CHAPTER 17 INTRAORAL BONE GRAFTS FOR DENTAL IMPLANTS
Autogenous bone has long been considered the gold standard for the grafting of ridge resorption and osseus defects. Autogenous bone grafting is a well-documented and clinically proven technique for bone augmentation in the preparation of sites for dental implant placement. The use of autogenous bone with dental implants was originally discussed by Brånemark et al.1 (1975) in the treatment of the atrophic edentulous maxilla and mandible. Early studies focused on the use of iliac bone grafts for reconstruction of severely atrophic jaws.2 Other donor sites for bone harvest have been studied, including the calvarium, rib, fibula, proximal tibia, and maxillofacial regions such as the mandibular symphysis and ramus. Autogenous bone can be procured and used in several forms, including cancellous marrow, particulated bone chips, or blocks. The timing of graft placement, and implant insertion has been well researched. Although many early studies attempted simultaneous graft and implant placement the preferred approach has become staging the events with delayed implant placement into the healed bone graft. Although autogenous bone grafting has proven to be a predictable method of enhancing bone volume, early studies reported lower implant survival rates in grafted sites.2 The use of implants with microtextured surfaces has improved results in regenerated bone with survival rates comparable to those in native bone.
 Bone Biology
Bone Biology
Autogenous bone is the only graft material that has osteogenic properties. Viable cells transplanted within the graft can survive to form new bone. These bone cells are found in higher concentration in the cancellous marrow. Upon harvesting the bone graft it should be immediately stored in sterile saline to maintain cellular vitality and minimal time should elapse before placement.3 The fewer viable cells contained in cortical grafts are probably insignificant in new bone formation. Autogenous bone grafts are also osteoinductive because they contain bone morphogeneic proteins and growth factors that induce new bone formation in the surrounding tissues.4 Osteoprogenitor cells within the surrounding tissues are transformed into osteoblasts through osteoinduction. The mineral component of the autogenous bone graft acts as an osteoconductive scaffold for bone formation.5 The bone graft is incorporated into the recipient site through remodeling and gradual replacement with new bone over time.
A free autogenous bone graft must become revascularized in order to incorporate. The cancellous portion of the graft revascularizes faster than the cortical bone.6 The dens cortical bone revascularizes through its existing haversian system.6 Angioneogenesis is associated with cutting cones that resorb the graft and slowly replace it with new bone (creeping substitution).
Graft resorption is a necessary aspect of graft incorporation to the osseous recipient site. The embryologic origin of an autologous bone graft has been suggested as a predictor of graft resorption. Membranous bone grafts from the mandible or calvarium have been found to reveal less resorption than grafts from endochondral sites such as the iliac crest.7–10 More recent studies emphasize the importance of the microarchitecture of the bone used for grafting over embryologic origin.5,11 Denser cortical bone grafts resorb less than more porous cancellous bone grafts when used for onlay bone augmentation.11 Cortical bone grafts from the mandible exhibit minimal resorption and maintain their dense quality, making them ideal for onlay augmentation prior to implant placement.12 Upon incorporation, the volume loss of cortical bone grafts used for onlay augmentation is less than 20%.13 Corticocancellous bone grafts from the ilium are associated with greater resorption due to the thinner outer cortex and more porous cancellous component. Whereas the greatest change in the width of a corticocancellous graft occurs in the first 3 months, the volume loss in height stabilizes after 1 year.14 It is prudent to slightly overbuild the reconstructed ridge in anticipation of some volume loss upon healing. It is also important to make a distinction between the graft morphology (particulate, block) and whether the graft is used for onlay or interpositional placement. Interpositional bone grafts (grafts placed between or within the host bone) typically resorb less than bone used for onlay augmentation. Extraction socket and sinus floor augmentations are more comparable to interpositional than to onlay bone grafts; therefore, less resorption would be expected.
 Preoperative Evaluation
Preoperative Evaluation
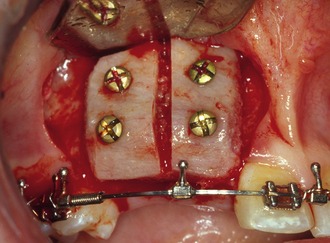
Planning of the bone graft surgery requires a comprehensive evaluation of the graft donor and recipient site. Conventional radiographs such as panoramic and periapical films are useful in the evaluation of the bone defect, ridge atrophy, adjacent dentition, and local anatomy. Computed tomography (CT) is useful for three-dimensional views of the bone deficiency and can also be used to assess intraoral donor sites. Implant planning software used with the CT scan is helpful to more precisely evaluate the reconstruction.15
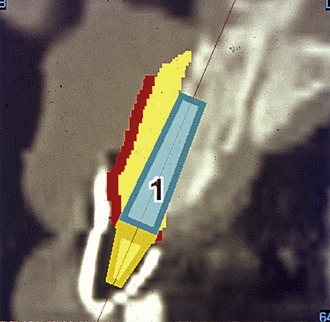
Mounted study casts and a diagnostic wax-up of the replacement teeth allow the surgeon to evaluate the ridge morphology in relationship to planned prosthetic outcome (Figure 17-1). Diagnostic casts also can be used for the fabrication of a radiographic template worn during the CT scan.16 The template is coated with barium sulfate to reveal the radiopaque outline of the prosthetic tooth positions in the tomographic view of the residual ridge (Figure 17-2). This allows a determination of graft volume requirements and donor site options (Figure 17-3). A template of the planned prosthetic tooth position is also helpful for use during graft surgery to confirm graft positioning for future implant placement. A stereolithographic model of the jaw can be generated from the scan to further plan the case.17
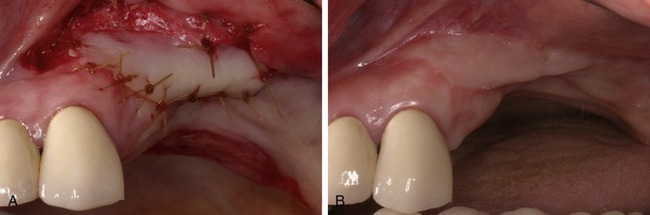
The soft tissue character in the recipient site should be assessed for quantity of keratinized tissue, thickness of the mucosa, muscle attachments, and the presence of scar tissue (Figure 17-4). It is often better to correct soft tissue problems prior to bone grafting. Autogenous free gingival grafts are preferred to cadaveric dermis for increasing the amount of keratinized tissue (Figure 17-5). Areas of thin alveolar mucosa can be enhanced with the interpositional placement of allogeneic dermis or connective tissue grafts. Removal of scar tissue improves blood supply to the area and helps improve the mobility of the soft tissue flap over the bone graft. The removal of a frenum or high muscle attachments in the recipient site will reduce tension on the incision line. Soft tissue corrective surgery should be performed at least 8 weeks prior to bone graft surgery to allow incorporation of the tissue graft and redevelopment of vascularity in the area.
 Patient Preparation
Patient Preparation
Because the consequences of postoperative infection are detrimental to graft success, the patient should be placed on prophylactic antibiotics starting with a loading dose 1 hour prior to surgery and continuing for 1 week.12,18 Amoxicillin is commonly used because it is well absorbed and requires administration only three times a day. Penicillin-allergic patients may be treated with a cephalosporin, clindamycin, or clarithromycin. Preoperative chlorhexidine rinsing can reduce the bacterial contamination of intraorally harvested bone grafts.19 Chlorhexidine rinse is used thereafter twice daily following surgery because oral hygiene procedures, such as brushing and flossing, are avoided around the surgical site. The use of short-term glucocorticoids can diminish postoperative facial swelling, local flap edema, and discomfort. Dexamethasone may be administered in a tapering dose over a 3-day period.20 Narcotic analgesics are prescribed for use during the immediate postoperative course. Thereafter the patient may transition into the use of nonsteroidal antiinflammatory medications. Preoperative antisialogogue agents such as glycopyrrolate are useful to decrease salivary flow that may carry bacteria into the graft site. Although clean technique has been found acceptable for dental implant surgery,21 clinicians should consider using aseptic technique during more extensive and prolonged reconstructive procedures. Most cases involving autogenous bone grafting in the office are performed under sedation. The clinician may use oral premedication such as triazolam and/or intravenous drug regimens.
 Bone Graft Donor Sites
Bone Graft Donor Sites
Maxillary Tuberosity
Although the maxillary tuberosity offers a smaller amount of bone than other donor sites, the softer consistency of the graft is often favorable for filling bone defects.22 The bone in the tuberosity area is porous and the outer cortical layer is thin. Because the tuberosity is in the same surgical field when performing a lateral approach to sinus grafting, it should be routinely considered for bone harvest.23 The amount of bone that may be obtained can be deceiving because the mucosa over the tuberosity is usually quite thick. A periapical or panoramic radiograph can be used to better assess the underlying bone. CT scans of the maxillary sinus region can allow three-dimensional quantification of the area.
The anatomic limitations of tuberosity bone harvest include the maxillary sinus, pterygoid plates, molar teeth, and the greater palatine canal. To gain access to the area for bone harvest an incision is made along the ridge crest over the tuberosity. A vertical releasing incision is made along the lateral aspect of the posterior maxilla. Mucoperiosteal reflection exposes the tuberosity, ridge crest, and lateral maxilla. The palatal tissue also should be elevated to reveal the entire width of the tuberosity. The graft may be harvested with a chisel or rongeurs. The chisel edge should be kept slightly superficial to the maxilla to shave off pieces of tuberosity bone and prevent inadvertent sinus communication.24 A chisel can also be used along the posterior lateral maxilla to obtain a thin piece of cortical bone to cover the window following grafting of the sinus floor (Figure 17-6).
Mandibular Symphysis
The symphysis of the mandible has been used extensively for onlay and sinus bone grafting.12,25–29 Techniques to harvest block or particulate bone grafts from the anterior mandible have been reported. The symphysis donor site offers the greatest volume of intraoral bone. The average interforaminal distance is approximately 5 cm and the depth of the anterior mandible usually exceeds 1 cm.30 The ease of surgical access is another advantage of the symphysis region. However, as will be discussed, the morbidity of this donor site has reduced its use by many clinicians. The symphysis is often reserved for cases requiring thicker block grafts that cannot be obtained from other intraoral donor sites (Figure 17-7).
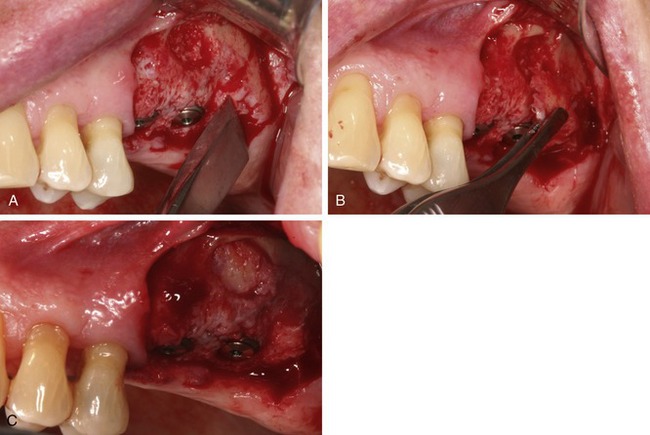
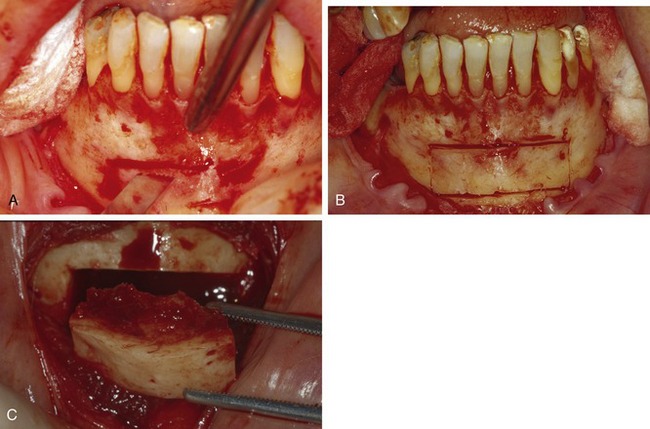
Bilateral mandibular blocks are administered with 0.25% bupivicaine, 1:200,000 epinephrine. Local infiltration in the vestibule of the anterior mandible is administered using 2% lidocaine, 1:100,000 epinephrine. Additional local anesthesia is often needed at the base of the mandible to block cervical innervation. Exposure of the symphysis may be obtained through a sulcular or vestibular approach. A sulcular incision may result in gingival recession and should not be used when mucogingival defects are present. The sulcular incision should extend to the premolar regions bilaterally. Small vertical releasing incisions may be made posteriorly. The vestibular incision is made in the mucosa between the cuspid teeth approximately 1 cm from the mucogingival junction (Figure 17-8). Limiting the distal extent of the incision will reduce the risk of mental nerve injury. A vestibular approach allows easy access but produces more soft tissue bleeding and possible intraoral scar formation. Both approaches have been associated with transient postoperative paresthesia. A mucoperiosteal flap is reflected to expose the mental foramina and the inferior border of the mandible (pogonion).
After the symphysis region is exposed the osteotomies for graft harvest are planned. The dimensions of the graft are determined by the bone volume needed to reconstruct the defect. Osteotomies should be kept at least 5 mm from the root apices and the mental foramina.12,31,32 In most cases the inferior and lingual cortices of the mandible are left intact. The facial cortex is fairly thick and the underlying cancellous bone is usually dense. The osteotomies may be made with a carbide fissure bur (#557 or #701) in a straight surgical handpiece, sagittal saw, or a Piezoelectric unit under copious sterile saline irrigation (Figure 17-9). Pilot holes are helpful in laying out the bony cuts. It is advised to have the patient bite together to gain better access to the chin area. The depth of the osteotomies must extend though the outer cortex and into the cancellous bone. Deeper cuts are necessary if a thicker graft is desired. The lingual cortex is typically thick, and inadvertent perforation is unusual.
Following the osteotomies, the graft is removed with a chisel (see Figure 17-9, C). A unibeveled chisel is tapped along the osteotomies, with the exception of the inferior border, to fracture the block from its cancellous base. The bevel is placed toward the center of the graft. The mandible should be supported during these maneuvers. The block bone graft also may be harvested in segments by sectioning the rectangular piece in the midline. Two bone blocks are often easier to harvest because the second block can be fractured from its lingual base with the chisel. Following the removal of the block graft, hemostatic materials such as collagen or gelatin may be placed over the cancellous bone. When larger bone grafts are harvested the donor site should be filled with a bone substitute such as resorbable hydroxylapatite to maintain facial contour.12 Smaller or particulate bone grafts may be procured using trephine burs, bone collection traps, or bone scraping instruments.33–35 Closure of the donor site should be performed after the graft is inserted into the recipient site. This will minimize the time between graft harvest and placement. The vestibular incision is closed in layers using resorbable sutures. The deeper layers may be sutured with 4-0 Vicryl and the superficial mucosa can be closed primarily with 4-0 chromic gut. The sulcular incision is closed with interrupted sutures through the papillas. Postoperative pressure dressings are used over the chin to reduce edema, hematoma formation, and incision line opening.
The mandibular symphysis is associated with a higher incidence of postoperative complications than other maxillofacial donor sites.28,36–38 Altered sensation of the lower anterior teeth is a relatively common postoperative symptom when bone blocks or trephine cores are removed12,28,36–38 because the contents within the incisive canal of the symphysis that innervate the teeth are disrupted during bone harvest (Figure 17-10). Patients describe dullness in sensation of the incisors, which usually resolves within 6 months. The need for endodontic treatment of anterior teeth is very rare but pulpal injury has been noted by the evidence of secondary dentin formation. Neurosensory disturbances in the chin region also may be encountered, even when a sulcular incision is used.36–38 The incidence of temporary mental nerve paresthesia for symphysis graft patients is usually low but has been found to be as high as 43%.36 Meteorotropism of the chin has also been reported.36 Although the vast majority of these nerve injuries recover, they are disconcerting to patients. It is prudent to discuss, prior to surgery, the possibility of temporary altered sensation of the teeth and chin. Although no postoperative alteration in soft tissue chin contour has been reported, patients are often concerned with the possible aesthetic consequences of bone removal from this area.36 Radiographic evidence of incomplete bony regeneration has been reported in elderly patients.39 Filling the donor site with a resorbable bone substitute such as bank or bovine bone can help alleviate patients’ concerns.12 Ptosis of the chin has not occurred and can be prevented by avoiding complete degloving of the mandible/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses