Material Considerations in the Fabrication of Prostheses for Completely Edentulous Patients
James A. Kelly and Thomas J. Salinas
Mayo Clinic College of Medicine, Rochester, Minnesota, USA
The scope of this chapter is to provide the reader with information related to material science in construction of implant prosthetics for patients with complete edentulism. The last decades have experienced a plethora of biomaterial and surgical sequencing developments, which have led to a modified approach in treating edentulous patients with dental implants. While evidence‐based information on this approach is not robust, some protocols with varying degrees of success will be reviewed for case application according to patient‐specific factors.
Origin of material selection for implant prostheses
The early decades preceding osseointegration had identified a challenge in meeting the need for treating patients with prostheses that were mucosally supported and retained.1 The edentulous patient demographic represented the greatest need to improve prosthesis support and retention. Using cast alloys and combining these with polymethylmethacrylate seemed to be the logical choice, as most removable dental prostheses were linked to fixed anchorage by precision or semi‐precision means. There seemed to be concerns about using base metals for this purpose as some galvanic potential2 was considered detrimental to health of the implant, so the use of noble alloys with a high elastic modulus likewise seemed logical. Knowing the cascade of events leading to osseointegration, it was also of concern that the implant–bone interface be protected from the impact of occlusal forces.3 The choice of using acrylic resin was intended to shield the bone interface from impact load.
The use of this design was published as being successful surgically and prosthodontically without the need for major prosthesis redesign.4 Even with additional experience of medium‐term success, results did not indicate that prosthesis redesign was a major factor in time to retreatment.5 Many other treatment centers that were conducting duplicate population studies seemed to find quite a high “survival” with what was being interpreted as synonymous implant and prosthesis survival.6,7 Survival of osseointegrated implants, even with first‐generation implant design, was quite predictable and it remains a reliable surgical technique. The reality is that surgical survival and prosthesis survival are quite different. As with other restorative interfaces, the servicing needs for materials that are chosen will be evident in some fashion. Goodacre et al.8 conducted a review of complications cited for these prostheses and identified the overdenture as requiring significant servicing needs. As literature accumulated, Purcell et al.,9 Gallucci et al.,10 and Dhima et al.11 all cited concerns with this type of design’s long‐term cost effectiveness. The problems encountered were fractured teeth, loosened screws, fractured screws, and failure of the veneering material in some form. Although some of the problems with implant components were addressed after a redesign, the balance of these complications seemed to happen on average 7–14 years after initial placement. The follow‐up requirement begged for an improvement of material performance, design testing, and improved space‐allocation techniques.
The advent of osseointegration has revolutionized the treatment of those who have acquired and congenital absence of teeth and associated maxillofacial structures. The treatment paradigm used for this demographic had historically been based upon unique factors of presentation. While many piloted centers had approached treatment of edentulous patients on a large scale, the demographics of these patients have changed considerably, with many patients keeping their teeth for a longer time.12,13
The oral conditions of patients who present with the affliction of decades‐old edentulism may differ considerably from those who present with a failing dentition (Figure 19.1). In these circumstances, it is imperative to understand spatial consideration with regard to diagnosis and treatment planning with specific prosthesis design. Treatment planning from both a surgical14,15 and prosthetic16 basis should be given due consideration as each will have specific requisites for successful outcomes.
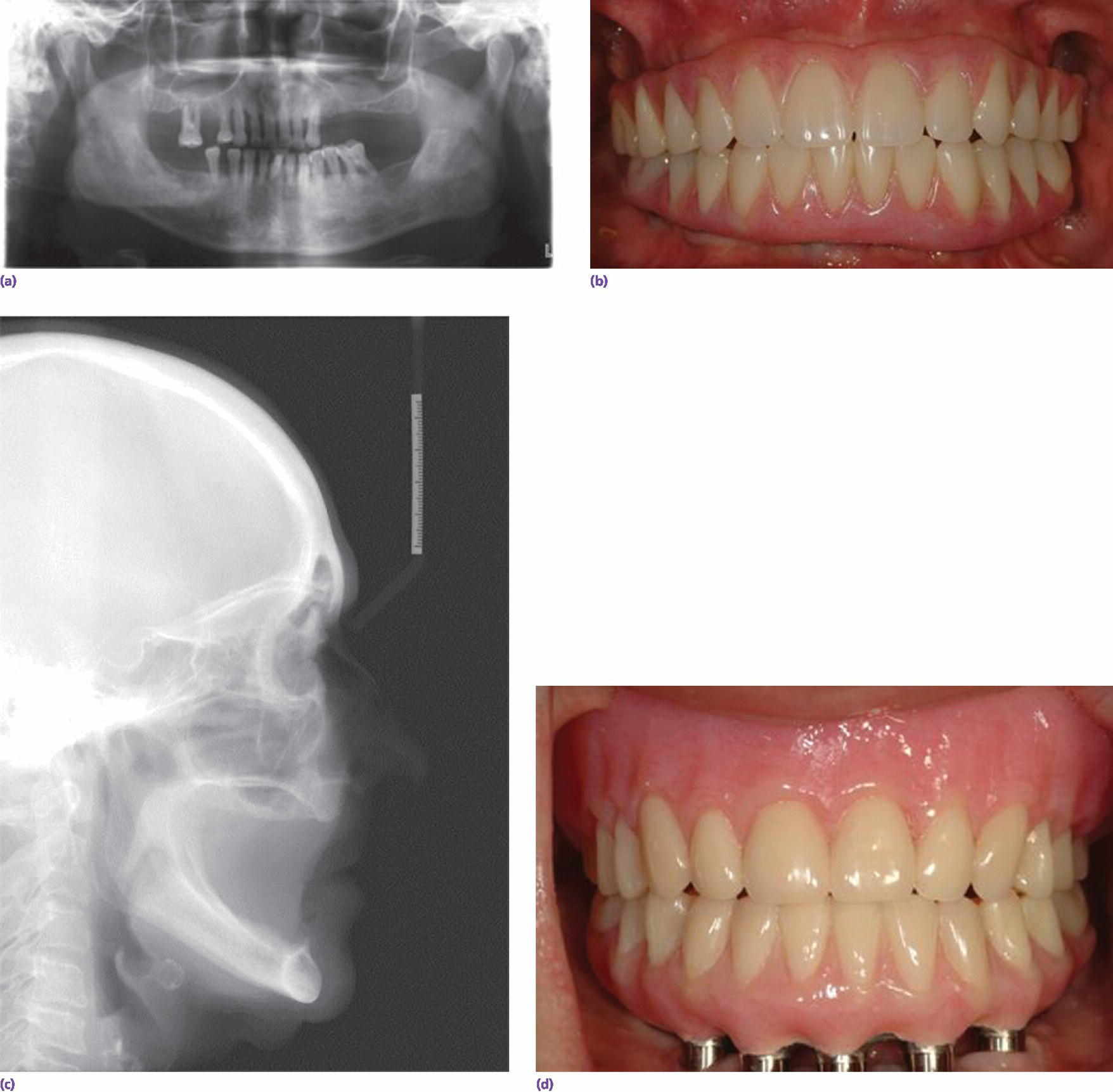
Figure 19.1 (a) Patient presenting for implant prosthetic reconstruction months prior to (b) definitive implant fixed reconstruction. (c) Patient presenting decades after tooth loss for (d) mandibular implant fixed reconstruction.
Initial evaluation and treatment planning
Patients presenting edentulous or in need of strategic edentulation should be evaluated for treatment goals and expectations.4,17 In some cases, patient expectations of treatment should be revisited to ascertain objectives, which may be nonachievable given their circumstances. Many instruments that evaluate expectations have been proposed for patient‐perceived outcomes with complete dentures.18–21 Although these instruments can give insight into behavioral ideals, they do not make provision for those who do not have appropriate perception of their edentulous state. In some cases, the use of the Diagnostic and Statistical Manual of Mental Disorders can assist with identification of body dysmorphic disorder or other similar perceptive deficits.22 If expectations are realistic and achievable, the initial treatment phase may be with conventional prosthetics or with provisional implant‐assisted prosthetics.
Facial form, orthognathic profile, and interocclusal distances will also give important information for gaining an understanding of the available restorative volume. Analog or digital analysis prior to extractions or implant placement is essential and will give the basis for sound treatment objectives (Figure 19.2). A further understanding of the patient’s concerns will direct proper planning to satisfy these requirements, be it fixed or removable prosthodontics.
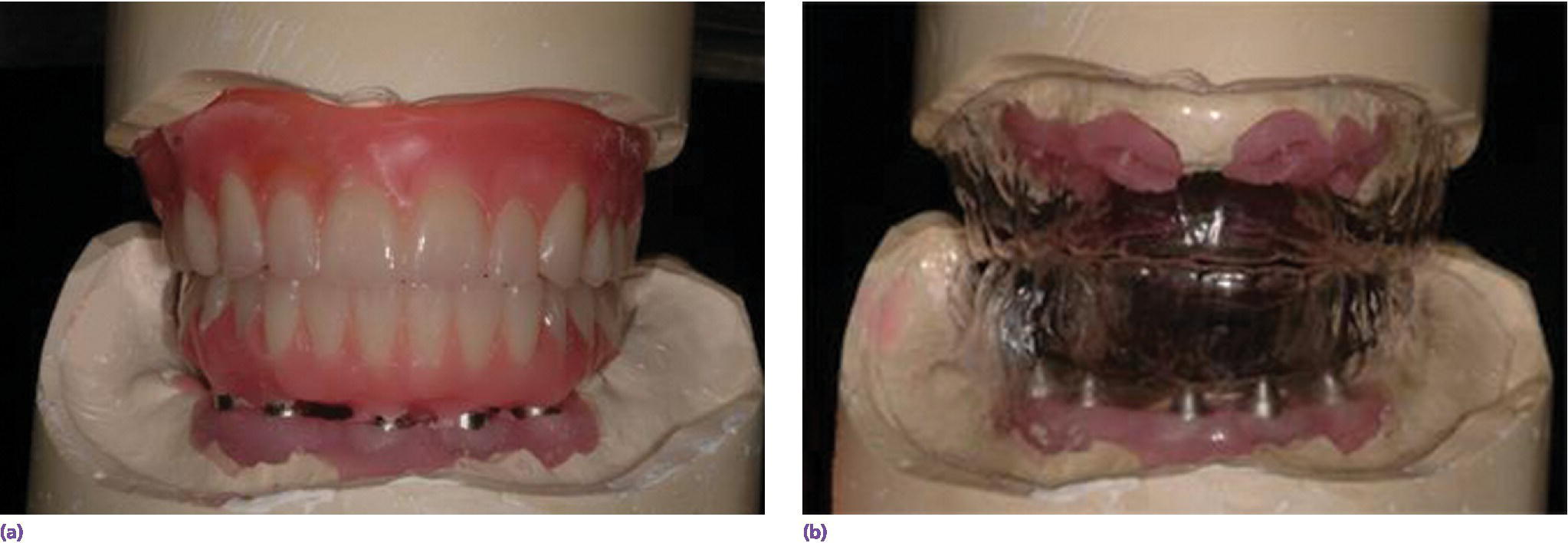
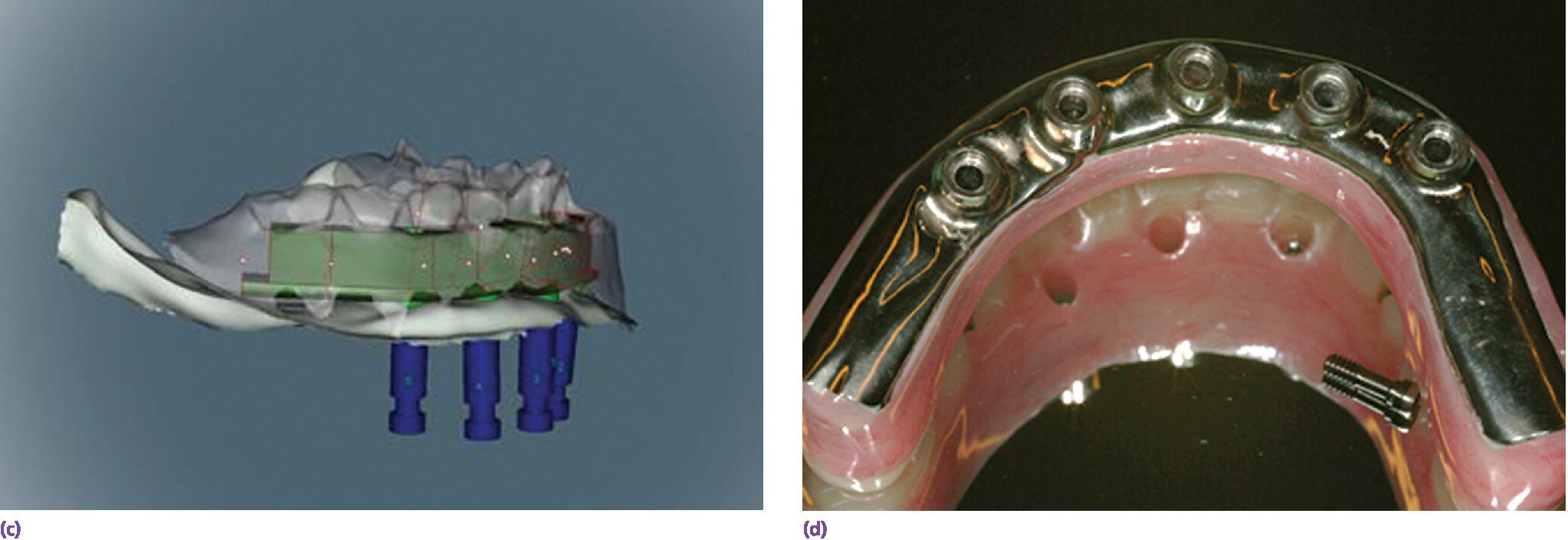
Figure 19.2 (a) Analog wax‐up. (b) Wax‐up permits spatial considerations for planning and fabricating maxillary and mandibular prostheses. (c) Virtual bar design after scan of wax‐up to produce bar structure. (d) Both techniques produce information to determine spatial constraints and proper design of prostheses.
Once patient‐mediated factors are considered, space availability and expected applied forces may be pivotal in the design selection. After a decision has been made, an understanding of material properties will aid further in making these decisions.
Mandibular edentulism has been approached from a number of different vantage points, and has been treated from a variety of approaches. Although there are limited studies which indicate specific protocols for treating patients with mandibular edentulism,16 some evidence of improvement in function does exist when using bone‐anchored prostheses. Patients who are dissatisfied with their mandibular dentures can be treated with new prostheses, or have treatment with dental implant anchorage with overdentures or fixed prostheses; these may have different outcomes.23 Treatment with implant‐assisted prostheses is preferable for patients with regard to efficient function. In fact, dietary choices are very different in those treated with a maxillary complete denture and implant‐supported mandibular prostheses in comparison to those treated with conventional complete dentures.24
Maxillary edentulism appears to be well treated with conventional complete dentures, as supported by many randomized studies, which have used the maxillary complete denture as a standard treatment. If patients express a level of satisfaction with a conventional maxillary complete denture, there is little evidence of any advantages of offering further treatment with implant stabilization. However, if stability or retention is not met, the patient may be offered a variety of treatment alternatives. The use of four well distributed dental implants for retention of a maxillary overdenture has met with success and substantial improvement in support and retention. With reduced palatal coverage and alloy‐reinforced bases, this seems to be a popular treatment alternative for patient satisfaction (Figure 19.3).25 Acceptance by patients, of a fixed dental prosthesis for maxillary edentulism versus a removable prosthesis, is variable, and requirements in facial, orthognathic, and phonetic forms are likewise variable. The approach to using four strategically placed and angled implants for a fixed prosthesis was introduced some years ago and has been replicated with a high degree of success.26,27 Other authors have reported good success rates with extended implants into the zygoma with auxiliary anchorage in the anterior maxilla for treatment of maxillary posterior atrophy (Figure 19.4),14,28 and, more recently, with extramaxillary orientation.29 Where there is additional deficiency of the premaxillary bone, the use of four zygomatic‐anchored implants has also been advocated as a potential treatment scenario (Figure 19.5).30 Strategies developed for these specialized protocols have targeted reduction of cantilever design, along with angulation of anterior and posterior implants, and a shortened arch form. In any case, systematic reviews indicate a high degree of success using four to six dental implants to restore an arch using a fixed dental prosthesis.31
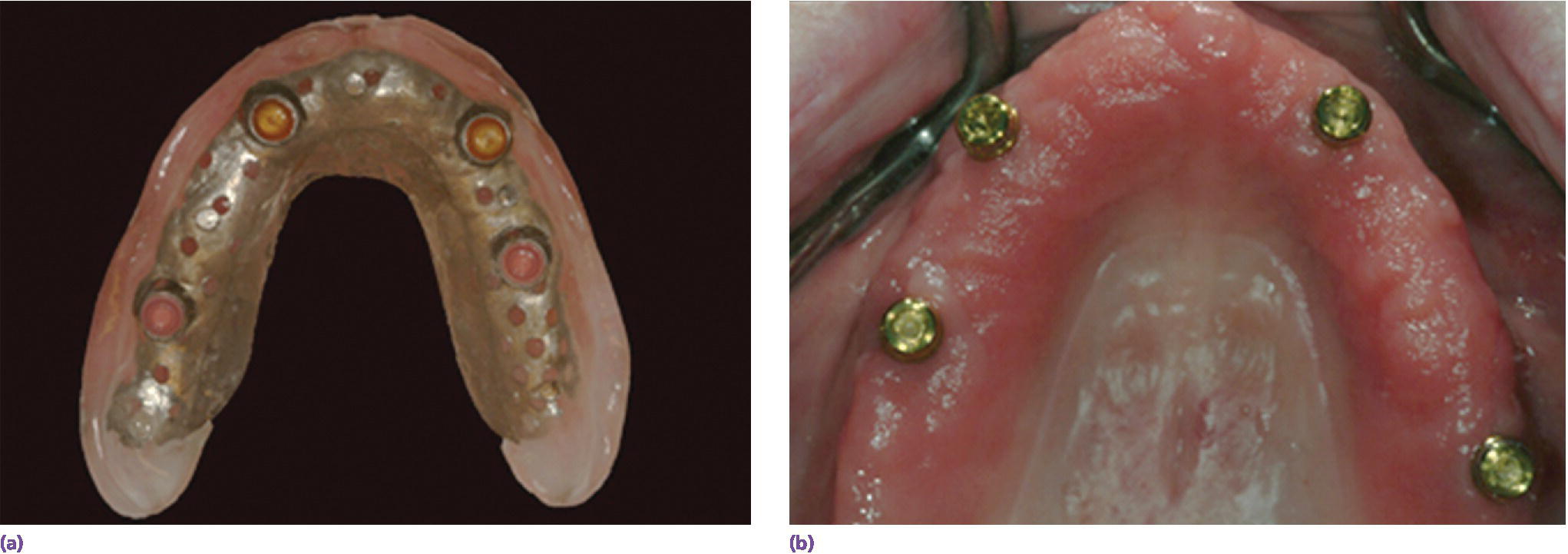
Figure 19.3 (a) Design of overdenture with reduced palatal coverage and metal‐reinforced base. (b) Stud abutments well spaced with potential for servicing.
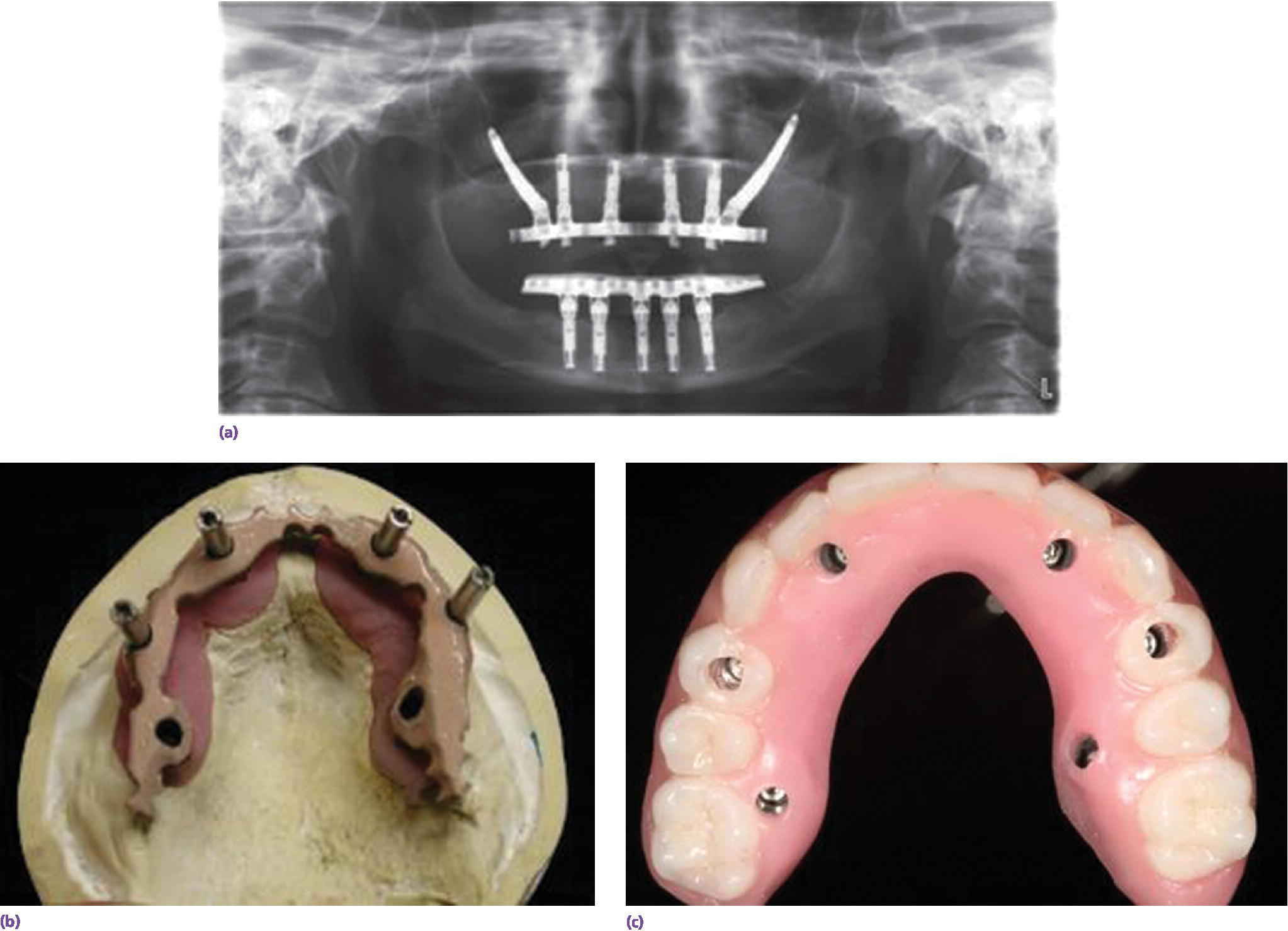
Figure 19.4 (a) Patient treated for anhidrotic ectodermal dysplasia and 10‐year follow‐up indicates some servicing need with multiple acrylic tooth replacements. Good surgical success with zygoma and conventional implants. (b) Silicoated TiAl6V4 frameworks. (c) Laminated with compression‐molded acrylic resin and denture teeth.
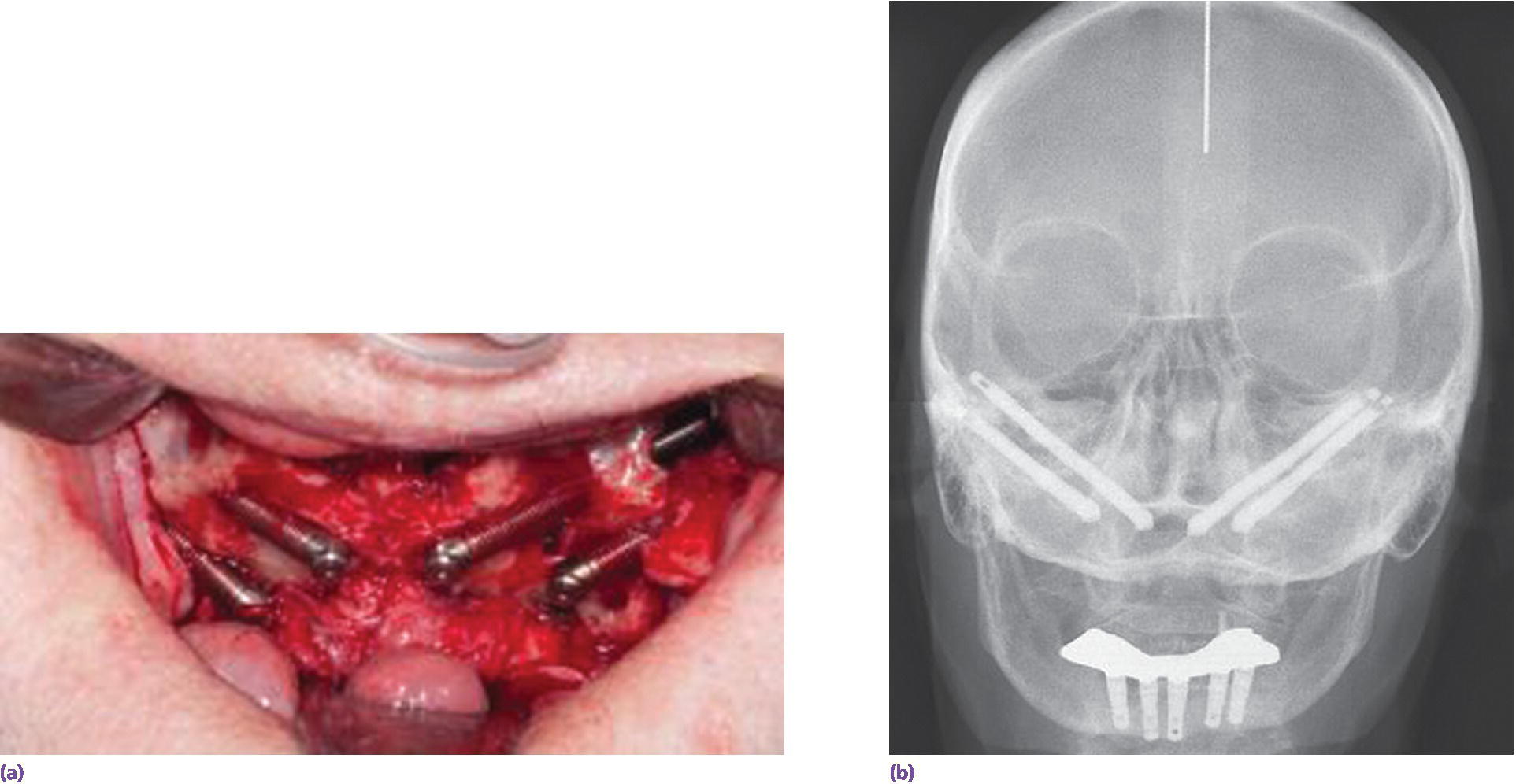
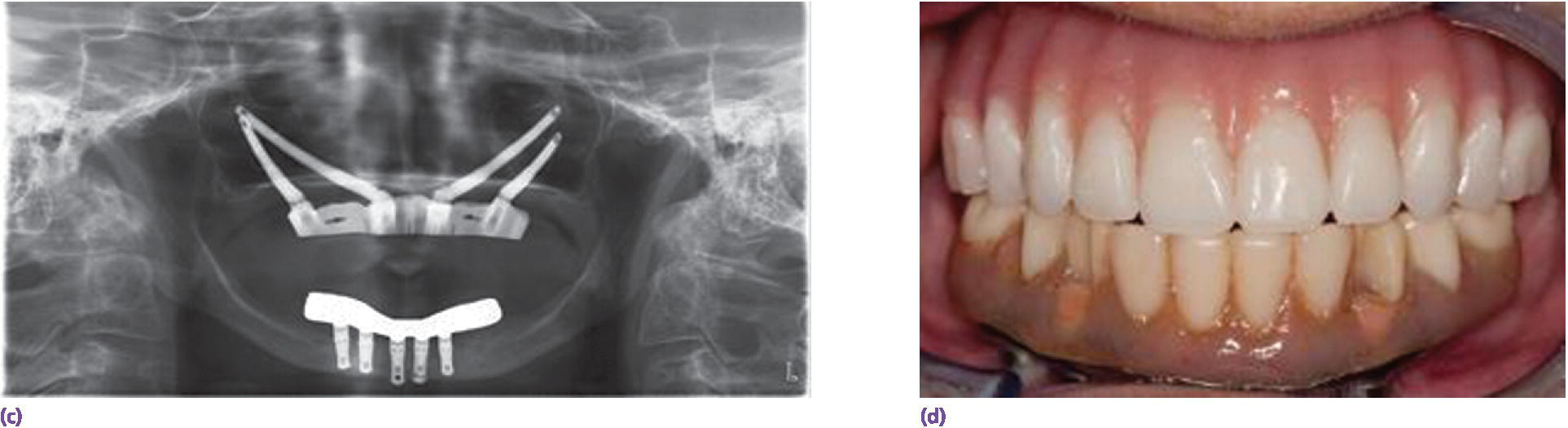
Figure 19.5 (a) Extended‐length zygoma implants placed adjacent to atrophic maxilla. (b) Follow‐up cephalogram indicates stable placement. (c) Radiograph showing subsequent bar attachment. (d) Clinical view with precision‐fit electrical‐discharged machined metal‐based overdenture.
Basic material properties
The range of dental materials has grown considerably over the last decade, with development in polymethylmethacrylate, composite resin, and dental ceramics. A comparison of the materials commonly used for veneering and base construction of implant prosthodontics will give a basic understanding of the gamut of physical properties (Table 19.1). Although methacrylate resin may seem inferior, the ease of repair is attractive, allowing the esthetics, vertical dimension, and occlusal schemes to be redesigned relatively easily.
Table 19.1 Comparison of different restorative material physical properties (PMMA, polymethyl methacrylate).
| Restorative material | Compressive strength1 (MPa) |
Elastic modulus2 (GPa) | Flexural strength3 (MPa) |
Ultimate tensile strength4 (MPa) |
| Cobalt–chromium alloy | 220 | 520–820 | ||
| Feldspathic porcelain | 149 | 70 | 65 | 25 |
| Composite resin | 225 | 21 | 139 | – |
| PMMA | 124 | 1.8–3.1 | 137 | 75 |
| Zirconia | – | 210 | 1087 | – |
| Ti‐6Al‐4 V | 970 | 114 | 903 | 930 |
1 Compressive strength: tested in standard cylinder that has a length of twice its diameter.
2 Elastic modulus: stiffness of a material in elastic range of stress/strain curve.
3 Flexural strength: three‐point bending test of a standard supported beam of material.
4 Ultimate tensile strength: maximum stress material can withstand before failure in tension.
While these materials can be used for a variety of prosthetic constructions, it should be realized that there are fundamental differences in behavior between alloys and ceramics. As stress is applied to metals, it becomes evident that an elastic and plastic deformation occurs. With regard to ceramics, however, this behavior is quite different and, despite high yield strengths of these materials, they may fail abruptly under an increased load (Figure 19.6).32
Figure 19.6 Stress/strain diagram indicating the brittle nature of ceramics in comparison to alloys.
Although material consideration is important for understanding construction requirements, thorough diagnosis and design principles will also need consideration. Patients requiring full‐arch prosthesis replacement of a dentition can be treated in a variety of pathways. The primary diagnostic sequences should give a general vision of patient expectations, available anatomy, interarch distances, and biomechanical design. Available anatomy is evaluated in a three‐dimensional (3‐D) form to give some correlation between diagnosis and treatment planning (Figure 19.7). In correlating this phase with patient expectations, the treatment team can properly plan the treatment sequencing to arrive at a predictable result. The first part of this anatomical consideration is to assure sufficient bone volume exists to meet the foundational need in planning implant location. On this basis, biomechanical design and interarch distance can prompt material selection, so that the surgical and prosthodontic disciplines are synergistically linked (Figure 19.8).
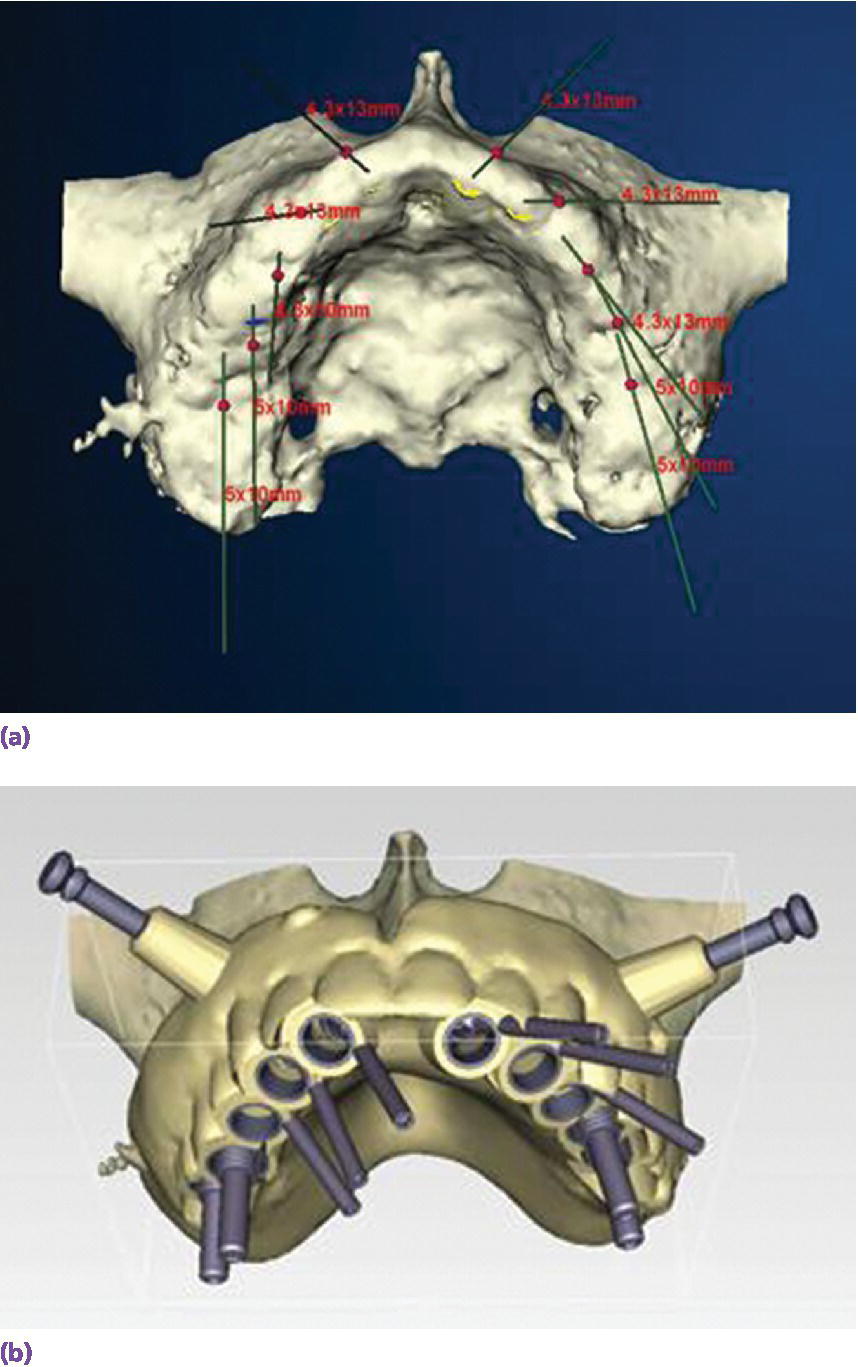
Figure 19.7 A patient presented with significant alveolar bone, desiring a fixed prosthesis. (a) Digital surgical planning with CT scan for site selection and implant angulation for screw‐retained prosthesis. (b) Surgical template fabrication from plan to carry out surgery supportive of prosthesis design.


Figure 19.8 Prosthodontic treatment of patient planned in Figure 18.7. (a) High school graduation photo of patient with desired esthetics. (b) Definitive prostheses with satisfactory lip support and achieved esthetics. (c) Radiographic survey of definitive prostheses.
Once patient‐mediated factors are considered, space availability and expected applied forces may be pivotal in the material selection. After foundational planning, a working knowledge of biomechanics should help the treatment team to understand the advantages that a screw joint imparts to the stability of multiple implant interfaces.
Basic screw joint mechanics
In the interests of efficient workflow and understanding the potential need for retreatment, consideration of screw joint mechanics is essential when constructing dental prostheses. Force transmission from the prosthesis to the implant platform is of primary concern. The surfaces that will participate in this will be those that are intended for force transfer and those that are orientation features.33 The most common configurations have been force transfer to a flat or conical implant connection, and, despite a trend to the conal variety, these do not demonstrate superior mechanical resistance in the long term.33,34 Preload, the compressive force between the platform and abutment, is important to allow sufficient generation of clamping force.36 This is generated by internal tensile stress in the screw, called pretension. When two surfaces are clamped together, the total zone of contact will transmit the applied load, making this successful long term (Figure 19.9). By this principle, the contact surfaces bear the primary load (up to 90%) and shield transfer of the load to the screw, making the components act as one. To accomplish the goal of a sufficiently strong screw joint, a standard application of torque is essential, and this should be applied with a calibrated torque delivery device. As mentioned, preload generated by a screw joint creates a clamping force, which stabilizes over the surface area of prosthetic abutment‐to‐implant connection. Between 2% and 10% of this clamping force will attenuate after flattening and loading of these surfaces under function.37
Figure 19.9 Clamping forces exerted between two surfaces when torque is applied to a screw securing two surfaces. (a) Pre‐tension in the screw is created that is shielded from the compression forces (preload) stabilizing the two plates. (b) The measure of load‐bearing surface area between implant platform and prosthesis is optimal when maximized for force transfer.
Force transfer and biomechanics
Force transfer from the prosthesis to the abutment or implant interface places emphasis on consideration of the available bone support. For instance, using a specific implant number, ideally and widely distributed throughout an edentulous arch with available restorative distance, results in little need for cantilevering where direct prosthesis‐to‐implant connections might be used (Figure 19.10). In these circumstances, the use of screw‐ or cement‐retained abutments, or a combination thereof, is feasible.
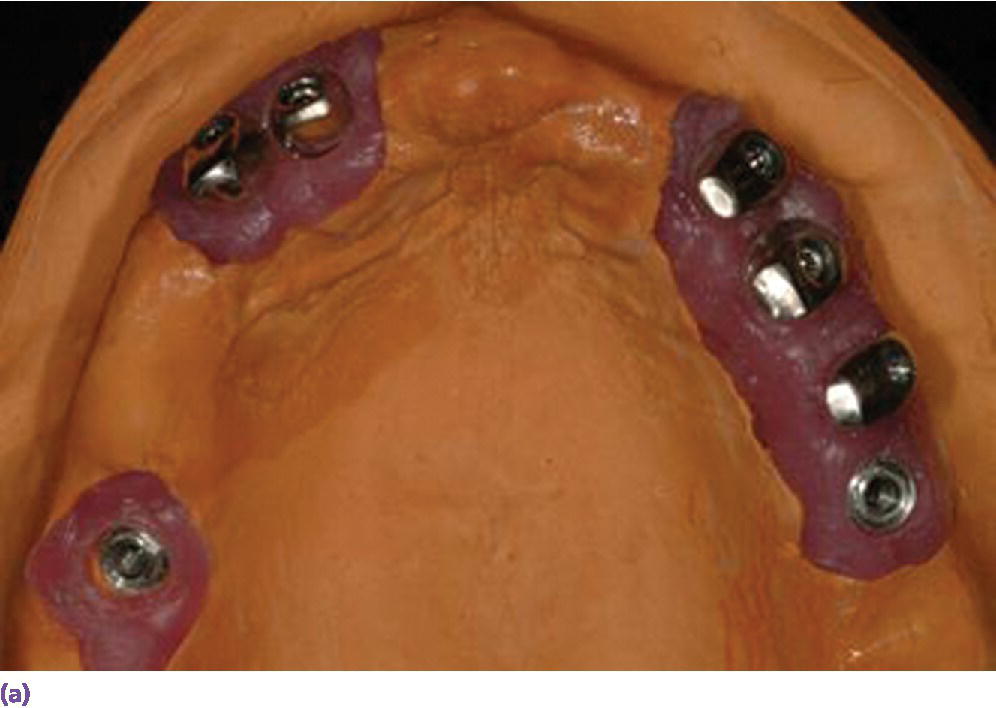

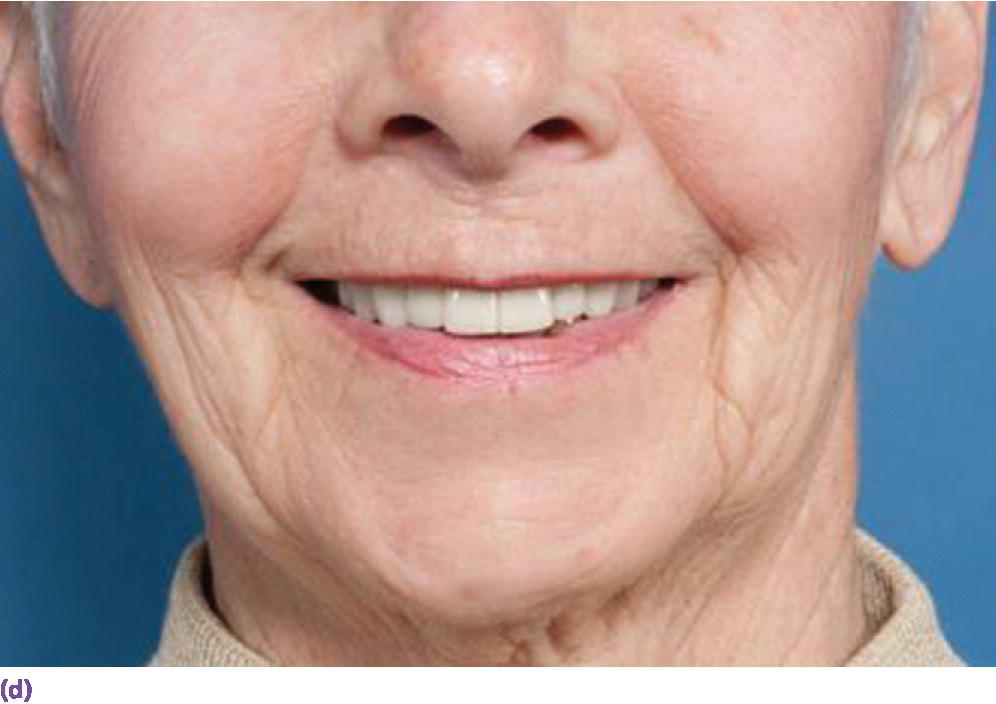
Figure 19.10 Patient with failing maxillary dentition presented with limited bone and sites selected with available bone. (a) Telescopic abutment design for angle correction and auxiliary screw retention on posterior implants. (b) Metal–ceramic design with cross arch splinting. (c) Intaglio of prosthesis showing telescopic retainers and direct‐to‐fixture screw connections. (d) Final esthetic result with fixed dental prosthesis.
The use of screw retention versus cementation appears controversial, but it certainly is advantageous to make the restoration retrievable, as it can be better serviced for technical complications if needed.38 Because of technique, material, and component developments, modern survival statistics for screw‐retained reconstructions are very different compared to those from studies prior to 2001.39 This paper reported updated prosthetic survival results for screw‐ and cement‐retained restorations, documenting similar 5‐year rates. The use of cemented prostheses seems to be problematic and associated with more biologic complications.40 Larger implant diameters seem to be associated with a greater chance of extravasated cement.41
In other circumstances, where there is limited bone or inability to distribute implants widely throughout the arch, the use of cantilevering or angle correction design may become necessary (Figure 19.11). The choice of using a direct implant connection to maximize preload is preferable, as this will reduce the likelihood of overloading the prosthetic screw assembly, a problem considered more likely with reduced screw diameter. Cantilever design has been controversial with implant prosthodontics. Two independent systematic reviews42,43 indicate that distal cantilevers on fixed implant prostheses do not carry a high risk of mechanical complications; other observational reports indicate an apposition of bone in arches restored with cantilevered prosthetics.44 Other reports indicate that, although biologic complications appear to be absent, technical complications, including veneer fracture, were common10,45 and may be related to deflection of the connector under load. In these cases, the deflection of a beam is inversely related to the third power of the occlusal gingival thickness. Use of stiffer materials imparts more tension to the most anterior screw joint, in which case a direct connection to the implant platform may be desirable for maximum resistance. The deformation of implant components beneath cantilever segments has also been controversial, as this clearly does occur, as demonstrated in laboratory studies (Figure 19.12).46 Some of this can be attributed to the differential hardness between the prosthetic alloy and components, where stiff alloys, such as palladium–copper, cobalt–chromium, or ceramic, may deform titanium after years of functioning. Supplying new components in these cases can be difficult as manufacturers redesign restorative systems, making original implant components obsolete and unavailable. It is a challenge to use stiffer materials to overcome this flexure of cantilever design, but it may be met with the alternative of alloyed titanium. Although alloyed titanium may be less likely to deform the underlying abutment or implant platform, continued high cycle flexure may have tendency to delaminate the veneering material.
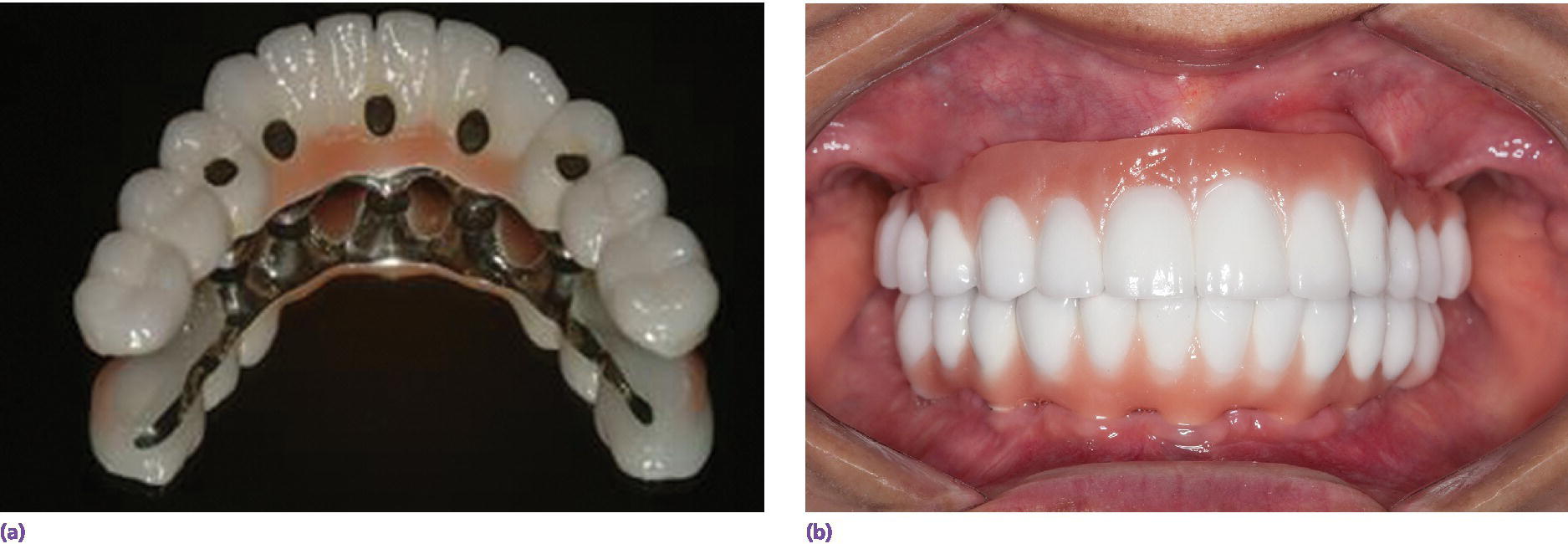
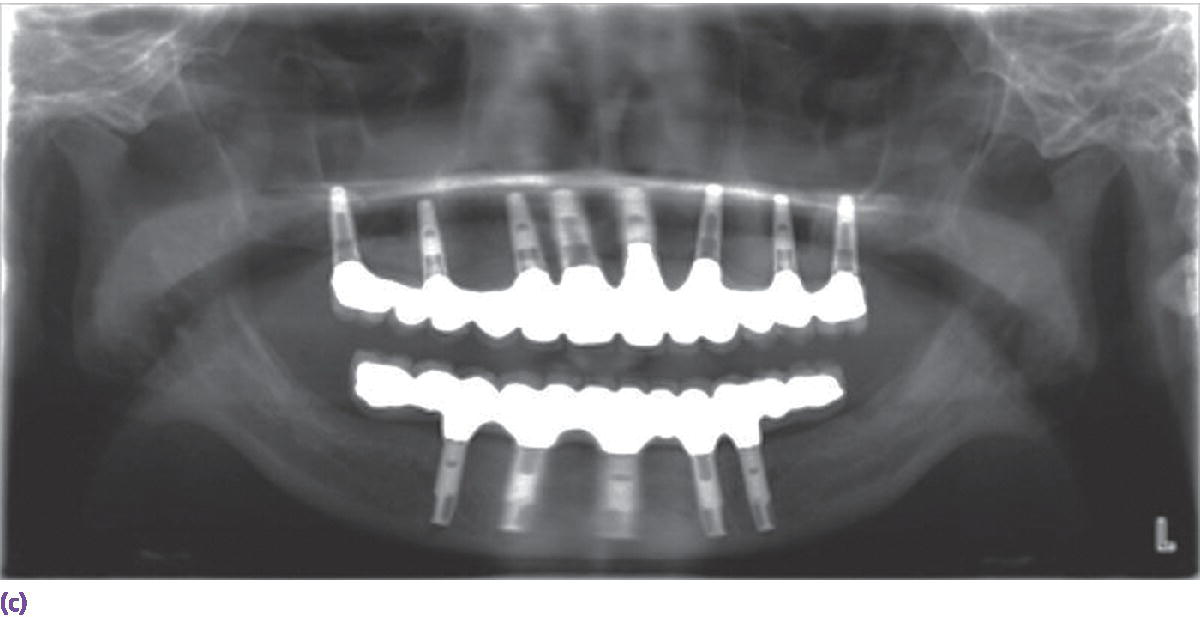
Figure 19.11 (a, b, c) Prosthesis construction included direct‐to‐fixture connection to secure cantilever design as sole osseous anchorage in interforaminal mandible opposing a maxillary fixed dental prosthesis. Palladium–copper framework used to obtain maximal resistance to stress on cantilevered area.

Figure 19.12 Standard abutments removed after 10 years of functioning beneath a fixed dental prosthesis with cantilevered design. Note the lip formed at the supporting portion of the abutments.
Prosthesis design
Overdentures
Traditionally, overdenture design was a classic approach for treatment of complete edentulism. Although minimal changes have been evident in methacrylate resin composition, aside of plasticizers and coloring agents, processing methods by continuous injection and low heat curing have resulted in a significant reduction in the amount of total dimensional changes upon polymerization.47 Spatial considerations for overdenture design have been suggested from an empirical approach.48 More specifically, the overdenture minimum thickness should be at least 2 mm49 (with a stock denture tooth requiring at least 3 mm of thickness).50 Spatial requirements of the resin base, prosthetic denture teeth, and attachment mechanisms should provide sufficient resistance under load where at least 2 mm of resin base is a foundation for the other components.51 Vertical restorative space is the primary consideration, and has a bearing on base reinforcement, alveoloplasty, intentional vertical dimension increase, occlusal plane repositioning, and overdenture attachment selection.
Some reviews have given rise to understanding resistant design in the long‐term management of these prostheses, and have led to the use of a cast reinforced framework (Figure 19.13).52 The reinforced base is more resistant to crack propagation and ultimate failure. The use of this reinforced design in patients with parafunctional activity and opposing natural or implant‐borne dentition may also be useful in reducing crack development and propagation. Resin‐to‐metal bonding is also beneficial, by making this union more chemically based, further enhancing the long‐term stability and resistance to microleakage, which occurs where an inherent gap exists between the two phases of materials.53,54
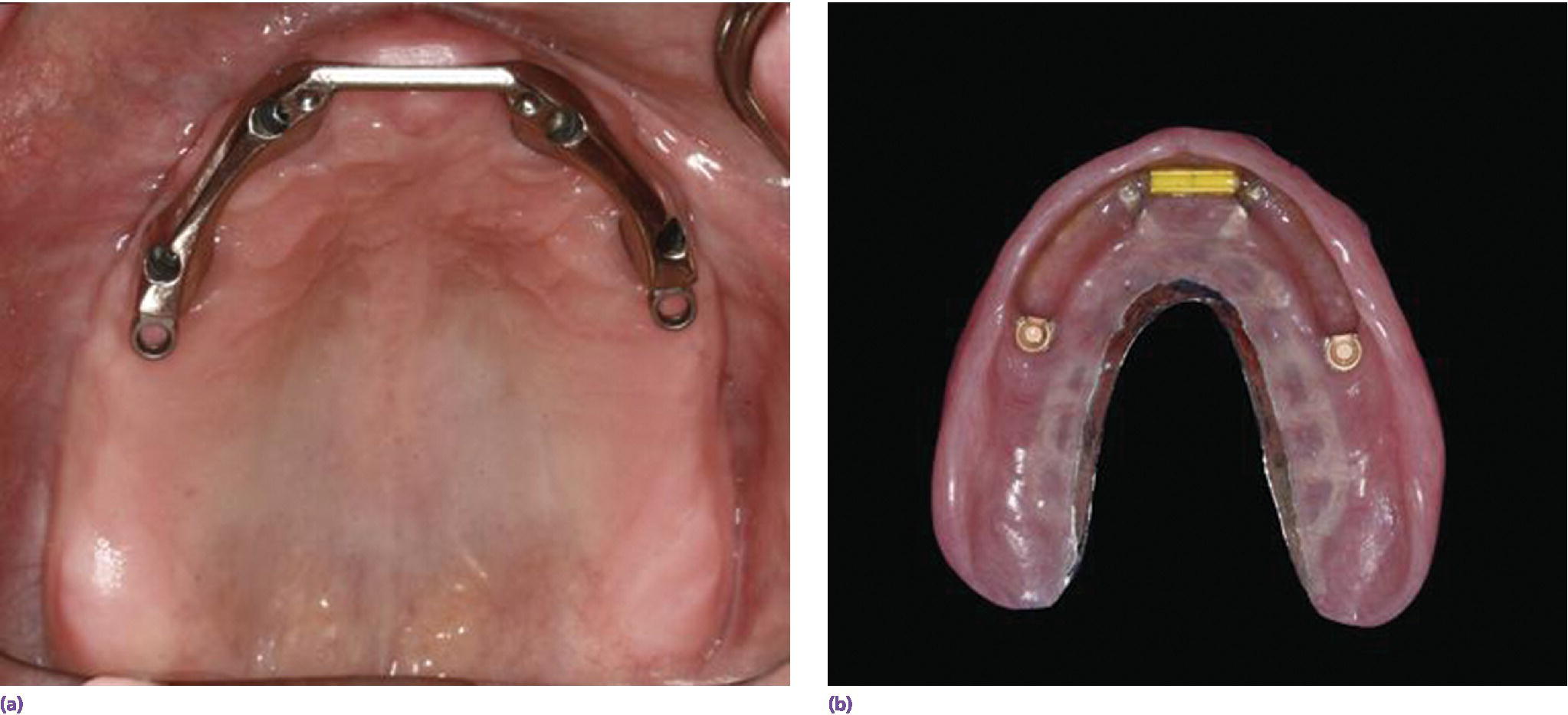
Figure 19.13 (a) Hader bar attachment in support and retention for (b)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


