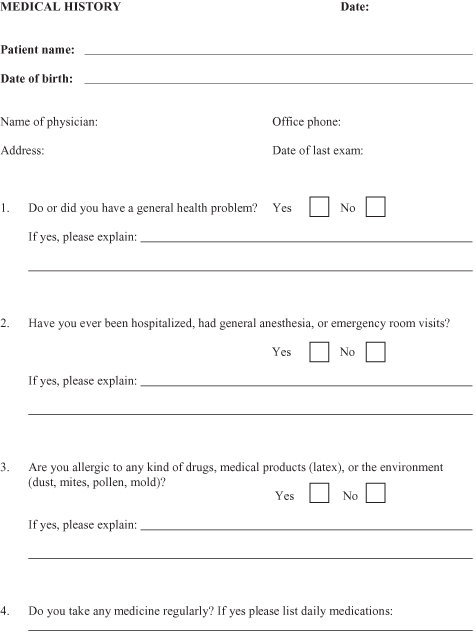
Changes occurring in the occlusion may reflect general health. A thorough medical history is therefore needed both for the clarification of the aetiology and for prediction of the tissue reaction to the orthodontics. Patients may think that their general health problems are irrelevant to their dental problems but information about previous diseases, e.g. juvenile idiopathic arthritis or trauma to either soft or hard tissues could contribute to clarification of the aetiology. Metabolic diseases and chronic medication may also have an influence. In this context a medical health questionnaire is useful as the repeated questions may seem trivial when asked verbally (Fig. 2.3).
Risk factors for periodontitis have been the subject of numerous studies and a multi-factorial aetiology is generally accepted (Papapanou 1999; Van Dyke and Sheilesh 2005). The role of systemic conditions and disorders in periodontal disease was discussed by Genco and Loe (1993) in a comprehensive review, focusing particularly on the impact of diabetes and smoking. The mechanism by which diabetes contribute to the periodontal breakdown was discussed by Lalla et al. (2000) and according to Taylor et al. (1998a,b), who compared people with diabetes and healthy individuals, the odds ratio for progression of bone loss in the case of diabetes was 4.2.
Smoking is the other risk factor that routinely stands out when performing analysis of risk factors related to periodontal disease. A meta-analysis concluded that the odds ratio for developing periodontal disease is increased by smoking to 2.82 with a 95% confidence limit of 2.36 to 3.39 (Papapanou and Lindhe 2003). The causal effect of smoking is not known. It may be indirect, as smokers are generally more slender than their counterparts therefore have lower bone density; smokers also in general have poorer oral hygiene than their non-smoker counterparts. On the other hand, it may also be a direct effect of the toxicity of tobacco smoke (Johnston 1994).
Other systemic risk factors include diseases or medications influencing the immune system, such as human immunodeficiency virus (HIV) infection and medications that lead to suppression of the immune system.
Clinical Examination
The clinical examination includes extraoral examination, evaluation of the function of the masticatory system and intraoral examination and should be supplemented with findings from a review of photographs, dental casts and radiographs.
When listing the results of the examination, only positive findings should be listed and these should always appear in the same order (Box 2.1).
Box 2.1 Clinical examination
Extraoral
- En face
- Smile – lip line
- Profile
- Lips
- Midlines: nose; maxillary dental; mandibular dental; chin
Oral function
- Opening path
- Maximum opening
- Lateral movements
- Temporomandibular joints (TMJs)
- Muscles of mastication
- Tongue function
- Lip catch
- Mode of respiration
- Mode of swallowing
Intraoral
- Mucosa
- Dental status
Missing teeth
Morphological anomalies
Restorations
Attrition
Periodontal status
- Pathological pockets
- Recessions
Dental casts
- Positional anomalies – tipping – rotation
- Occlusion – sagittal, vertical, transverse
Space analysis
- Maxilla
- Mandible
Arch shape
- Maxilla
- Mandible
Cephalometric analysis
Extraoral Examination
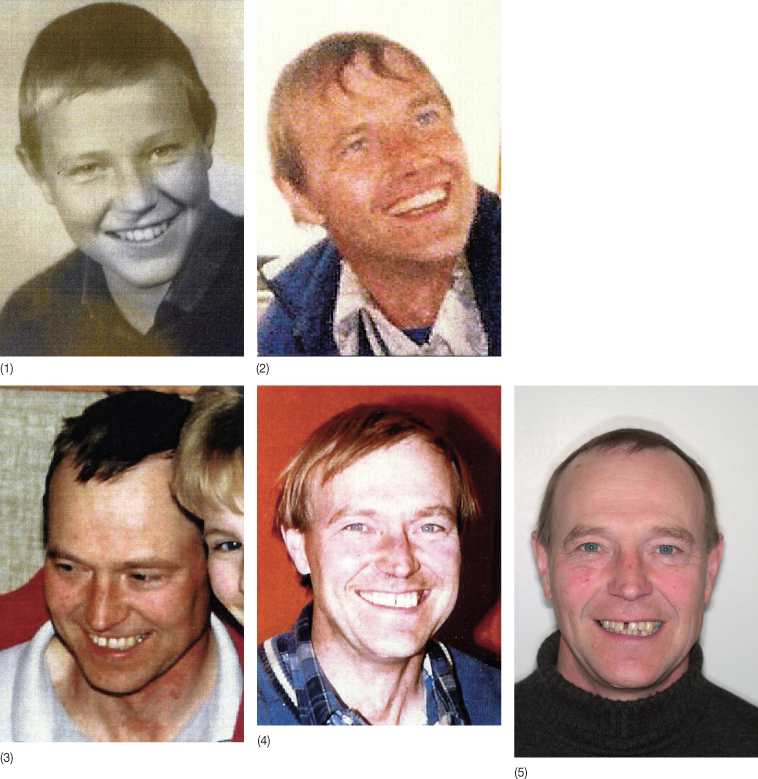
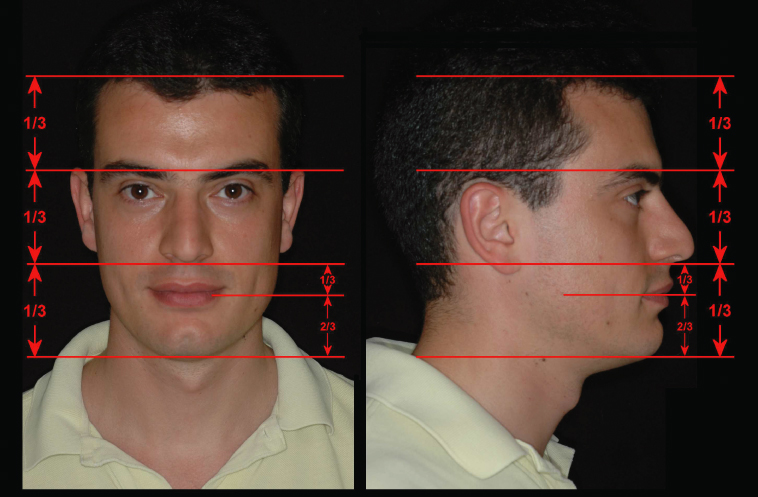
The face is first observed from the frontal view and apparent asymmetries noted. The relative widths of the eyes, the nose and the mouth are assessed and major deviations noted (Fig. 2.4). The inter-inner-canthal distance in a harmonious face corresponds to the width of the nose, whereas the inter-iris width is equal to the width of the mouth (Fig. 2.4). The vertical proportions can be measured both on the frontal and on the profile views. The division of the face into thirds has been accepted as a desirable norm for white Caucasians (Fig. 2.5).
Fig. 2.4 Frontal view of a patient fulfilling the criteria of harmony. The inter-inner-canthal distance corresponds to the width of the nose. The symmetry of the face can be evaluated by drawing vertical lines through the medial and lateral aspects of the eyes.
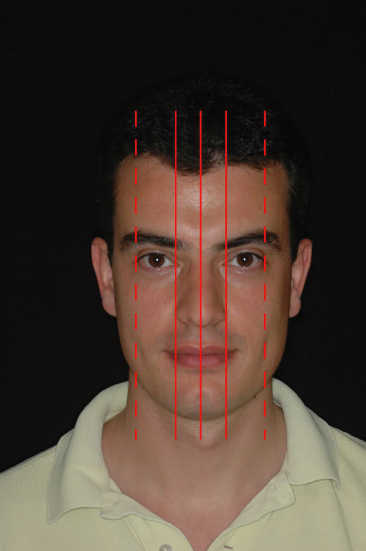
Fig. 2.5 Vertical proportion of the face seen en face and in profile view. The proportions indicated are the ideal values for white Caucasians.
Exact measurements are of little value. ‘Beauty is in the eye of the beholder’ and the results of such analysis are partially subjective and can only act as a guide. Sagittally, a face can, based on white Caucasian norms, be characterized as convex, straight or concave (Fig. 2.6). An impression of the mandibular inclination can be obtained by holding a straight instrument along the border of the mandible (Fig. 2.7). Anthropometric measurements that have been published for different ethnic groups are characterized by large standard deviations and low reproducibility (Farkas and Kolar 1987; Farkas 1994) and many of our patients cannot be classified as belonging to one race only.
Fig. 2.6 Profiles representing different skeletal patterns. The convex profile (1) typically presents with a Class II malocclusion whereas the concave profile (3) would be seen in a patient with a Class III malocclusion. In both cases the deviation may be in either the position of the maxilla or in the position of the mandible. The straight profile (2) may likewise be due to bimaxillary retrusion or protrusion.
(From Proffit and Ackerman (2000). Reproduced with permission from Elsevier.)
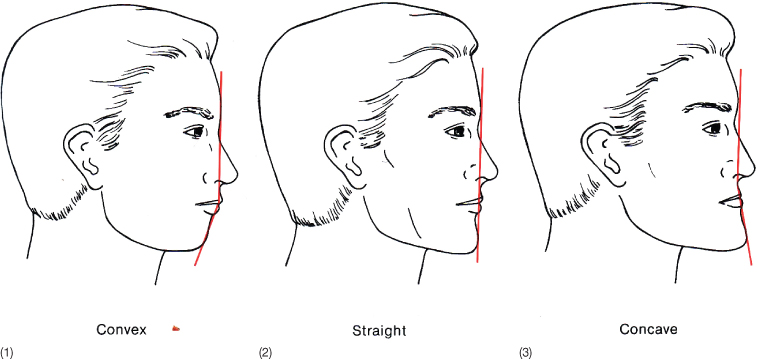
Fig. 2.7 Assessment of mandibular inclination.

Most soft tissue analyzes have focused on the two-dimensional profile and frontal images, but although both hard and soft tissues can now be analyzed three dimensionally, two-dimensional images still dominate our diagnostic routine (Arnett and Bergman 1993a,b).
Extraoral Photographs
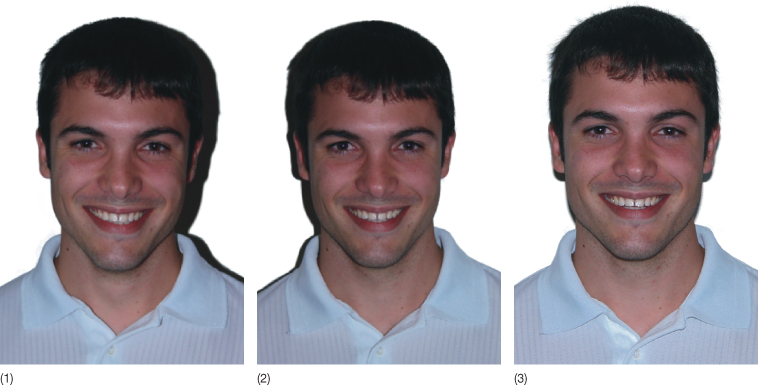
As the evaluation of the extraoral appearance has an increasing role in treatment planning, it is of paramount importance that photographs are taken in a way that they provide a valid record. The relative position of patient, photographer and source of illumination should be taken into consideration. The ideal distance from the lens to the patient is 100 cm. With shorter distance, the image will be distorted (Fig. 2.8). The facial photographs should include the neck and a part of the thorax. The background should be of a uniform colour, preferably light; however, some orthodontists prefer a blue or a black background as it gives fewer problems with shadows. The patient should be upright with the lips in a relaxed position. In the case of insufficient lip closure a photograph should also be taken with the lip strain necessary to obtain closure. The ears should be uncovered.
Fig. 2.8 (1) The lens focal distance for the extraoral images should be 1–1.5 m. (2) Frontal image taken with shorter lens focal distance leading to severe distortion.

Vertically, the centre of the camera should be at the level of the Frankfort horizontal plane, in the midsagittal plane of the patient.
For the en face views the patient should look at the superior part of the lens of the camera. A camera above or below this level will result in a distortion of the face (Fig. 2.9). The light from the flash should be above the top of the object (at 12 o’clock) in order to get the correct distribution of shadows (Fig. 2.10).
Fig. 2.9 Influence of the photographic technique on the extraoral image taken: (1) with the lens 10 cm above the height of the eyes of the patient, (2) at correct height, and (3) 10 cm too low.

Fig. 2.10 (1–3) Different distributions of the shadows caused by different positions of the flash.
On the profile images, the patient looks straight ahead, but turning the head just enough to see the eyelashes of the other side often gives a better impression of the profile (Fig. 2.11). The illumination has to be oblique from the front with the flash turned towards the nares. This concentrates the shadows behind the head. Light from above produces shadows below the head (Fig. 2.12) and light from below will result in shadows above. Lateral illumination will lead to a shadow below the face and a pronounced nasolabial line (Fig. 2.13). Thus incorrect illumination results in unsatisfactory images.