18
Orthodontic Treatment in Patients Requiring Orthognathic Surgical Procedures
Summary
Orthodontists and oral/maxillofacial surgeons have been working as a team for several decades to treat patients with significant skeletal jaw imbalances. As described in the quote below by Atul Gawande, advances in our technology and know-how have the potential to create better medical and dental outcomes for our patients, but they also create situations in which avoidable failures occur. Therefore, in the management of patients with skeletal jaw imbalances in the horizontal, vertical and/or transverse plane will benefit from the use of a checklist. While many of the steps listed in the checklist are well known by many providers, some of the steps listed below and described in this chapter will serve as a reminder of their importance and will encourage implementation of each of the steps by orthognathic teams and their staff.
The following checklist has been used by the author and his orthognathic teams to help patients not only achieve functional balance of the intricate stomatognathic system which is generally the primary goal of therapy, but also to provide esthetic improvement. When treating patients with complex jaw imbalances, orthognathic teams also strive to achieve functional balance, using reliable methods that achieve realistic, esthetic outcomes that are economically feasible. In addition, the orthodontist’s/surgeon’s teamwork also strives to provide a stable, satisfactory relationship that enhances the overall orofacial health of the patient. The acronym FRESH, described in step II, has been useful as a guide to specifically describe the major goals of orthodontic/orthognathic treatment for patients considering this option.
Thus, creating an orthognathic team, identifying specific treatment goals for each patient, and focusing on each step in the sequence of treatment (checklist), presented in this chapter, will help accomplish the desired outcome of orthognathic treatment on a routine basis.
Here then is our situation at the start of the twenty-first century: We have accumulated stupendous know-how. We have put it in the hands of the most highly trained, highly skilled, and hardworking people in our society. And, with it, they have indeed accomplished extraordinary things. Nonetheless, that know-how is often unmanageable. Avoidable failures are common and persistent, not to mention demoralizing and frustrating, across many fields – from medicine to finance, business to government. And the reason is increasingly more evident: the volume and complexity of what we know has exceeded our individual ability to deliver its benefits correctly, safely, or reliably. Knowledge has both saved us and burdened us.
That means we need a different strategy for overcoming failure: one that builds on experience and takes advantage of the knowledge people have but somehow also makes up for our inevitable human inadequacies. And there is such a strategy – though it will seem almost ridiculous in its simplicity, maybe even crazy to those of us who have spent years carefully developing ever more advanced skills and technologies.
It is the checklist.
Gawande (2010)
The Importance of the Sequence/Checklist
While most people think that a successful orthognathic treatment starts with an interview and an examination of the patient with skeletal jaw imbalance, the most important steps in providing treatment take place long before the surgeon or orthodontist meets the patient. The feedback loop sequence (checklist) described in Table 18.1 identifies eighteen significant steps that provide both the patient and their doctors with an excellent means of achieving the desired treatment outcome when there is a significant dentofacial imbalance.
Table 18.1 The preferred sequence of treatment for patients with significant dentofacial imbalances
| Stage | Description |
| Team preparation – Steps I and II | |
| I | Multiple provider team selection |
| • Orthodontist | |
| • Periodontist | |
| • Restorative dentist | |
| • Oral surgeon | |
| • Psychologist | |
| • Physical therapist | |
| II | Goal clarification for team members |
| • Functional occlusion | |
| • Reliable methods | |
| • Esthetics | |
| • Stability | |
| • Health | |
| Diagnosis and patient care – Steps III – X | |
| III | Clinical awareness of dentofacial deformity |
| • Self, general dentist, spouse/other | |
| IV | General assessment of patient |
| • A good candidate? | |
| • Periodontal status | |
| • Temporomandibular joint status | |
| V | Evaluation of preliminary records by the dental team |
| • Splint therapy for diagnosis of temporomandibular dysfunction, if needed | |
| VI | Completion of diagnostic records |
| • May include lifestyle assessment by clinical psychologist | |
| • May require more sophisticated temporomandibular joint studies | |
| VII | Multidisciplinary review of dentofacial problem based on patient records |
| VIII | Explanation to patient of available treatment options |
| • Optimal treatment plan | |
| • Alternatives | |
| • New, less invasive techniques | |
| IX | Consultation with patient and significant other by dental team providers |
| • Risk-benefit ratio | |
| • Fees and insurance coverage | |
| • Treatment time | |
| • Other concerns | |
| X | Patient acceptance of treatment plan |
| Presurgical – Steps XI and XII | |
| XI | Comprehensive orthodontic treatment (usually for 8–18 months before surgery) |
| • Orthodontic movement to decompensate tooth positions | |
| • Coordination of arches in anticipation of surgical repositioning | |
| • Alignment of teeth and correction of rotations | |
| XII | Presurgical re-evaluation records |
| • Complete records (models, panoramic radiograph, cephalogram, and photos) | |
| • Prediction tracing (detailed movements planned) | |
| • Model surgery (reviewed by orthodontist and surgeon) | |
| • Determination of specific fixation needs | |
| • Patient–spouse/other review with orthodontist and surgeon | |
| Postsurgical – Steps XIII – XVI | |
| XIII | Orthognathic surgery |
| • Simplest procedure or procedures to achieve professional goals and satisfy patient’s needs | |
| XIV | Postsurgical period |
| • Early: 2–3 weeks of fixation | |
| • Late: 3–8 weeks of fixation | |
| • Re-evaluation of surgical procedure | |
| • Review outcome with patient | |
| • Assess need for physical therapy | |
| XV | Evaluation and surgical stability |
| • Orthodontic finishing, occlusal adjustments, and retention procedures | |
| • Optimal continuation of contact with psychologist | |
| XVI | Post-treatment records |
| • 1 year post-treatment | |
| • Treatment evaluation by patient and orthodontist | |
| Feedback – Steps XVII – XVIII | |
| XVII | Re-evaluation of findings with dental team, especially oral surgeon and general dentist |
| • Problem solving | |
| • Re-evaluation of degree of success in achieving goals | |
| XVIII | Treatment experience to be used in management of future cases to enhance/refine checklist |
| • Re-evaluation of degree of success in achieving goals | |
| • Positive reinforcement | |
This chapter will highlight each of the steps needed to address every aspect of care for this special group of patients. In the sequence of treatment for patients with major dentofacial imbalances, Steps I, II, XVII, and XVIII are most often underemphasized. It is recommended that the reader review Steps I, II, XVII, and XVIII carefully, to optimize the checklist approach to the management of orthognathic patients and to improve the care as each orthognathic patient is treatment planned. In addition, Steps III through XVI are required to make sure that a uniform communication process is incorporated by each of the providers for all orthognathic patients; each step will be illustrated and reinforced through presentations of successfully treated case examples in this chapter. By following the general concepts stated in each step, the orthodontist, general dentist, and surgeon will spend the necessary time with the patient and be able to effectively address most of the patient’s pre- and postsurgical concerns. Using this checklist, the orthodontist can explain the sequence of treatment steps to the patient and the general dentist through the use of a treatment conference report. Orthognathic patients often experience increased anxiety and ask extra questions about the surgery; these questions need to be addressed, to help maintain their confidence and trust. The patient records in Figure 18.1 illustrate an adult patient with complex treatment requirements:
- Skeletal Class III with asymmetry of the mandible to the left
- Anterior crossbite
- Impacted maxillary left canine with retained deciduous canine
- Gingival deficiency in the lower anterior incisor area
- Missing maxillary right first molar (recently extracted)
- Patient’s attitude about treatment and the longevity of her dentition (asked about the option of dentures during her initial interview).
Figure 18.1 (a–c) Pretreatment facial photographs. (d–f) Pretreatment intraoral photographs – note thin gingival tissue in lower anterior area. Retained deciduous maxillary left canine and midline asymmetry. (g) Pretreatment panoramic radiograph. (h) Pretreatment cephalometric radiograph with Bolton template overlay. (Note the skeletal Class III malocclusion with significant mandibular excess.)

Due to the complexity of the treatment planning for the patient seen in Figure 18.1, and the other patients with similar skeletal jaw imbalances, an individualized treatment plan is necessary. This will help to detail the sequence of the steps, so that all of the interdisciplinary providers and the patient understand the process, the timetable, and the specific sequence of steps (Figure 18.2).
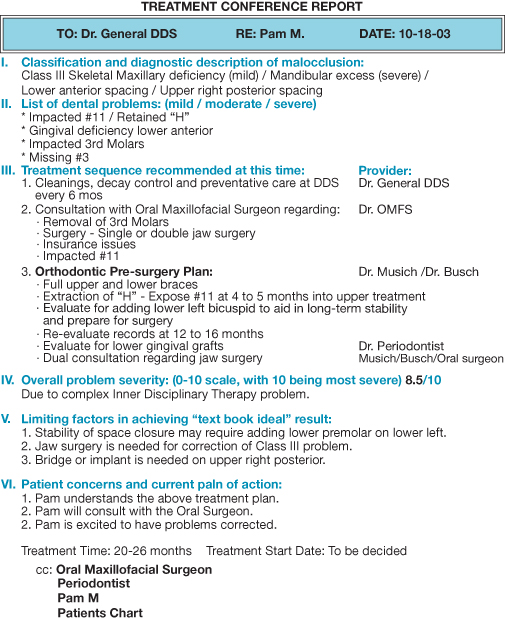
Figure 18.2 The Treatment Conference Report. For patients with interdisciplinary therapy requirements it is important to have the steps in the plan summarized for each of the providers and for the patient. The Treatment Conference Report provides the ‘roadmap’ for treatment and the approximate timing of the steps.
The following explanations of each step in the sequence detail the rationales and strategies for providing careful treatment planning for patients with complex treatment requirements.
Team Preparation – Steps I and II
Step I: Multiple Provider Team Selection (Table 18.1)
- Orthodontist
- Periodontist
- Restorative dentist
- Oral surgeon
- Psychologist
- Physical therapist
Development of the interdisciplinary team is a deliberate step that requires judicious interaction (sometimes ‘interviews’) with other potential members of the team. The interaction can occur within continuing education professional study clubs or might evolve from the discussions of patient treatment planning (Box 18.1). As stated by Turpin (2010): ‘Talking with current members of successful study clubs, I found that they share many traits. Historically, most study clubs had rather modest beginnings, but, with strong leadership, they can evolve into large organizations with lofty goals. No matter the size or the location, the secret of orthodontic study clubs is clear to me: you get out of them what you put into them.’ Study clubs that include both orthodontists and surgeons as members, can develop effective interactions and an accelerated awareness of new, evidence-based insights regarding the type of care that is best suited for their patients with skeletal jaw imbalances.
Box 18.1 Basic goals for interdisciplinary dentofacial teams
- Philosophy of treatment consistent to achieve desired goals
- Ability to recognize, prioritize, and address the patient’s chief concern
- High-quality communication process between the doctors and treatment coordinators
- Logistic availability of office; office hours; method of doctor-to-doctor communication
- Compatible insurance coverage (in network – out of network)
- Patient’s comfort and trust of the providers within the referral loop
An excellent book by Roblee (1994), Interdisciplinary Dentofacial Therapy: A Comprehensive Approach to Optimal Patient Care, advanced the concept of interdisciplinary dentofacial therapy and provided a strategy for developing predictable outcomes for patients with complex dentofacial situations:
The concept of Interdisciplinary Dentofacial Therapy (IDT) was developed to maximize treatment results by optimally synergizing the knowledge, skills, and experience of all the disciplines in dentistry and its associated fields, while minimizing the frustrating and problematic shortcomings typically associated with working as a team.
Roblee et al. (2009)
This book is recommended reading for any IDT team that is in its formative stages. Roblee et al. (2009) emphasized two key elements of the teamwork needed to consistently produce high quality results:
Regimental sequencing to insure that every procedure is performed in the order closest to ideal throughout the entire interdisciplinary process.
Extensive communication between providers, to optimize all aspects of IDT.
The dentist will refer patients (Figure 18.3) with skeletal malocclusion to the orthodontist, but only if he/she is confident that the patient will receive appropriate state-of-the-art care. The orthodontist must then select surgeons who are experienced and well-trained in the spectrum of orthognathic procedures. A periodontist, psychologist, and physical therapist may become key team members in selected cases, as they may be required for certain types of orthognathic situations. With the advent of rigid fixation, patients seem to have less of a need for psychological intervention as the post-operative phase of depression has been less of a problem (Dolce et al., 2002).
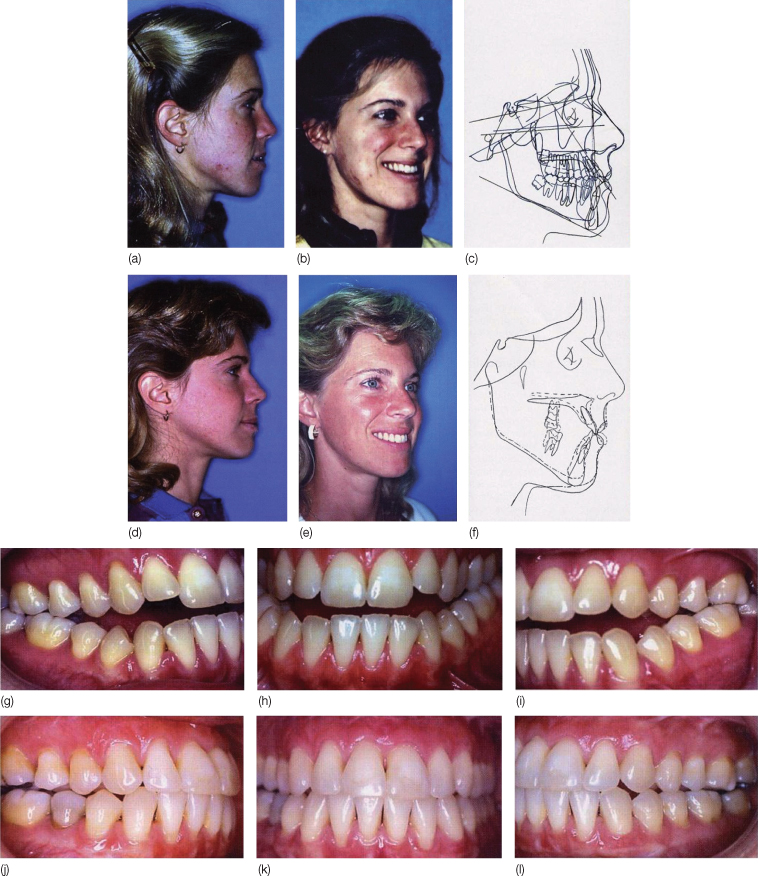
Figure 18.3 Patient with Class III with open bite. (a) Pretreatment profile. (b) Pretreatment three-quarter smile photograph. (c) Pretreatment tracing of cephalogram with Bolton template superimposed to provide a template-guided treatment plan. (d) Post-treatment profile. (e) Post-treatment three-quarter smile photograph after maxillomandibular surgery and orthodontics, and periodontal grafting to improve her overall dental health and functional environment. (f) Cephalometric superimposition of before and after tracings. (g–i) Pretreatment intraoral photographs. (j–l) Post-treatment intraoral photographs.
However, there are patients with profound self-esteem issues, for whom presurgical counseling may better prepare them for the changes that may occur during the orthodontic/orthognathic treatment. This counseling may also help patients develop realistic expectations of the treatment outcome (Figure 18.4).
Figure 18.4 Patient with significant mandibular deficiency and chin deficiency. (a) Presurgical facial profile of (b) Presurgical three-quarter smile. (c) Postsurgical facial profile of same patient following orthodontics and bimaxillary surgery. (d) Postsurgical three-quarter smile of same patient – patient had mandibular advancement and maxillary impaction and genioplasty.

Step II: Goal Clarification for Team Members (Box 18.2)
- F unction (optimal)
- R eliable/realistic
- E sthetic/economic
- S tability/satisfaction
- H ealth – dental/mental
Box 18.2 F.R.E.S.H
- Function – The fundamental goal of improving occlusal relationship is paramount; it is desirable to establish optimal gnathological parameters for the stomatognathic system (incisal guidance, canine rise, and balanced, bilateral posterior occlusal support), temporomandibular joint (TMJ) health, and TMJ stability without symptoms.
- Reliable – Methods of treatment that have been scientifically verified to be highly successful in achieving correction of skeletal imbalances, and that are of lower risks than other available procedures for the improvement of a given condition, are utilized. Recent examples of techniques that have proven their reliability include rigid fixation approaches; jaw surgery to resolve sleep apnea; and use of micro-screws as anchorage-to improve the range of nonsurgical treatment.
- Realistic – The plan of treatment has a high probability of correcting the patient’s chief concern, and offers the best option to achieve an outcome with a high probability of meeting both the patient’s and doctor’s expectations.
- Esthetics – Issues of esthetics relate to both dental and facial appearance; facial esthetics requires assessment of both the profile and frontal views, to achieve soft tissue balance, as well as optimal symmetry. The facial balance should be present both statically and dynamically in speech and during facial expression, especially in smiling. The role of the ‘aging process of the face’ should also be integrated into the treatment planning process, especially when considering camouflage options.
- Economic – The cost of the proposed treatment requires consideration because most patients have a well-defined budget for their medical and dental needs. With limited insurance for orthodontic care, and reduced coverage for orthognathic surgical procedures, financial considerations frequently interfere with the optimal combined orthognathic/orthodontic treatment plan.
- Stability – A key part of the treatment outcome is ending with jaw and tooth positions that are reasonably stable. There are several dimensions to stability, and there are many adult orthodontic problems that require fixed retention to assure stability, especially of the lower and upper incisors.
- Satisfaction – Achieving both patient and provider satisfaction is important. This usually occurs when there is open discussion, prior to treatment, about the goals that both the doctor and the patient are striving to achieve in this individual situation. This would include a frank discussion from the doctor about the ‘downside’ or ‘limits’ of the accepted plan. This is particularly true in patients who have a skeletal diagnosis and are being considered for camouflage therapy when skeletal correction is more ideal. The use of visualized treatment objectives and computerized predictions can assist the patient and the providers.
The members of the provider team should share similar concepts of treatment goals. For example, functional occlusal goals, stability of outcome, and dental and facial esthetic goals can mean different things to different professionals. Periodic group meetings oriented to individual case analysis offer an opportunity for team members to discuss their concepts of the treatment goals that apply to the individual patient, and to establish consistency in pursuing treatment and treatment goals.
Borderline Surgery Class II – Case Report (Figure 18.5)
Sometimes ‘borderline’ surgical patients are referred to oral and maxillofacial surgeons (OMS) to enhance informed consent and to help the patient develop better insights into the options of their care. There is value in considering all treatment goals as a group, using the acronym FRESH.
- Interdisciplinary consultation can improve dialog between the provider and the patient, so that prioritization becomes clearer to each. When one goal or several are prioritized over others, careful consideration should be given to which goals are being de-prioritized, so that the outcome of treatment is not undermined. For example, if the goal of economic treatment becomes a priority when the stability of the outcome is not factored into the treatment plan, the results will fail when the equilibrium requirements of the stomatognathic system cause the malocclusion to reoccur.
- Interdisciplinary consultation allows restatement of the conditions of the disharmony that can successfully be treated and the ones that cannot.
- The use of therapeutic diagnosis with functional appliances is appropriately presented (Figure 18.6)
- Medicolegal issues will be less likely with this sort of full disclosure (Wheeler, 1992; Jerrold, 2000).
Figure 18.5 (a–c) Pretreatment intraoral photographs showing a Class II malocclusion with maxillary protrusion, with upper premolars missing, crowded lower anteriors and a significant overjet. (d–f) Post-treatment intraoral photographs with correction of overjet, crowding, and Class I canine relationship. (g,h) Progress intraoral photographs showing reversal of arch collapse due to early extraction of the mandibular right first molar. Longstanding arch collapse created the appearance of a skeletal malocclusion, when much of the overjet was a result of the collapsed mandibular arch, drifting of the right buccal segment, and collapsed lower incisor area secondary to lip entrapment. (i) Pretreatment cephalometric tracing; initial treatment plan by first orthodontist suggested a surgical approach to resolve the overjet. (j) Pretreatment periapical radiograph showing the collapsed area at the mandibular right first molar. (k) Progress panoramic radiograph showing space opening at mandibular right first molar that also advanced the lower anteriors, which reduced the overjet without surgical intervention. The space at the missing mandibular right first molar was stabilized with a fixed restoration.

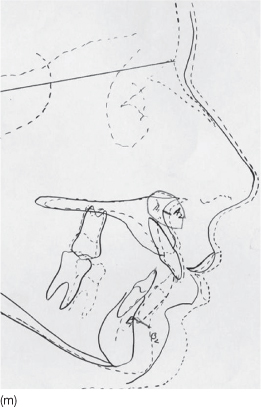
Figure 18.6 (a–c) Pretreatment intraoral photographs. (d–f) Posttreatment intraoral photographs. (g) Pretreatment panoramic radiograph. (h) Posttreatment panoramic radiograph. (i,j) Pretreatment facial photographs. (k,l) Post-treatment facial photographs. (m) Pretreatment and posttreatment cephalometric tracings superimposed, illustrating excellent growth response of the mandible through the use of the mandibular anterior repositioning appliance (MARA).

In addition to the above points, during the past decade, the treatment paradigm has changed with the effectiveness of newly developed modalities, such as the use of temporary anchorage devices (TADs) (Xun et al., 2007), surgically facilitated orthodontic treatment (SFOT) (Roblee et al., 2009), and periodontal accelerated orthodontic procedures (PAOP) (Murphy et al., 2009). As a result, there are several more treatment planning options available for the patient with borderline surgical problems.
Diagnosis and Patient Care – Steps III–X
Step III: Clinical Awareness of Dentofacial Deformity (Figure 18.7)
- Self – through awareness of symptoms or intrinsic esthetic issues
- General dentist – through diagnostic process or increase of subjective and objective symptoms
- Spouse/other – through personal research and support
- Friend – who might have experienced an orthognathic correction and encourages the patient to pursue correction
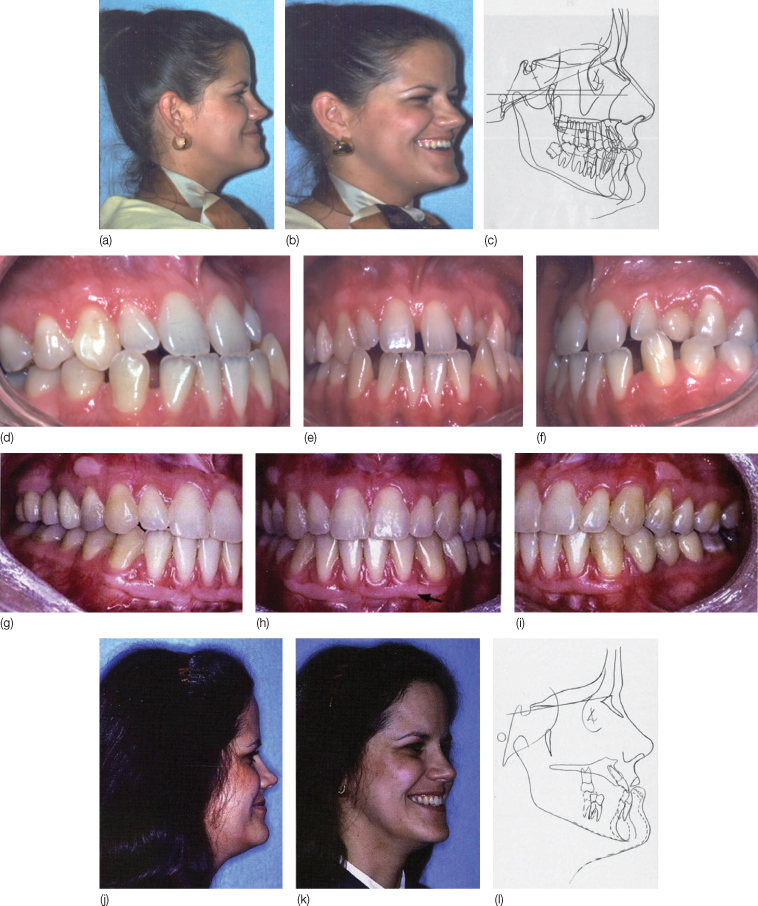
Figure 18.7 (a) Pretreatment facial photograph. (b) Pretreatment three-quarter smile photograph. (c) Template-guided diagnosis with Bolton template superimposed on pretreatment cephalometric tracing of patient. (d–f) Pretreatment intraoral photographs. (g–i) Post-treatment intraoral photographs showing successful outcome of interdisciplinary dentofacial therapy, as illustrated in Figure 18.2. (j) Post-treatment facial profile photograph. (k) Post-treatment three-quarter smile photographs. (l) Superimposition of pretreatment tracing with post-treatment skeletal change demonstrated.
Patients learn about their dentofacial imbalance through a variety of ways. Frequently, awareness of the problem starts with early diagnosis at the family dentist’s practice. Some patients exhibit disproportionate growth patterns that will not show up until early adulthood. For example, the patient in Figure 18.8 only became aware of the need for orthognathic surgery after a robust adolescent growth spurt, which occurred after two years of full orthodontic treatment. Other factors that lead patients to consider orthognathic procedures are facial and/or jaw trauma, pain due to dysfunctional TMJ apparatus, inability to chew and digest food, periodontal breakdown, and combinations of the above conditions, frequently augmented by the patient’s esthetic concerns. Tables 18.2–18.4 show the prevalence of skeletal jaw imbalances that would be significant enough to require surgery.
Table 18.2 Estimated prevalence of mandibular deficiency severe enough to indicate surgery
| Percentage | Number | |
| Prevalence of skeletal Class II malocclusion | 10a | 31 000 000 |
| At appropriate age for surgical treatment | 68 | 21 125 000 |
| Severe enough to warrant surgery | 5 | 1 056 250 |
| Mandibular advancement | 70 | 739,375 |
| Maxillary setback | 10 | 105 625 |
| Both | 20 | 211 250 |
| New patients added to the population yearlyb | 0.5 | 21 250 |
aAssuming US population of 325 million.
bAssuming 4.25 million live births per year.
Table 18.3 Estimated prevalence of Class III problems severe enough to indicate surgery
| Percentage | Number | |
| Prevalence of skeletal Class III malocclusion | 0.6a | 1 950 000 |
| At appropriate age for surgical treatment | 65 | 1 267 500 |
| Severe enough to warrant surgery | 33 | 418 275 |
| Mandibular setback | 45 | 188 224 |
| Maxillary advancement | 35 | 146 396 |
| Both | 20 | 83 655 |
| New patients added to the population yearlyb | 0.2 | 8 500 |
aAssuming US population of 325 million.
bAssuming 4.25 million live births per year.
Table 18.4 Estimated prevalence of long-face problems severe enough to indicate surgery
| Percentage | Number | |
| Prevalence of severe anterior open bite | 0.6a | 1 950 000 |
| At appropriate age for surgical treatment | 65 | 1 267 500 |
| Severe enough to warrant surgery (superior repositioning of the maxilla) | 25 | 316 875 |
| New patients added to the population yearlyb | 0.2 | 6375 |
aAssuming US population of 325 million.
bAssuming 4.25 million live births per year.
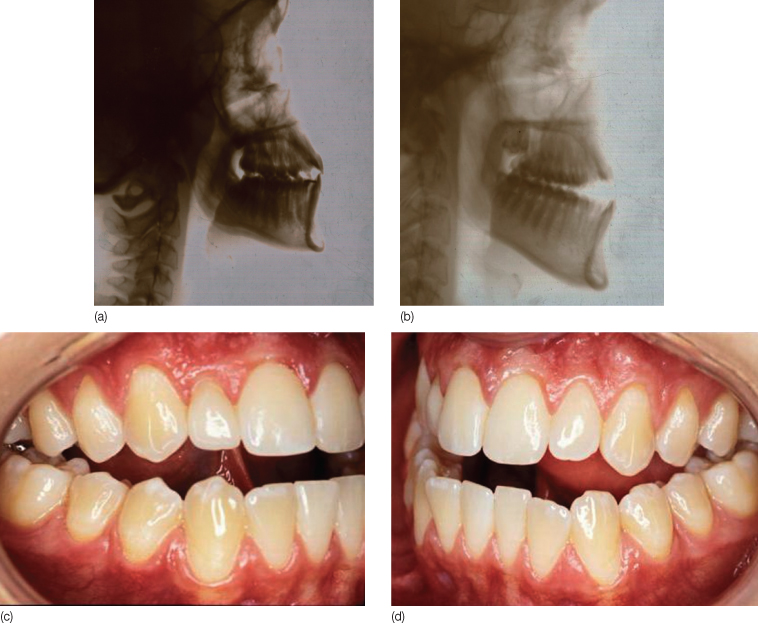
Figure 18.8 (a) Cephalogram of post-orthodontic transfer patient at age 14.5. Note bonded lingual arch in place. (b) Cephalogram at time of new records in new office following a robust adolescent male growth spurt, illustrating significant differential growth of maxilla and mandible which ultimately required orthodontic retreatment and bimaxillary surgery. (c,d) Intraoral photographs showing the degree of Class III malocclusion and the anterior open bite.
Step IV: General Assessment of a Patient
For all patients, periodontal diagnosis requires the attention of the orthodontist. One of the most overlooked considerations in the management of the adult patient considering combined orthodontic and orthognathic treatment is the impact of patient susceptibility to periodontal disease, coupled with the pre-existing habit of smoking. Up until 2003, many orthodontists did not include a question on the adult medical history form asking if the patient used tobacco products, nor did the form include a follow-up question about the frequency of tobacco use. In 1996, the American Academy of Periodontists published a position paper titled ‘Tobacco use and the periodontal patient’ (Ryder, 1996). In this well-researched paper, the American Academy of Periodontists referenced 97 published papers, which verify the following:
Clinical and epidemiological studies support the concept that tobacco use is an important variable affecting the prevalence and progression of periodontal diseases, such as adult periodontitis, refractory periodontitis, and ANUG [acute necrotizing ulcerative/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


