18 The Dental Microscope in Endodontics
Owing to the very small size and complex nature of the tooth root canal system, the naked eye cannot discern in sufficient detail several factors that influence the outcome of endodontic treatment. Problems arising during primary root canal treatment, such as narrow root canal orifices, detection and dealing with obstructions or obliterated canals, and recognizing root canals type III or V–VII (Vertucci, 1984), can severely limit the chances for treatment success.
In addition, endodontic retreatment is usually associated with a myriad of problems that can be effectively overcome only with combined application of the underpinning clinical knowledge and state-of-the-art technology.
The introduction of the clinical dental microscope provided a new dimension in diagnosis and therapy in dentistry. The combination of additional light, magnification, and ergonomic design makes the dental microscope one of the most significant technological developments in endodontology. It permits the effective use of both time-tested techniques and newer therapeutic procedures, and has thus expanded the boundaries of endodontology to include successful maintenance of previously questionable teeth.
As early as 1921, Carl Olof Nylen used a monocular microscope during surgical therapy. In 1975, Baumann described the first use of a microscope in dental practice. He recommended it as a diagnostic and therapeutic aid during caries removal, root canal treatment, during the preparation of dental restorations, and calculus removal. He drew attention to its ergonomic construction, which allows the dentist to adopt an upright seated position during treatment. Following additional technical improvements during the early 1990s, the dental microscope is increasingly used in specialist dental practices.
The dental microscope provides for an optimal clinical diagnosis (Zaugg, 2004). The clinical detection of even the smallest root canal orifices is significantly improved using the dental microscope (Schwarze, 2003). The newest minimally invasive therapeutic procedures for the removal of endodontic pins/posts, root canal filling material, foreign bodies, and fragments in complex retreatment cases can be carried out successfully. In addition, new frontiers in endodontology have been opened up by the ability to deal with intracanalicular obstructions and ledges, and to close perforations successfully (Arnold, 2009).
Construction and Functions
Support Stands
There are three ways in which a dental microscope can be integrated into a dental operatory. In addition to the classic floor mount, wall-mounted or bench-mounted supports are available. Besides the need for an adequately strong supporting wall or countertop to support the device, key criteria for selection of the appropriate support include the space available and the desired degree of mobility. An absolute requirement is a vibration-free area when working at larger magnifications. Before finally purchasing, a technical inspection of the space by an expert is recommended.
Balance
Of special importance for the day-to-day, continuous use of the dental microscope is ease of mobility combined with a solid and stable support. The use of simpler, apparently cost-saving supports can lead to vibration/oscillation, delaying clinical treatment. It must be possible to manipulate the device with one hand in all planes of space, and so the mechanical or electromagnetic brakes must securely hold the microscope in the desired position.
18.1 The dental microscope
ProErgo, Zeiss (Oberkochen, Germany and Thornwood, NY, USA)
1 Floor stand
2 Swing arm with integrated computer controls and display monitor
3 Swing arm with integrated light source
4 Connection with electromagnetic brake
5 Optical head including:
– Eyepiece
– Tiltable tube
– Varioscope
– Video camera
6 Hand grips for:
– Light with brightness control
– Zoom, brake
– Documentation
Optics and Magnification
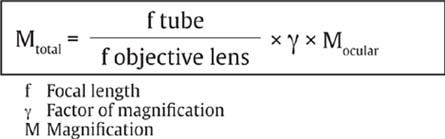
The optics of the dental microscope consist essentially of the Kepler tube (eyepiece and tube), the magnification changer, and the objective itself. The binocular optics permit spatial perception. The range of the focusing lens system varies according to manufacturer, especially at higher magnifications.
Light
The light originates from a separate source and travels through a fiberoptic to the optical parts of the device, and via a prism, coaxial to the optical axis. The light source may be a halogen or xenon lamp. These lamps are significantly different in terms of heat development, color of the light, temperature, and lifespan.
For endodontic practice, the xenon light source is used, with a daylight-like color, temperature of about 5800 K and a significantly higher light intensity of 420 klx in contrast with halogen lighting (which is about 100 klx).
Ergonomics
The use of a dental microscope permits the clinician to assume an upright posture that is less prone to cause fatigue, at a distance of more than 50 cm from the patient. For the treatment of maxillary teeth, the operator should be in the 12-o’clock position and for the mandible at the 8–9-o’clock position with respect to the reclining patient. With the patient’s mouth wide open, treatment can proceed under indirect vision using a rhodium-plated mirror. For lengthy procedures, the patient’s head should be stabilized using adjustable or inflatable airline-type pillows.
For vibration-free clinical work at higher magnifications, use of an operator chair with arm supports is absolutely necessary. Extended arm rests and a back support will guarantee a comfortable and relaxed position for the back muscles of the clinician. At the same time the dental assistant can keep a check on the stage of the clinical procedure on the monitor, and therefore provide optimum assistance. Other aids include microprobes, microabrasive ultrasonic instruments, and microsuction. Procedures of more than 2 hours’ duration can be easily carried out while continuing to maintain a high level of concentration.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses




