Combined Surgical and Orthodontic Treatment
INDICATIONS FOR ORTHOGNATHIC SURGERY
DEVELOPMENT OF ORTHOGNATHIC SURGERY
THE BORDERLINE PATIENT: CAMOUFLAGE VERSUS SURGERY
Malocclusion Severity as an Indication for Surgery
Orthognathic Surgery versus Temporary Skeletal Anchorage
Esthetic and Psychosocial Considerations
CONTEMPORARY SURGICAL TECHNIQUES
SPECIAL CONSIDERATIONS IN PLANNING SURGICAL TREATMENT
PUTTING SURGICAL AND ORTHODONTIC TREATMENT TOGETHER: WHO DOES WHAT, WHEN?
Indications for Orthognathic Surgery
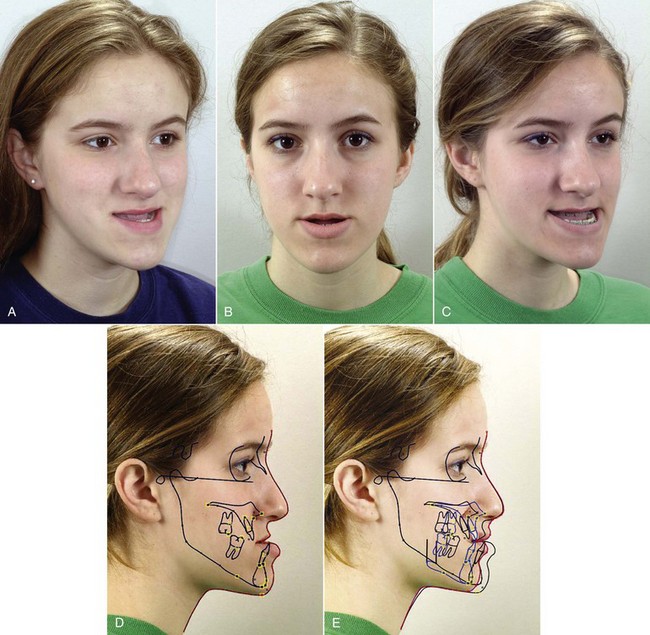
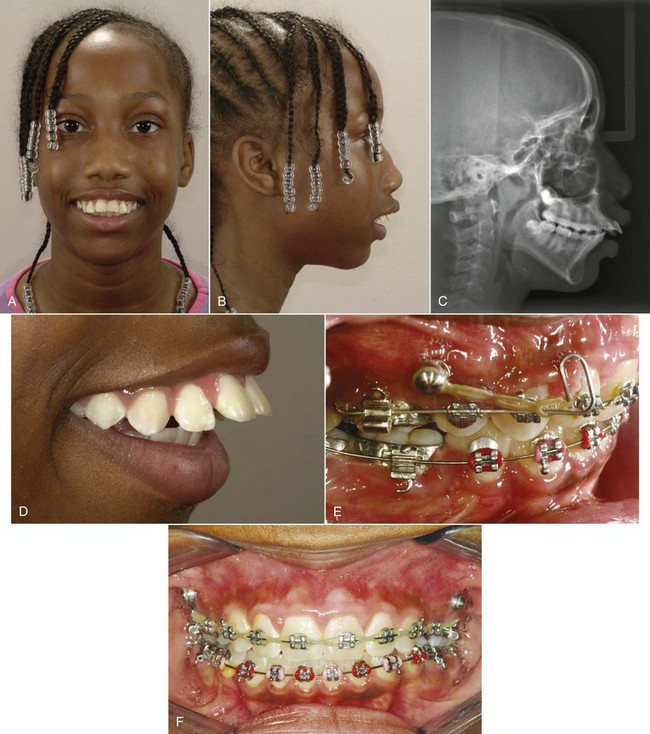
For patients whose orthodontic problems are so severe that neither growth modification nor camouflage offers a solution, surgery to realign the jaws or reposition dentoalveolar segments is the only possible treatment. Surgery is not a substitute for orthodontics in these patients. Instead, it must be properly coordinated with orthodontics and other dental treatment to achieve good overall results. Dramatic progress in recent years has made it possible for combined treatment to correct many severe problems that simply were untreatable only a few years ago (Figure 19-1).
Development of Orthognathic Surgery
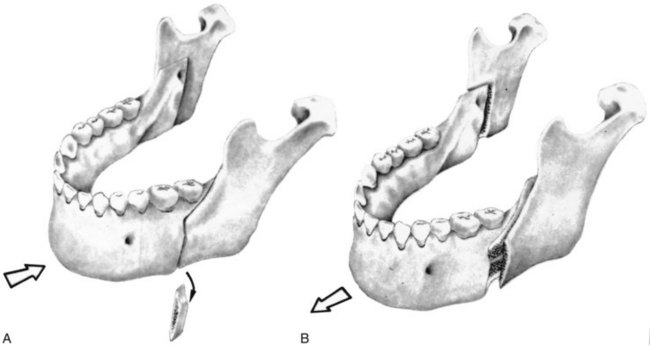
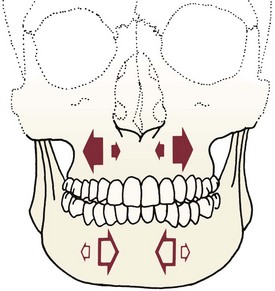
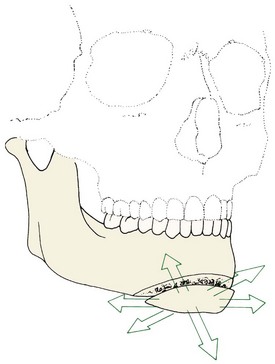
Surgery for mandibular prognathism began early in the twentieth century with occasional treatment that consisted of a body ostectomy, removing a molar or premolar tooth and an accompanying block of bone. Edward Angle, commenting on a patient who had treatment of this type over 100 years ago, described how the result could have been improved if orthodontic appliances and occlusal splints had been used. Although there was gradual progress in techniques for setting back a prominent mandible throughout the first half of this century, the introduction of the sagittal split ramus osteotomy in 1957 marked the beginning of the modern era in orthognathic surgery.1 This technique used an intraoral approach, which avoided the necessity of a potentially disfiguring skin incision. The sagittal split design also offered a biologically sound method for lengthening or shortening the lower jaw with the same bone cuts, thus allowing treatment of mandibular deficiency or excess (Figure 19-2).
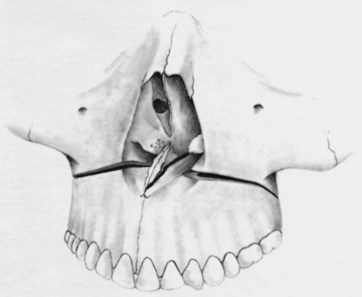
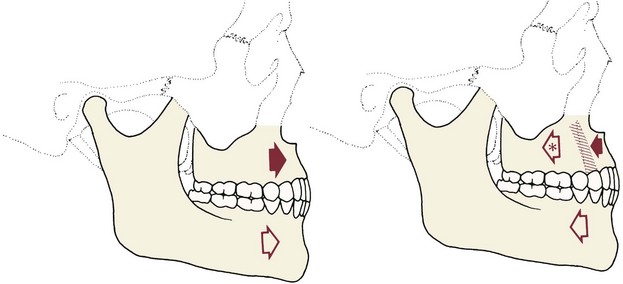
During the 1960s, American surgeons began to use and modify techniques for maxillary surgery that had been developed in Europe, and a decade of rapid progress in maxillary surgery culminated in the development of the LeFort I downfracture technique that allowed repositioning of the maxilla in all three planes of space (Figure 19-3).2,3 By the 1980s, it was possible to reposition either or both jaws, move the chin in all three planes of space, and reposition dentoalveolar segments surgically as desired. In the 1990s, rigid internal fixation greatly improved patient comfort by making immobilization of the jaws unnecessary, and a better understanding of typical patterns of postsurgical changes made surgical outcomes more stable and predictable. With the introduction of facial distraction osteogenesis around the turn of the century and its rapid development since then, larger jaw movements and treatment at an earlier age became possible for patients with the most severe problems (usually related to syndromes).
The Borderline Patient: Camouflage Versus Surgery
Malocclusion Severity as an Indication for Surgery
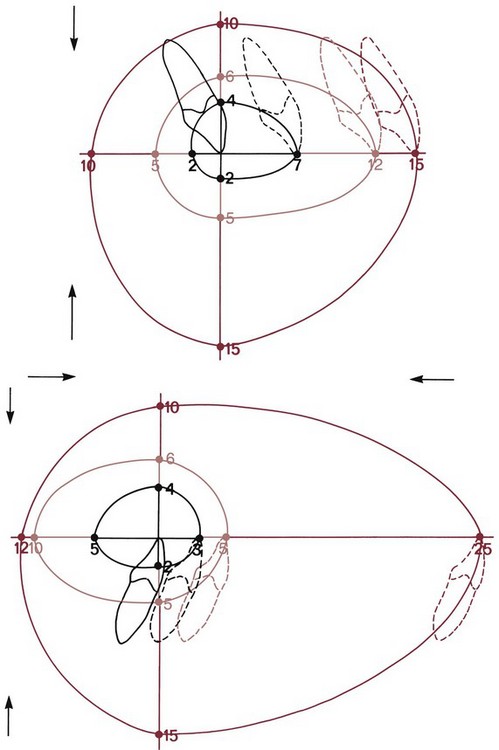
One indication for surgery obviously is a malocclusion too severe for orthodontics alone. It is possible now to be at least semiquantitative about the limits of orthodontic treatment in the context of producing normal occlusion. As the diagrams of the “envelope of discrepancy” (Figure 19-4) indicate, the limits vary both by the tooth movement that would be needed (teeth can be moved further in some directions than others) and by the patient’s age (the limits for tooth movement change little if any with age, but growth modification is possible only while active growth is occurring). Because growth modification in children enables greater changes than are possible by tooth movement alone in adults, some conditions that could have been treated with orthodontics alone in children (e.g., a centimeter of overjet) become surgical problems in adults. On the other hand, some conditions that initially might look less severe (e.g., 5 mm of reverse overjet) can be seen even at an early age to require surgery if they are ever to be corrected.
Keep in mind that the envelope of discrepancy outlines the limits of hard tissue change toward ideal occlusion, if other limits due to the major goals of treatment do not apply. In fact, soft tissue limitations not reflected in the envelope of discrepancy often are a major factor in the decision for orthodontic or surgical–orthodontic treatment. Measuring millimeter distances to the ideal condylar position for normal function is problematic, and measuring distances from ideal esthetics is impossible. The diagnostic and treatment planning approach discussed in Chapters 6 and 7 reflects a greater emphasis on soft tissue considerations in modern treatment and is essential when camouflage versus surgery is considered.
Orthognathic Surgery versus Temporary Skeletal Anchorage
The advent of temporary skeletal anchorage in the form of miniplates or bone screws has led many orthodontists to wonder if this could decrease the number of patients who would need surgery. Applications of skeletal anchorage in treatment of adults have been discussed in detail in Chapter 18. Tooth movement for patients with a jaw discrepancy, of course, is camouflage—successful only if the jaw discrepancy is no longer apparent enough to be a problem. It is true that protruding maxillary incisors in a patient with mandibular deficiency can be retracted further with skeletal anchorage. This is as likely to produce a camouflage failure as to correct the problem. The limits of orthodontic treatment are much more a matter of facial appearance than anchorage.
There are two circumstances, however, in which skeletal anchorage may be an alternative to orthognathic surgery. Moving the maxilla up with a LeFort I osteotomy is highly stable and predictable and has made it possible to correct anterior open bite/long-face problems that previously could not be treated. Maxillary posterior teeth can be intruded using miniplates at the base of the zygomatic arch or long bone screws reaching into the same area (see Figures 18-50 to 18-52). It is clear now that 3 to 4 mm intrusion can be obtained, with an expected short-term relapse of about 1 mm, and that for the average patient, 2 mm closure of the open bite occurs for every 1 mm posterior intrusion. At this point, however, neither the long-term stability of this treatment nor the limits of intrusion have been established. The indications and contraindications for posterior intrusion will become much clearer in the next few years.
The other interesting possibility for skeletal anchorage is protraction of the maxilla in preadolescent children (see Chapter 13). It is apparent now that Class III elastics to skeletal anchors in the posterior maxilla and anterior mandible are more effective than reverse-pull headgear to the teeth in moving the maxilla forward. As with face mask treatment, however, the moment of truth comes during adolescence, when mandibular growth can lead to a return of the Class III problem. Can the maxilla be moved far enough forward at ages 10 to 12 to prevent the need for later surgical advancement? For some children, this seems likely, but no data exist for long-term outcomes, and the more the problem is mandibular prognathism than maxillary deficiency, the greater the chance of growth that eventually will require surgery.
Esthetic and Psychosocial Considerations
The negative effect on psychic and social well being from dentofacial disfigurement is well documented,4,5 and it is clear that this is why most patients seek orthodontic treatment. Those who look different are treated differently, and this becomes a social handicap. Treatment to overcome social discrimination is not “just cosmetic.” It is neither vain nor irrational to desire an improvement in facial appearance that can improve one’s total life adjustment. This motivation, not surprisingly, is even stronger in patients with the more severe deviations from the norm that might require orthognathic surgery. If an improvement in appearance is a major goal of treatment, it makes sense that in addition to the jaws and teeth, changes in the nose, and perhaps other changes in facial soft tissue contours that could be produced by facial plastic surgery, should also be considered in the treatment planning. The integration of orthognathic and facial plastic surgery is a current and entirely rational trend.
The great majority of patients who undergo orthognathic procedures report long-term satisfaction with the outcome (80% to 90%, depending on the type of surgery). A similar number say that, knowing the outcome and what the experience was like, they would recommend such treatment to others and would undergo it again.6 On long-term recall, patients often comment that the changes produced by their surgery gave them the confidence they needed in order to succeed in their business or profession.
This does not mean, of course, that there are no negative psychologic effects from surgical treatment. First, a few patients have great difficulty in adapting to significant changes in their facial appearance. This is more likely to be a problem in older individuals. If you are 19, your facial appearance has been changing steadily for all your life, and another change is not a great surprise. If you are 49 and now suddenly see a different face in the mirror, the effect may be unsettling. Psychologic support and counseling therefore are particularly important for older patients, and major esthetic changes in older adults may not be desirable. As we have discussed in Chapter 18, adults seeking treatment fall into two groups: a younger group who seek to improve their lot in life and an older group whose goal is primarily to maintain what they have. The older group may need orthognathic surgery to achieve their goal, but for them, often treatment should be planned to limit facial change, not maximize it.
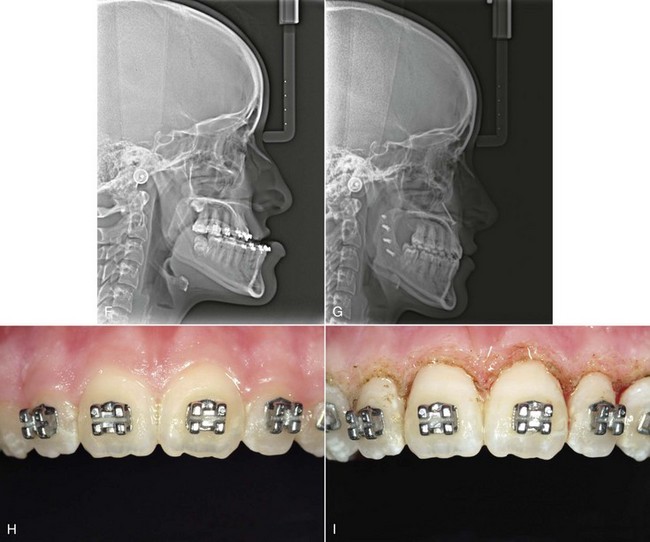
Second, whatever the age of the patient, a period of psychological adjustment following facial surgery must be expected (Figure 19-5). In part, this is related to the use of steroids at surgery to minimize postsurgical swelling and edema. Steroid withdrawal, even after short-term use, causes mood swings and a drop in most indicators of psychologic well being. The adjustment period lasts longer than can be explained by the steroid effects, however. The surgeon learns to put up with complaining patients for the first week or two postsurgery. By the time orthodontic treatment resumes at 3 to 6 weeks postsurgery, the patients are usually—but not always—on the positive side of the psychologic scales. Sometimes the orthodontist also has to wait for a patient to make peace with his or her surgical experience.
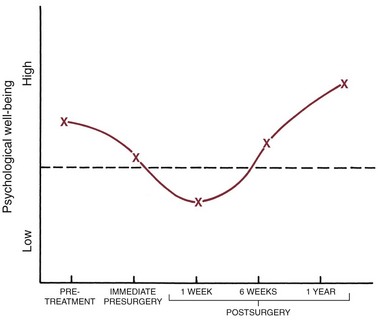
FIGURE 19-5 A generalized representation of the typical psychological response to orthognathic surgery, based on the work of Kiyak.16 Prior to treatment, patients who seek orthognathic surgery tend to be above the mean on most psychosocial parameters. Immediately before surgery, they are not quite so positive, as anxiety and other concerns increase. In the days immediately after surgery, a period of negativism typically occurs (e.g., depression, dissatisfaction). This is related in part to steroid use at surgery and withdrawal afterward but is not totally explained by this. By 6 weeks postsurgery, the patients usually are on the positive side of normal again and at 1 year, typically rate quite high for satisfaction with treatment and general well-being.
Computer Simulation of Alternative Treatment Outcomes
It always has been a moral and ethical imperative to allow the patient to make important decisions about what treatment he or she will accept, and now it is a legal obligation as well. Involving the patient as decisions are made about the choice of alternative treatments is an essential element of informed consent (see Chapter 7).
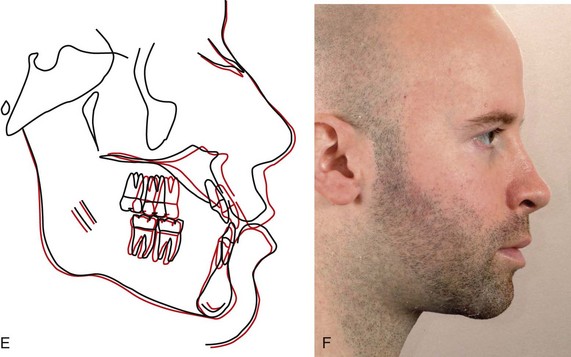
Computer image predictions are particularly valuable in helping patients decide between camouflage and surgery and in planning surgical treatment. The patient can view the impact on the soft tissue profile of orthodontic camouflage versus surgery when these are realistic treatment alternatives (Figure 19-6) and also view the effect of varying amounts of surgical change—more or less mandibular advancement, for example, or the effect of genioplasty or rhinoplasty in addition to change in jaw position. Predictions of changes in the frontal view still are artwork rather than scientifically based, but current computer prediction programs do a good job of predicting profile changes,7 and steady improvements continue to occur. It is one thing to describe in words what the different outcomes of camouflage and surgery would be and something else to help the patient visualize it by seeing image predictions.
At one point, there was great concern that showing predictions to patients might lead to unrealistic expectations and disappointment with the actual result, but patient responses show that this risk is minimal or nonexistent. In a randomized trial, those who saw the prediction images before surgery were more, not less, likely to be satisfied with their result.8 Only the patient can decide whether the difference between surgical correction of jaw relationships and orthodontic camouflage would be worth it in terms of the additional risk and cost of surgery. Computer simulations help them do that.
Extraction of Teeth and the Camouflage/Surgery Decision
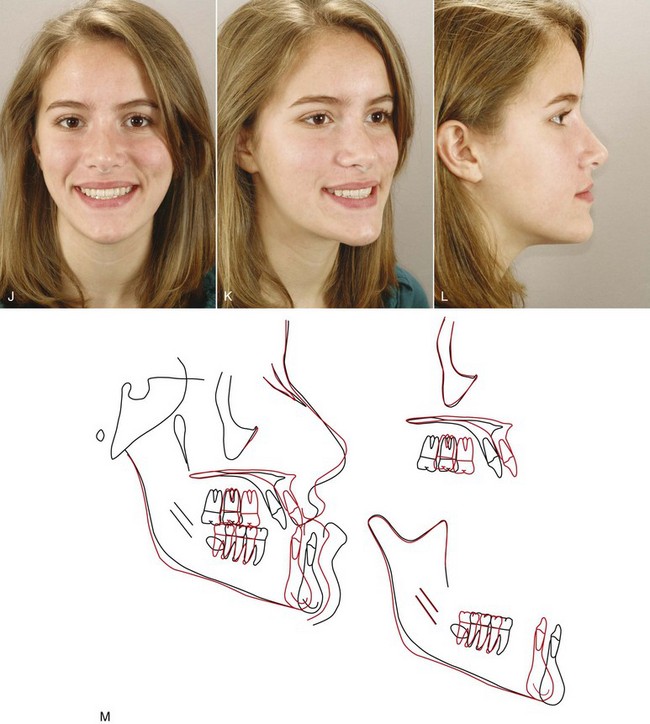
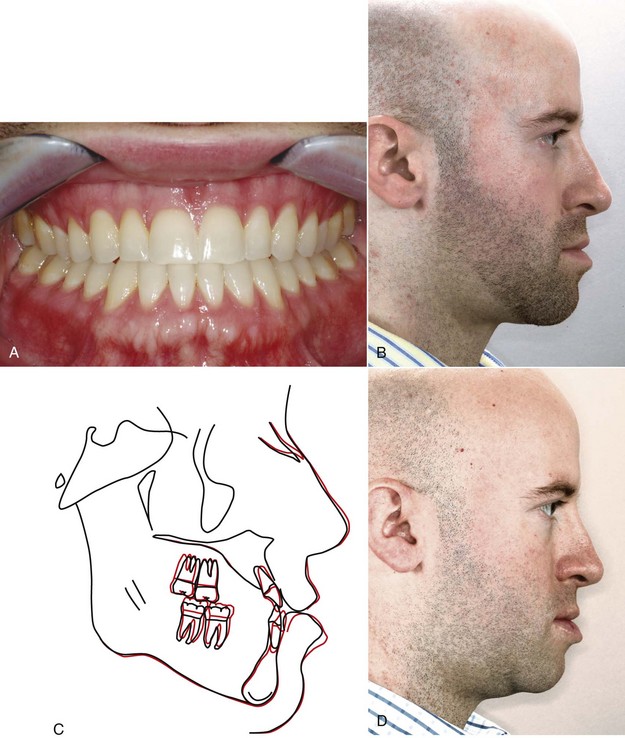
The decision for camouflage or surgery must be made before treatment begins because the orthodontic treatment to prepare for surgery often is just the opposite of orthodontic treatment for camouflage. It is a serious error to attempt camouflage on the theory that if it fails, the patient can then be referred for surgical correction. At that point, another phase of “reverse orthodontics” to eliminate the effects of the original treatment will be required before surgery can provide both normal jaw relationships and normal occlusion (Figure 19-7).
The critical importance of deciding on camouflage or surgery at the beginning of treatment is illustrated by the difference in extractions needed with the two approaches. In camouflage, extraction spaces are used to produce dental compensations for the jaw discrepancy and the extractions are planned accordingly. For example, with orthodontic treatment alone, a patient with mandibular deficiency and a Class II malocclusion might have upper first premolars removed to allow the retraction of the maxillary anterior teeth. Extraction in the lower arch would be avoided, and the lower incisors probably would be tipped facially to help reduce the overjet (Figure 19-8).
The extraction pattern for this same patient would be quite different if mandibular advancement were planned (see Figure 19-6). Instead of creating dental compensation for the jaw deformity, the orthodontic treatment now would be planned to remove it. In the upper arch, the position of the incisors relative to the maxilla often is normal or retrusive; if so, upper premolar extraction would be undesirable. Often in mandibular deficiency the lower incisors are protrusive relative to the chin. Then there are two possibilities: extraction in the lower arch to retract them and temporarily increase the overjet so the chin will be brought further forward when the mandible is advanced or a lower border osteotomy to move the chin forward.
A similar but reversed situation would be seen in a patient with a skeletal Class III problem. If camouflage were planned, typical extractions might be lower first premolars alone, lower first and upper second premolars, or one lower incisor. Surgical preparation of a Class III patient often requires moving the lower incisors forward and retracting the upper incisors (which may require extraction of upper first premolars) to correct their axial inclinations and increase the reverse overjet (see Figure 19-7). As a general rule, Class III problems are less amenable to camouflage than Class II because retracting the lower incisors may make the chin appear even more prominent, just the opposite of effective camouflage. If space were needed in the lower arch, second rather than first premolar extraction would be a logical choice so that the lower incisors were not retracted.
It obviously is important for the patient who could be treated either way to understand all these considerations in the decision between camouflage and surgery. Although the patient can and must make the decision, it remains true that some conditions can be treated better with orthodontics alone than others, simply because the impact on facial esthetics is likely to be better. Some characteristics that can make the difference between satisfactory camouflage treatment and camouflage failure are summarized in Box 19-1.
Contemporary Surgical Techniques
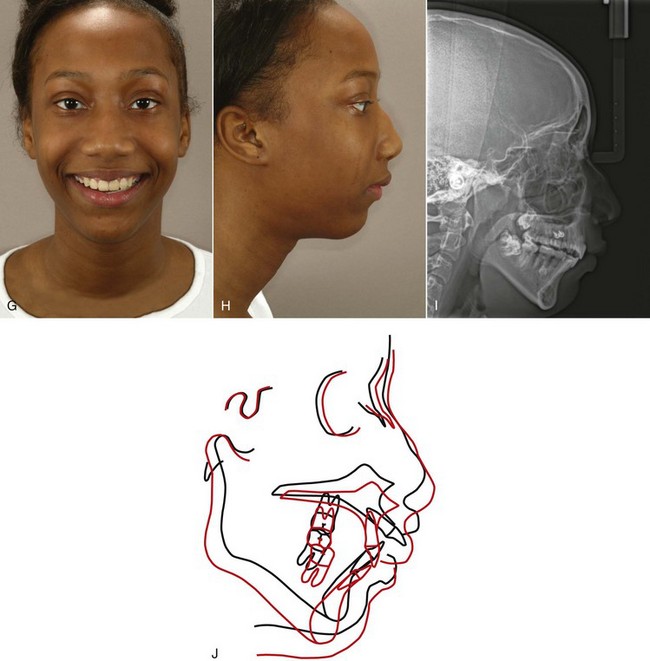
The possible jaw movements with orthognathic surgery are shown diagrammatically in Figures 19-9 and 19-10. As the figures illustrate, both jaws can be repositioned three dimensionally, but not all directions of movement are feasible.
Mandibular Surgery
The sagittal split osteotomy (see Figure 19-2) now is used for almost all mandibular surgery because of several advantages over mandibular body procedures and alternative techniques for ramus surgery:
• The mandible can be moved forward or back as desired, and the tooth-bearing segment can be rotated down anteriorly (increasing the mandibular plane angle) when additional anterior face height is desired.
• It is quite compatible with the use of rigid intraoral fixation (RIF), so immobilization of the jaws during healing is not required.
• Excellent bone-to-bone contact after the osteotomy means that problems with healing are minimized, and postsurgical stability is good.
In contemporary treatment, a lower border osteotomy of the mandible to reposition the chin relative to the mandibular body (Figure 19-11) is a major adjunct to ramus procedures, especially when the mandible is advanced. It is used in about 30% of the patients who receive a ramus osteotomy and in about the same number of patients with maxillary surgery. The lower border procedure allows the chin to be moved transversely, forward or back, and up or down.
Other mandibular procedures are used primarily for major advancements or surgery involving the condyles. An extraoral approach often is required, and a bone graft is likely to be needed. Rarely, a midline osteotomy of the mandible with removal of an incisor is used to narrow it anteriorly.9
Maxillary Surgery
The LeFort I osteotomy with downfracture of the maxilla (see Figure 19-3) dominates contemporary maxillary surgery just as the sagittal split dominates mandibular surgery. It allows the maxilla to be moved up and/or forward with excellent stability. Moving the entire maxilla back is quite difficult because of the structures behind it, but this is not necessary when the upper teeth are protrusive. A segmental osteotomy, closing the space where a premolar was extracted, allows the anterior teeth to be retracted and posterior teeth to be moved superiorly so that anterior open bite is closed as the mandible rotates upward and forward (Figure 19-12). Segmental osteotomies also allow the posterior maxilla to be widened or (less frequently) narrowed.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses