Chapter 17
Problem Solving in the Management of Teeth With Subgingival Carious and Fractured Margins Including Radicular Defects
Problem-solving issues and challenges in managing compromises in sound tooth margins and radicular defects addressed in this chapter are:
“Once the biologic width of the supporting periodontal attachment apparatus has been severely violated, more extensive procedures are often necessary to manage compromised root structure and supporting bone.”< ?xml:namespace prefix = "mbp" />
Preserving the natural dentition in symptom-free clinical function is a major goal of dentistry and its specific disciplines. Prosthetic dentistry has provided fixed and removable substitutes for teeth that have been lost, and the advent of implant dentistry has brought about a new concept, replacement of the natural dentition. While the development of implantology has been a marvelous addition to the practice of dentistry and has enhanced patient well-being,
In this chapter, surgical procedures will be presented that can be used effectively to retain teeth with a variety of complications in addition to pulpal disease. The most common problems encountered are clinical crowns with subgingival carious or fractured margins and insufficient tooth structure to retain a restoration. In many of these cases, crown lengthening is an ideal solution. Exposure of sound tooth structure can make restoring certain types of compromised teeth a routine procedure, enhancing not only the restoration of the tooth but the biologic widths of the supporting periodontium. The basic techniques of this surgical intervention can be extended to the management of other endodontic problems such as resorption and perforation defects.
Normal Periodontium in Relation to Surgical Treatment Planning
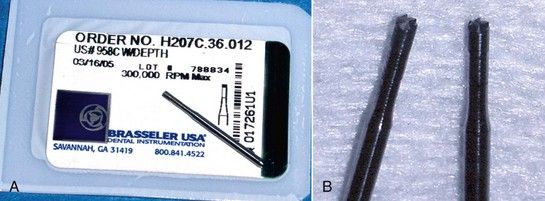
Prior to considering periodontal surgical procedures, a review of the normal anatomy of these tissues is essential. A discussion of average sulcus depth was included at the beginning of
FIGURE 17-1 A, Normal periodontium. B, Histologic section through normal periodontium (H&E stain ×10).
The width of the attached gingiva varies from 1 to 9 mm,

FIGURE 17-2 A, Attached gingiva of normal, ample width. B, Width of attached gingiva in this maxillary right premolar area is 1 mm or less.
The contours of the normal alveolar bone are also of great significance. Most often, surgical crown lengthening cannot be achieved without removing some crestal bone. Postoperatively, the measure of success is not only increased clinical crown length but also restoration of a normal periodontium circumferentially. In recontouring bone, the clinician should reproduce or create the contours of normal periodontium. Except in the mandibular second and third molar areas, the buccal and lingual plates are usually fairly thin throughout the dentition (
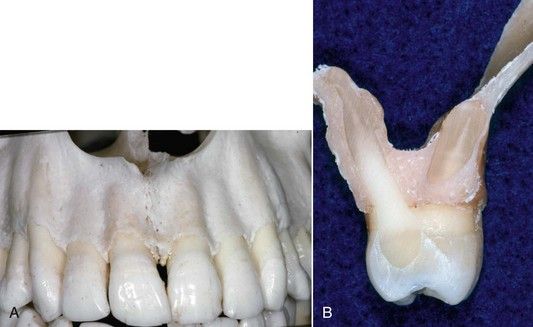
FIGURE 17-3 A, Labial plate of bone is normally thin. B, Cross-section of maxilla in the first molar area, showing buccal and palatal plates of bone.
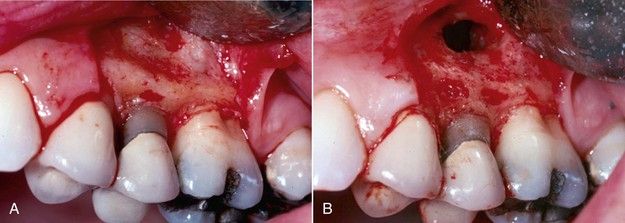
FIGURE 17-4 A, Excessive width of buccal plate of bone. B, Recontoured buccal plate during periapical surgery procedure.

CLINICAL PROBLEM
Problem
Can the interproximal bone throughout the mouth be recontoured using a standardized technique?
Solution
No, because there is a significant difference between the interproximal contours of the bone between the posterior teeth and the contours found between the anterior teeth. The normal contour between posterior teeth is flat buccolingually (

FIGURE 17-7 A, Periodontal surgery for severe chronic periodontitis. B, Following osseous recontouring and pocket elimination. Note ramping of buccal plate into interproximal spaces.
(Courtesy Dr. Curtis Wade.)

FIGURE 17-8 Normal interproximal anatomy of bone in the anterior dentition is characterized as a crest.

Indications for Crown Lengthening
There are multiple considerations in which crown lengthening can and should be considered in the treatment planning for tooth retention.
Convenience of Tooth Isolation
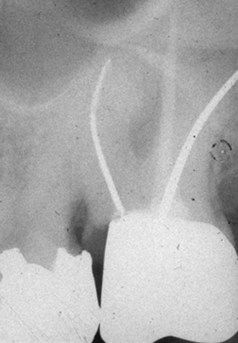
Before arriving at crown lengthening as the treatment of choice, a discussion of common alternatives is indicated. Most teeth with significant carious lesions can be isolated without crown lengthening. One simple solution is to place the dental dam clamp directly on the gingiva and complete the root canal treatment (

FIGURE 17-11 Placing dental dam clamp directly on gingival margin does not address subgingival caries or restorability following root canal treatment.

FIGURE 17-12 Dental dam sealers are effective, but restorability of the deep fracture in this case remains a problem.
Many clinicians favor complete restoration of the endodontically involved tooth. Access is then made through the new restoration (
Establishing Increased Clinical Crown for the “Ferrule Effect”
This key restorative goal is discussed in detail in
Preventing Restorative Failure
Lack of a ferrule also can focus excessive occlusal forces on the post and core and eventually cause the post to loosen or fracture
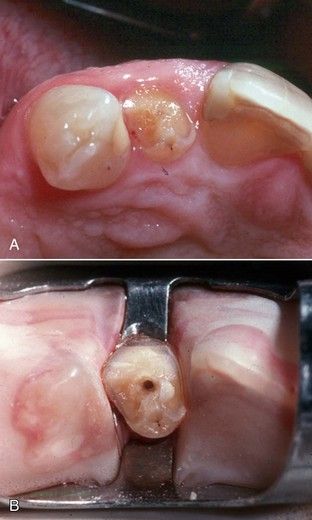
Avoiding Marginal Problems With Restorations
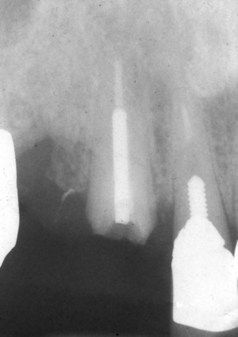
Excavation of caries below the free gingival margin or a fracture requires subgingival margin placement, or impressions and restorations will be faulty (
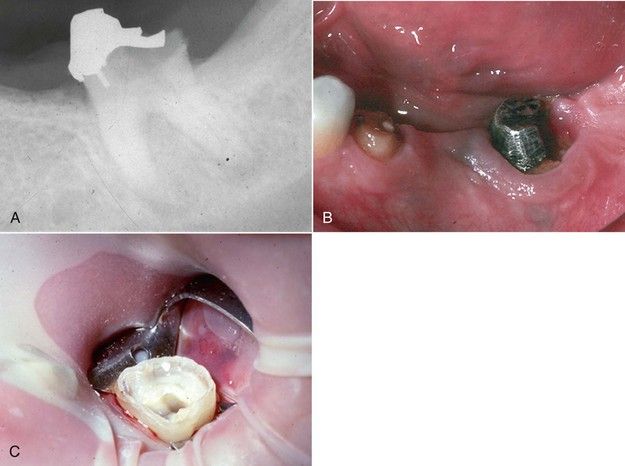
Managing Deep Fractures
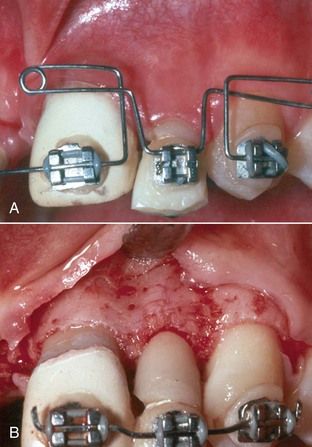
Many deep subgingival fractures cannot be restored adequately, and over time the tooth may develop periodontal complications. Crown lengthening addresses such complications prior to restoration, resulting in a routine procedure with an excellent, uncomplicated prognosis (
Location of Obscure Root Canal Orifices
A specific endodontic indication is the case in which a coronal fracture has resulted in hyperplasia of the marginal gingiva, obscuring the location of a canal orifice. Often, if these fractures were present as mere cracks for any length of time, narrowing and calcification of adjacent root canal orifices occurred secondary to long-term bacterial ingress and pulp tissue irritation. After crown lengthening, orientation is greatly improved, enhancing access preparation and canal orifice location (
Following Orthodontic Extrusion of Teeth or Roots
The techniques for orthodontic extrusion are discussed in previous editions of this text and in the orthodontic literature. The periodontal consequence of extrusion is coronal movement of the attachment.
Potential Contraindications for Crown Lengthening
There are both general and local considerations in which crown lengthening may not be considered in the treatment planning for tooth retention.
Medical Status
Generally, the medical status and current medications prescribed for the patient are reviewed for the same conditions that would contraindicate any surgical procedure. The reader is referred to other texts on oral surgery for a discussion of these issues.
Esthetic Zone
Loss of a clinical crown through fracture is a common indication for crown lengthening. In the esthetic zone, however, apical repositioning of the gingival margin may be unacceptable esthetically,
Minimal Vertical Dimension of the Root Trunk
On molar teeth, the root trunk is defined as the distance from the furcation to the level of crestal bone. If the trunk distance is less than 4 mm, crown lengthening cannot establish the 4 mm of tooth exposure without extending past and into the furcation
Surgical Techniques for Crown Lengthening
Surgical crown lengthening does not require an extensive list of instruments or supplies. Generally the procedure will include a standard oral surgery setup to incise, elevate, reflect, reposition, and suture tissue. In addition, a set of periodontal curettes, a small chisel, and a series of surgical-length round burs will be sufficient to complete most procedures. If the clinician is already equipped to perform periapical surgery, few additions to the instrument list will be necessary. A suggested instrument list is provided in
TABLE 17-1 Suggested Instruments for Crown Lengthening Procedures
| Instrument | Suggested Choice |
|---|---|
| Scalpel | Bard-Parker No. 15 |
| Periosteal elevator | No. 7 Spatula or Woodson No. 1 |
| Periosteal retractor | Seldin No. 23 or Minnesota |
| Periodontal curettes | Gracey 1-2, 11-12, 13-15, and 15-16 |
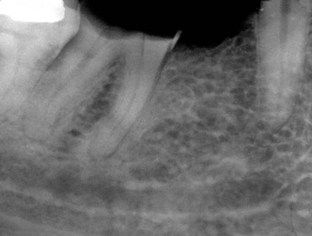
| Surgical-length burs | Round (USA) No. 2, 4, 6, 8; ISO 1.0, 1.4 1.8, and 2.3 mm ( |
| End-cutting bur | Brasseler (USA) 958C WDEPTH |
| Chisel | Wedelstadt 1-2 |
| Needle holder | Mayo-Hegar 140 mm, preferably with tungsten carbide |
| Suture | 4-0 Resorbable |
* Hu-Friedy Co., Chicago, Illinois, USA.
† Brassler USA, Savannah, GA, USA.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses