18
Geriatric Health and Functional Issues
I. Background
Aging is a natural consequence of life and involves anatomical, biochemical, and physiological alterations in every system. These changes present with a high degree of heterogeneity, which challenge health-care providers to differentiate signs of normal aging from disease. Common age-related changes and age-related disorders of vision, hearing, mobility, and cognition will be discussed in this chapter. These health concerns often cause disability and vulnerability, and impact one’s quality of life. Age-related visual and hearing impairments decrease one’s ability to complete their activities of daily living (ADLs) and communicate with others, and can lead to isolation and depression.1
Description of Disease/Condition
Age-Related Visual Changes
The most common causes of vision impairment that lead to blindness are age-related macular degeneration (AMD), glaucoma, cataract, and diabetic retinopathy.
Presbyopia is the loss of visual acuity due to a progressive change in the optic compartment. Presbyopia presents with difficulties in the ability to focus at close range, read small print, see well in dim lighting, and differentiate colors. It is not a disease. Most with presbyopia do not become completely blind, but experience partial/moderate loss of vision and may need to develop new skills to remain self-reliant.
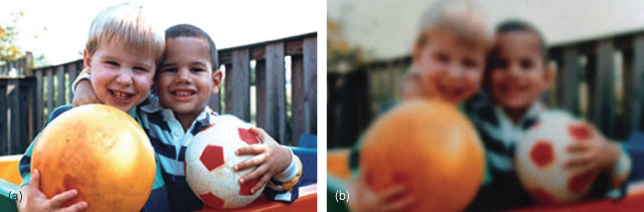
Cataract is a clouding or opacity of the lens of the eye that can range from a small, localized area to a diffuse loss of transparency. Most are related to aging. By age 80, >50% of Americans have a cataract or have had cataract surgery. The most common symptoms include cloudy or blurry vision, colors seem faded, glare from headlights and sunlight, poor night vision, double vision, or multiple images in one eye. See Fig. 18.1.
Figure 18.1 (a) Normal vision. (b) The same scene as viewed by a person with cataract. From the National Eye Institute, NIH, USDHHS. Facts about Cataract. September 2009.
Adapted from Don’t Lose Sight of Cataract (NIH Publication No. 94-3463) and Cataract: What You Should Know (NIH Publication No. 03-201). Available at: http://www.nei.nih.gov/health/cataract/cataract_facts.asp.
AMD is due to the abnormal vascularization under the retina, which causes progressive damage to the macula, the central part of the retina that allows fine details to be visible.2 AMD leads to loss of central vision, which is needed for reading, driving, recognizing faces, and remaining independent. Peripheral vision is usually retained.
- Two forms:
- Dry (atrophic) AMD accounting for 90% of cases.
- Wet (neovascular/exudate) AMD is a more severe form, causing acute pain.
Glaucoma comprises a group of disorders characterized by optic nerve damage and visual field loss. It is chronic, progressive, and degenerative, usually occurs insidiously and is asymptomatic in early stages. Vision loss is caused by a progressive loss of optic nerve fibers. If not treated, it can cause irreversible blindness.3 Those with glaucoma may have elevated intraocular pressure.4
- Two main types:
- Open-angle (chronic) glaucoma—90% of cases
- Characterized by a clinical triad:
(1) elevated intraocular pressure;(2) development of optic nerve atrophy; and(3) loss of peripheral field of vision.3
- Characterized by a clinical triad:
- Angle-closure (acute) glaucoma—10% of all cases
- Causes a quick, severe, and painful rise in intraocular pressure.
- Treatment must occur quickly as there is an increased risk of involvement of the second eye.
- Open-angle (chronic) glaucoma—90% of cases
Diabetic retinopathy is a vascular complication of diabetes caused by poor blood glucose control. Diabetic retinopathy-related eye changes include micro-aneurysms, hemorrhages, hard and soft exudates, proliferation of newly formed vessels, retinal detachment, and the development of secondary glaucoma.5 Early treatment can prevent blindness.
Age-Related Hearing Loss
Age-related hearing loss or presbycusis is a progressive sensorineural hearing loss that may involve both peripheral reduction in hearing threshold sensitivity and impairment of central processing. It is usually symmetric, though may have significant variation between ears. Age-related hearing loss often goes undetected and untreated, and has caused some with hearing loss to be wrongly labeled as “confused,” “nonresponsive,” or “uncooperative.” Hearing-impaired older adults may withdraw from social situations to avoid frustration and embarrassment, increasing their risk of social isolation, depression, and declining physical functioning—ultimately decreasing their quality of life.6
Mobility Limitations
Osteoarthritis (OA) or degenerative joint disease is a progressive pathological change of the hyaline cartilage and underlying bone of a joint, and is the most common type of arthritis. Joints most commonly affected are knees, hips, hands (Heberden’s nodes a re a visible sign, see Fig. 18.2), and spine. It is not caused simply by wear and tear. Presence of OA in weight-bearing joints has the greatest clinical impact. Disease onset is gradual and usually begins after the age of 40.
Figure 18.2 Heberden’s nodes in osteoarthritic hand.

Cognitive Impairment/Dementias
The Role of Cognition in Older Adults
As people age, they are at an increased risk of having cognitive and memory problems, or cognitive aging. The cognitive functions most affected by age are attention and memory; however, age-related changes are not uniform across all cognitive domains7 or across individuals. There is enormous variability in cognitive decline seen in older adults. Memory loss is not inevitable as people have lived to extreme old age without severe memory loss.8
The lack of cognitive health can have profound implications for a person’s health and well being. Limitations in one’s ability to manage medications, medical conditions, or to live safely are of particular concern when a person is experiencing a cognitive impairment. Poor cognitive health leads to increased vulnerability to disease, injury, malnutrition, crime, abuse, and eventually a loss of independence.
Cognitive declines range from mild cognitive impairment (MCI) to Alzheimer’s disease (AD) and other dementias. Studies of brain abnormalities have recognized that AD, Lewy body disease, Huntington’s disease, frontotemporal dementia, amyotrophic lateral sclerosis, Parkinson’s disease, and Creutzfeldt–Jakob disease have similar clinical symptoms, including memory loss, movement problems, and sleep–wake disorders. Memory impairment can also be the result of cerebrovascular disease, hydrocephalus, hypothyroidism, vitamin B12 deficiency, central nervous system infection, a cognitive disorder related to human immunodeficiency virus infection, adverse effects of prescribed medications, substance abuse, and cancer.9 See also Chapter 14 “Neurological Disorders.”
Cognitive impairments adversely affect the person with the disease and their family, caregivers, and friends. Obtaining an early diagnosis of a cognitive impairment can make a significant difference in the lives of patients and their families; however, it is relatively rare that a cognitive disorder is diagnosed early in the course of the disease.10
Mild Cognitive Impairment (MCI)
MCI is a syndrome of having a cognitive decline greater than expected for an individual’s age and education level that does not interfere notably with ADLs. MCI does not meet the criteria for dementia. MCI criteria include a cognitive impairment, essentially normal functional activities, abnormal memory function for age and education (1–2 standard deviations), and absence of dementia.11
MCI is a risk state for AD, with the rate of conversion ranging from 10% to 15% per year, due to differences in assessment procedures, sample composition, and definition of cases. Early identification of MCI can lead to secondary prevention by controlling risk factors.12
There are two primary types of MCI:
- Has a high risk of progression to dementia particularly that of an Alzheimer’s type;13 averages 12% per year.
- Neuropathology is typical of AD.
- May be associated with cerebrovascular disease, frontotemporal dementias, or have no specific pathology.
- Does not progress to AD.
Dementia
Dementia is a syndrome characterized by progressive deterioration in multiple cognitive domains, severe enough to interfere with daily functioning. Dementia is the umbrella term used to describe cognitive impairment.
- It affects one’s memory, understanding and use of words, ability to identify objects, and ability to comprehend and act on messages.
- It is a principal cause of disability and institutionalization of older adults.
- Later stage present with total dependence on others.
Alzheimer’s Disease (AD)
AD is a progressive, degenerative, neurological disorder that manifests by loss of intellectual functions, including memory, language, visuospatial skills, behavioral changes, problem-solving ability, and abstract reasoning.14 Early-onset AD, a rare disease inherited in an autosomal dominant pattern, occurs between 30 and 50 years of age. Late-onset AD typically affects those ≥65 years. AD is the most common type (60–80%) of dementia in the United States.
- Clinical hallmarks are progressive impairment in memory, judgment, decision making, orientation to physical surroundings, and language.
Disease onset is insidious; manifestations evolve over a period of years from mildly impaired to severe cognitive loss. Progression of the disease is inevitable and may include plateaus of 1–2 years.9 Table 18.1 describes the seven stages of Alzheimer’s.
Table 18.1. Seven Stages of Alzheimer’s
| Stage 1: | No impairment (normal function) The person does not experience any memory problems. An interview with a medical professional does not show any evidence of symptoms of dementia. |
| Stage 2: | Very mild cognitive decline (may be normal age-related changes or earliest signs of Alzheimer’s disease) The person may feel as if he or she is having memory lapses—forgetting familiar words or the location of everyday objects. But no symptoms of dementia can be detected during a medical examination or by friends, family, or coworkers. |
| Stage 3: | Mild cognitive decline (early-stage Alzheimer’s can be diagnosed in some, but not all, individuals with these symptoms) Friends, family, or coworkers begin to notice difficulties. During a detailed medical interview, doctors may be able to detect problems in memory or concentration. Common stage 3 difficulties include:
|
| Stage 4: | Moderate cognitive decline (mild or early-stage Alzheimer’s disease) At this point, a careful medical interview should be able to detect clear-cut symptoms in several areas:
|
| Stage 5: | Moderately severe cognitive decline (moderate or mid-stage Alzheimer’s disease) Gaps in memory and thinking are noticeable, and individuals begin to need help with day-to-day activities. At this stage, those with Alzheimer’s may:
|
| Stage 6: | Severe cognitive decline (moderately severe or mid-stage Alzheimer’s disease) Memory continues to worsen, personality changes may take place, and individuals need extensive help with daily activities. At this stage, individuals may:
|
| Stage 7: | Very severe cognitive decline (severe or late-stage Alzheimer’s disease) In the final stage of this disease, individuals lose the ability to respond to their environment, to carry on a conversation and, eventually, to control movement. They may still say words or phrases. At this stage, individuals need help with much of their daily personal care, including eating or using the toilet. They may also lose the ability to smile, to sit without support, and to hold their heads up. Reflexes become abnormal. Muscles grow rigid. Swallowing impaired. |
It is difficult to place a person with Alzheimer’s in a specific stage as stages may overlap.
Permission granted: “Alzheimer’s Association 2011. All rights reserved.”
Pathogenesis/Etiology
Age-Related Visual Changes
Age-related eye changes include the following:
- Retina: Colors appear less bright with contrast between colors less noticeable. Blue, black, and green colors appear faded and difficult to differentiate.
- Decreased visual field, around 1–3 degrees per decade of life; individuals 70–80 years have lost between 20 and 30 degrees of peripheral vision.
- Pupil gets smaller and pupil dilation decreases with age, resulting in less light reaching the retina.
- Ocular muscles weaken, with pupil and decreased elasticity of lens causing a delay in dark adaptation from bright areas, and may contribute to night vision problems.15
- Cornea and pupil are less responsive, resulting in the need for more light to see clearly.
- Lens yellows and becomes less clear, so light is scattered, which reduces color vision and contrast sensitivity.
- Lens hardens, which leads to decreased ability to accommodate.
- Those ≥80 years need three to six times more light for comfortable reading than those in their twenties.
Cataract is an age-related condition.
AMD: Etiology is unknown.
- Dry AMD: Light-sensitive cells in macula break down causing distorted and blurred central vision with blind spots in advanced cases.
- May precipitate the development of wet AMD.
- Wet AMD: A result of abnormal blood vessels growing under the retina and leaking blood and fluid and damaging the macula.
Glaucoma
- Open Angle: Unknown etiology.
- Angle Closure: Occurs when the aqueous humor fluid is blocked.
Diabetic retinopathy: Vision loss occurs through retinal detachment, vitreous hemorrhage, neovascular glaucoma, and macular edema or capillary nonperfusion.5
Age-Related Hearing Loss
- Results from peripheral cochlear defects and a defect in central auditory processing, but etiology is unknown. May be due to degenerative structural changes in the inner ear, genetic factors, or exposure to loud noises over a long period of time.
- Usually occurs slowly, affecting hearing of high tones (1000–8000 Hz range); thus, male voices are easier to hear than female voices.
Mobility Limitations
OA: Unknown etiology; classified as idiopathic and secondary (traumatic, congenital, or due to other causes).
Cognitive Impairment/Dementias
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


