CHAPTER 19 TEETH IN A DAY AND TEETH IN AN HOUR
IMPLANT PROTOCOLS FOR IMMEDIATE FUNCTION AND AESTHETICS
 A Brief Examination of Osseointegration
A Brief Examination of Osseointegration
Osseointegration may be defined broadly as the dynamic interaction of vital bone with the surface of a biocompatible implant in the absence of an interposing fibrous connective tissue layer.1–2 Without successful osseointegration at the bone-implant interface, endosseous implants invariably fail.
In 1985 Brånemark described the potential causes of failure of bone-to-implant integration: “In unsuccessful cases nonmineralized connective tissue, constituting a kind of pseudoarthrosis, forms in the border zone at the implant. This development can be initiated by excessive preparation trauma, infection, loading too early in the healing period before adequate mineralization and organization of hard tissue has taken place, or supraluminal loading at any time, even many years after integration has been established. Once lost, osseointegration cannot be reconsistitued.”1
Critical to Brånemark’s original protocol was an initial period during which implant fixtures remained submerged and out of function in order to eliminate implant micromovement, a process likely to lead to fibrous tissue encapsulation rather than true bone-to-implant contact.1 To a large degree, Brånemark’s original delayed protocol is still followed by many clinicians. In addition, Brånemark’s second-stage protocol (implant exposure and abutment connection) also called for a delay in prosthetic loading until soft tissue healing was complete around the newly installed transmucosal abutments.
 Immediate Loading: What the Evidence Says
Immediate Loading: What the Evidence Says
The viability of immediately loading endosseous implants has been an area of considerable interest to dental researchers for many years. In 1990, Schnitman et al. placed multiple Brånemark implants between the mandibular mental foramina and two additional implants distal to the foramina.3 The two distally positioned implants and one anterior implant were placed into immediate function through attachment to a fixed-detachable prosthesis. According to the investigators, this treatment protocol was successfully applied to seven patients without any adverse effects on long-term implant therapy. In 1997 these same investigators published 10-year results for Brånemark implants immediately loaded in the mandible with fixed prostheses at implant placement.4 In this latter study, a total of 63 Brånemark 3.75-mm implants of various lengths were placed, 28 of which were immediately loaded, providing support for fixed provisional restorations. Thirty-five adjacent implants were submerged for a 3-month period. Of the 28 immediately loaded implants, 4 eventually failed and 100% of the standard two-stage protocol fixtures osseointegrated. The 10-year survival rate for the immediately loaded implants was 84.7% and 100% for the submerged implants.
In 1997 Balshi and Wolfinger published a preliminary report examining immediate loading of Brånemark implants placed in 10 patients with edentulous mandibles.5 One hundred thirty implants were placed, with a minimum of 10 implants in each mandible. In each patient, abutments were connected to 4 implants immediately after insertion, 2 between the mental foramina and 2 distally. The remaining implants remained submerged for 3 months. The 4 implants with abutment connections were immediately loaded with all-acrylic resin-fixed prostheses (“conversion” prostheses).6 Seven to 10 days later the conversion prostheses were temporarily removed for suture removal and final plaster impressions. At 6 weeks, metal frameworks replaced the all-acrylic conversion prostheses because it was thought that the metal-reinforced prostheses would provide superior distribution load to the implant fixtures. At second-stage surgery, all 10 patients experienced a prosthesis survival rate of 100%. Thirty-two of the 40 immediately loaded implants were stable at second-stage surgery, yielding an 80% survival rate, versus a 98% survival rate for the unloaded implants at second-stage surgery.
In 2003 Balshi et al. published five-year results of their previously reported 1997 study, adding an additional 24 patients with edentulous mandibles treated with a simplified protocol for immediate loading.7 In the simplified protocol group, 144 implants were placed between 1997 and 2000. A mean of 6 implants were placed in each mandible in both healed and fresh extraction sites. Two significant changes in this modified protocol group were instituted: (1) An increasing number of implants were loaded immediately, using fewer overall implants per arch. All implants were loaded immediately for the last patients in this test group. (2) The all-acrylic resin conversion prostheses were not disturbed during the initial 3 months of treatment following implant placement.
The results of Balshi’s 2003 study proved instructive. All 10 of the original patients who reached second-stage surgery had a 100% prosthesis survival rate 5 years later. Two additional implants originally unloaded failed after second-stage surgery but no further immediately loaded implants within this original group failed at the 5-year follow-up. In the added simplified protocol group, no prosthesis failed. Of the immediately loaded implants in this group, 97% survived at the end of the first year. Unlike the initial group, there was no statistically significant difference between the immediately loaded and submerged implants in the simplified protocol (P =.423). In examining the data from this study, the authors suggest the following: (1) Undisturbed splinting of immediately loaded implants with an all-acrylic conversion prosthesis is critical during the initial 3-month healing period following implant placement to prevent unwanted implant micromotion at the bone-to-implant interface. (2) In vitro comparison of force distribution to the implants between the acrylic-resin versus metal-reinforced prostheses showed no differences, suggesting no reason to convert to a metal-reinforced material during critical early healing.7 (3) In immediately loaded implant full-arch reconstruction, implants placed in the characteristically dense bone between the mental foramina, with the potential for bicortical anchorage, exhibit an increased potential for long-term survival when compared to posterior positioned implants.
A number of studies have also examined the effect implant surface structure may have on implant survival rates of immediately loaded implants. In 2004 Rocci et al. compared immediately loaded TiUnite oxidized titanium implants (Nobel Biocare, Kloten, Switzerland) to machine-surfaced Brånemark System implants for posterior mandibular partial fixed bridges.8 After 1 year of prosthetic load, the cumulative success rate for the TiUnite fixtures was 95.5% versus 85.5% for the machine-surfaced implants, despite the fact that there were more smokers and more implants placed in type 4 bone in the TiUnite group. A second study by Glauser et al. examined long-term results of immediate loading of Brånemark System TiUnite implants placed mainly in soft bone.9 In this study, 102 Brånemark System Mk IV TiUnite implants (38 maxillary and 64 mandibular) were inserted primarily in posterior regions of the jaws and loaded at the time of implant insertion. At the end of 4 years of loading, 3 stable maxillary implants were removed at 8 weeks secondary to postoperative infection in the adjacent area that had a guided bone regenerative procedure. No other implants were lost, with a net cumulative implant success rate of 97.1% at 4 years. A third prospective study by Banden et al. examined 18-month results of 111 Brånemark System TiUnite implants placed into maxillary or mandibular posterior quadrants, areas known for low bone density.10 In this study, implants were splinted and placed into function within 9 but no longer than 16 days following implant insertion. Of the 111 implants, only 1 failed, yielding an overall survival rate of 99.1%. No prosthesis in this study failed. In each of these 3 studies, the combination of rigid splinting plus oxidized titanium fixture surfaces generated results equivalent to those seen in Brånemark’s traditional two-stage submerged protocol.
In 2005 Balshi et al. reported resonance frequency analysis (RFA) results of 164 maxillary and 112 mandibular implants immediately loaded and splinted according to a strictly defined treatment protocol termed “Teeth In A Day.”11 Resonance frequency analysis is a noninvasive technique in which mechanical vibration is used to record bone-implant stiffness parameters and hence is a measure of implant stability.12 RFA readings were obtained at implant insertion and on days 30, 60, and 90, time points considered crucial for successful initiation of osseointegration. In this study, RFA values consistently decreased in value through day 30, indicating intense bone remodeling. This initial decrease was followed by consistent increases in RFA values through day 60, suggestive of significant osteoblastic bone regenerative activity occurring at the implant-bone interface. At the end of 90 days, increased RFA values indicative of positive implant stability correlated strongly with 99.1% and 97.5% mean implant survival values in the mandible and maxilla, respectively. According to the authors, the Teeth In A Day protocol, calling for immediate cross-arch splinting of all inserted implants, allows for application of functional, evenly distributed loads, resulting in increased RFA values during critical early time periods.
 Teeth In A Day
Teeth In A Day
In 2005 Balshi et al. published a landmark prospective study of 55 consecutive cases examining maxillary immediate full-arch functional loading following their highly specific Teeth In A Day protocol.13 The study, which spanned a period between December 1999 and February 2004, examined 552 immediately loaded implants, with an average of 10 implants per maxilla. In each patient, the Teeth In A Day protocol dictated specific sequenced treatment procedures that were closely adhered to throughout this study. Of particular importance was the attachment of all implants immediately into a full-arch, second molar to second molar screw-retained all-acrylic fixed prosthesis, rigidly splinting all inserted implants to control occlusal loads during the initial 12-week healing period (Figure 19-1).
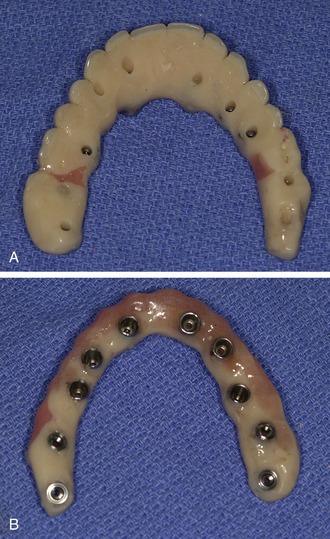
Figure 19-1. An all-acrylic conversion prosthesis containing stainless steel screw housings: underside (A) and palatal (B) views.
Initial Evaluation
A comprehensive initial examination and evaluation is the critical first step in the Teeth In A Day protocol. Prior to clinical examination, panoramic and full-mouth periapical radiographs are obtained for each patient (Figure 19-2, A).
Following assessment of the patient’s chief complaint and detailed review of the patient’s medical and dental histories, a thorough oral clinical examination is undertaken. In addition to assessing for any present pathology, a meticulous occlusal analysis is performed, including assessment of current vertical dimension, temporomandibular joint function, tooth arrangement, including midline shifts, spacing between teeth, and planes of occlusion. Appropriate jaw records are obtained and recorded. A detailed aesthetic examination is then undertaken, including assessments of facial symmetry from frontal and profile views, smile analysis, including lip anatomy as well as smile line level, tooth coloration and gingival tone and shade, and facial skin color and tone. Intraoral and full-face digital photographs are then taken from every angle for immediate review with the patient and for later study (Figure 19-2, B and C).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



