Implant Restoration of the Maxillary Edentulous Patient
Nicola U. Zitzmann
School of Dental Medicine, University of Basel, Switzerland
Implant restorations in the maxillary edentulous patient are one of the most daunting challenges in dentistry, due to high patient expectations, complex diagnosis, difficult initial morphological situations, and compound surgical and restorative requirements. This chapter will examine the current knowledge on patient selection and risk factors for fixed and removable implant prostheses for the edentulous maxilla through the lens of a methodical diagnostic regimen. Guidelines will be offered for specific design considerations of implant prostheses. While long‐term treatment success has been an elusive achievement, a discussion of patient‐reported outcome measurements will assist the clinician in prognosis as part of a comprehensive informed consent.
Morphology of the edentulous maxilla
Tooth loss generally occurs earlier in the maxilla than in the mandible, which is most likely related to early damage from anterior trauma and vulnerability to periodontal disease, particularly with furcation involvement in the first premolars and molar teeth. Further, periodontal and endodontic treatment of maxillary molars is very demanding, due to contorted root canal anatomy, which complicates treatment and tooth preservation. As a consequence edentulism in the maxilla is more frequent, affecting approximately 40% of the population 65 years and older; in this age group 27% are edentulous in the mandible and these patients are almost invariably edentulous in both jaws.1,2
The scaffold of the maxillary bone is susceptible to severe alveolar ridge resorption following tooth loss, particularly in the anterior region, with thin cortical bone plates on the buccal aspect. In the posterior region, an increase in the pneumatization of the maxillary sinus reduces the bone volume (Figure 17.1a). Due to normal tooth inclination in the maxilla, the arch circumference of the maxillary dentition is larger than its bony foundation and normally overlaps the mandibular dentition. The faciolingual axial inclination of the central incisors, described as the angle between the long axis of the tooth and a line drawn perpendicular to a horizontal plane, measures 28°, it is on average 26° for lateral incisors, and 16° for canines.3 This tooth angulation, particularly in the anterior region, contributes to the resorptive pattern of the edentulous maxilla, which is superiorly and medially directed, resulting in a reduced arch circumference (Figure 17.2).4,5 For implant placement, the edentulous maxilla frequently has limited bone height and width, with a bone foundation displaced cranially and medially when compared to the ideal position of the clinical crowns. Depending on the progression of the bone resorption, this initial morphological situation frequently leads to a wide, unparalleled, fanned implant position, unless buccal augmentation has been anticipated. These morphological changes following tooth loss, accompanied by difficult implant procedures, require a thorough initial diagnosis by the clinician to visualize the three‐dimensional (3‐D) relationship between the ideal tooth position and the underlying soft and hard tissues. When there are high esthetic demands in addition to full display of the maxillary sextant, the margin for error is minimal. For this diagnostic sequence extra‐ and intraoral factors should be assessed systematically (Table 17.1), so that a reasoned treatment recommendation can be given and explained to the patient.
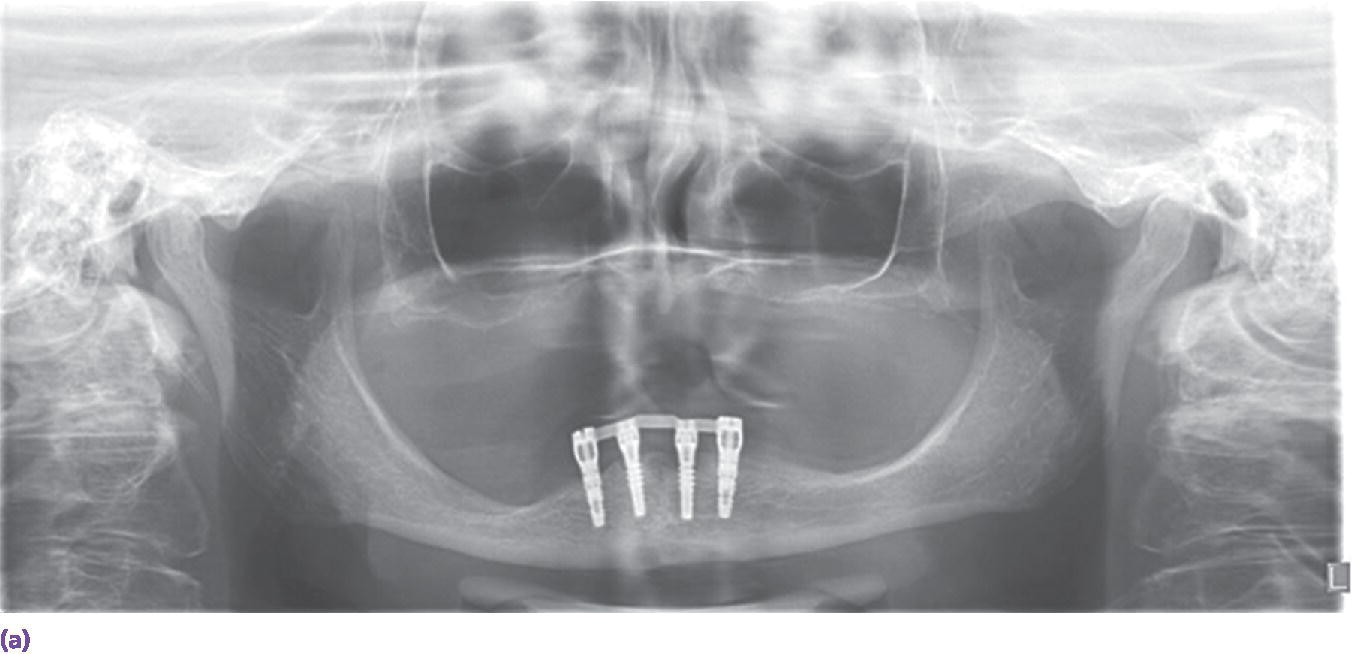
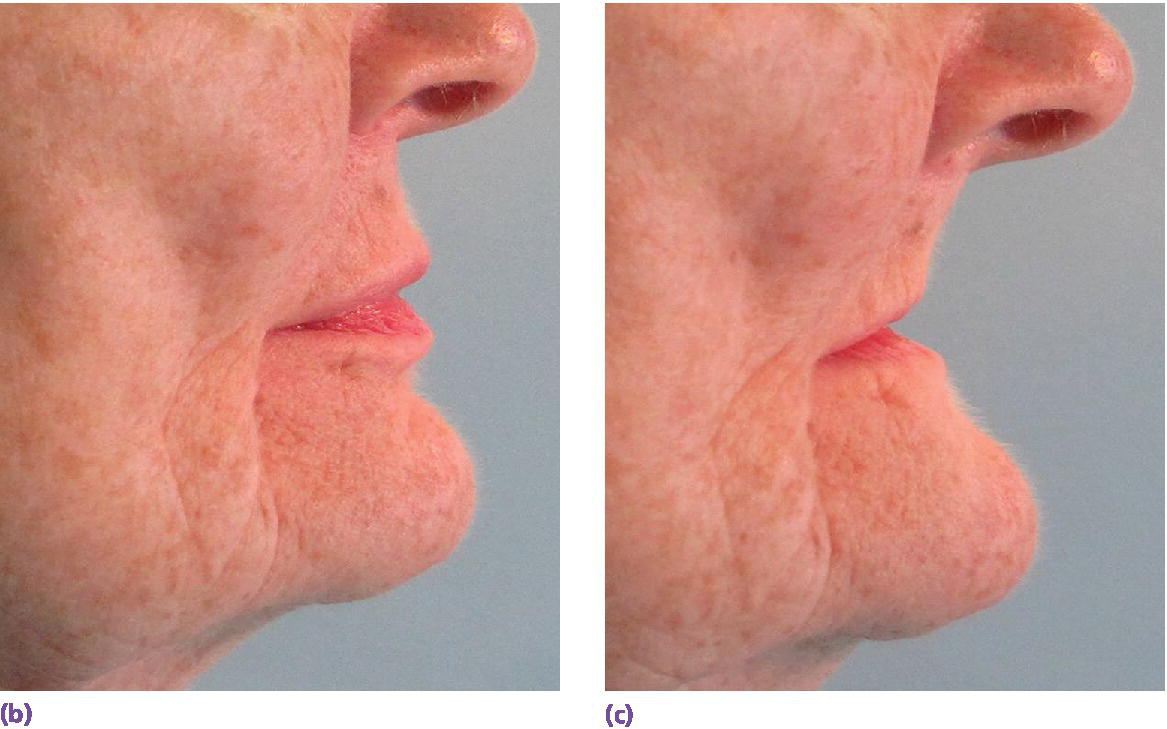

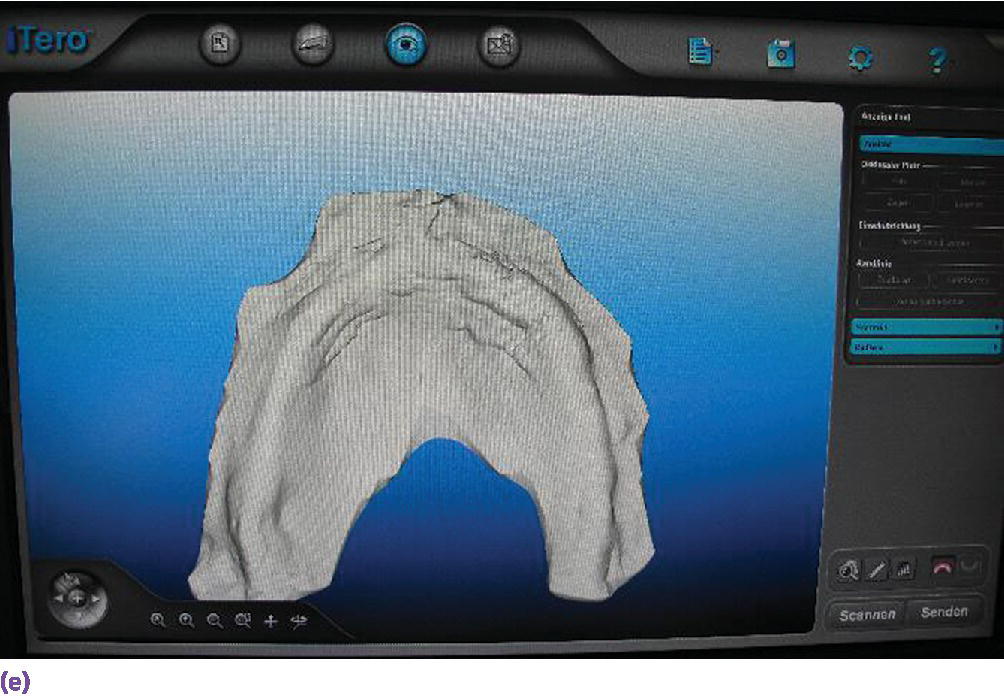
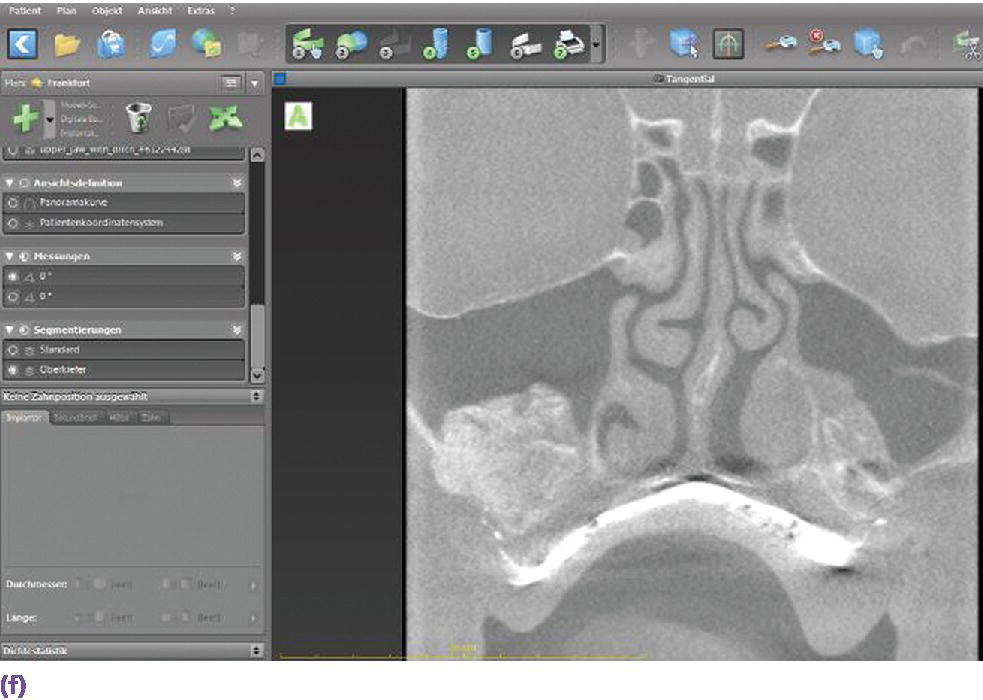
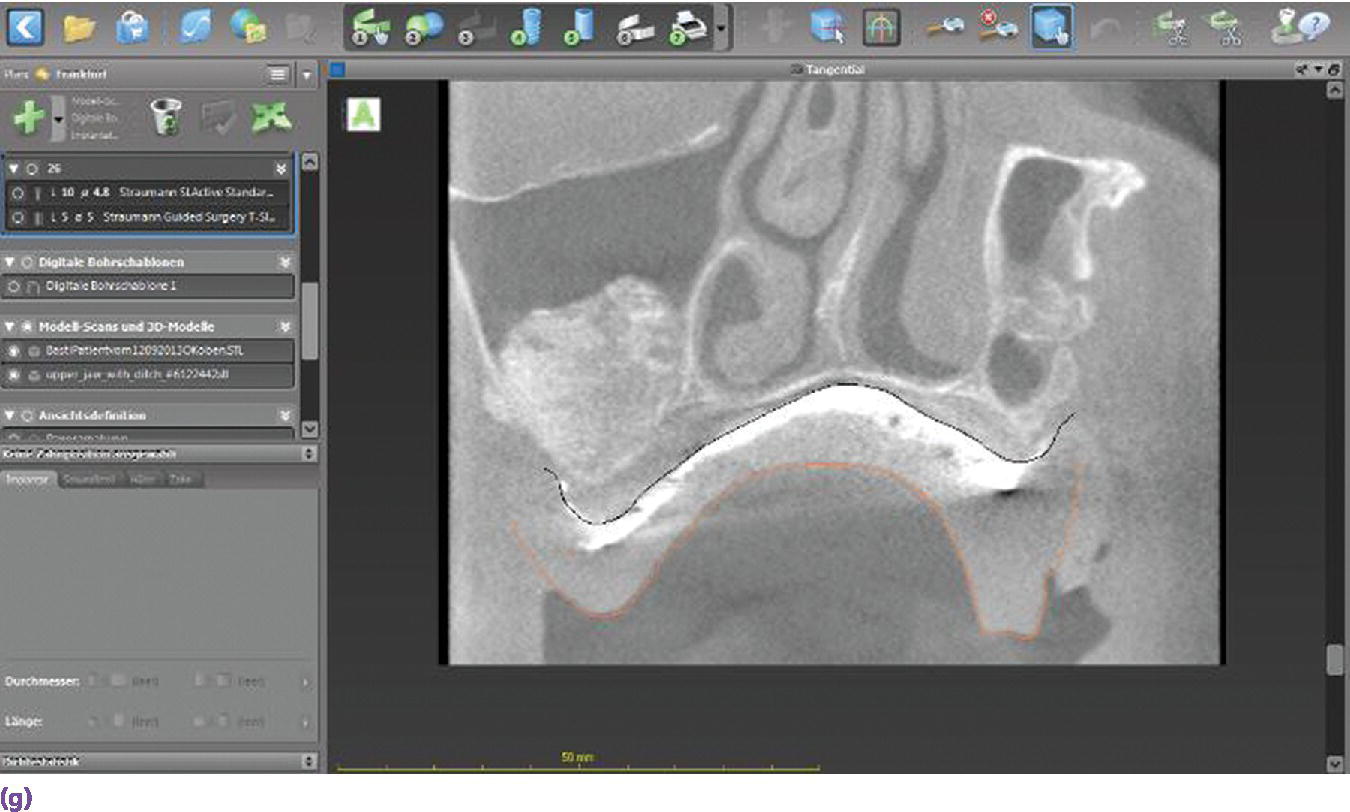
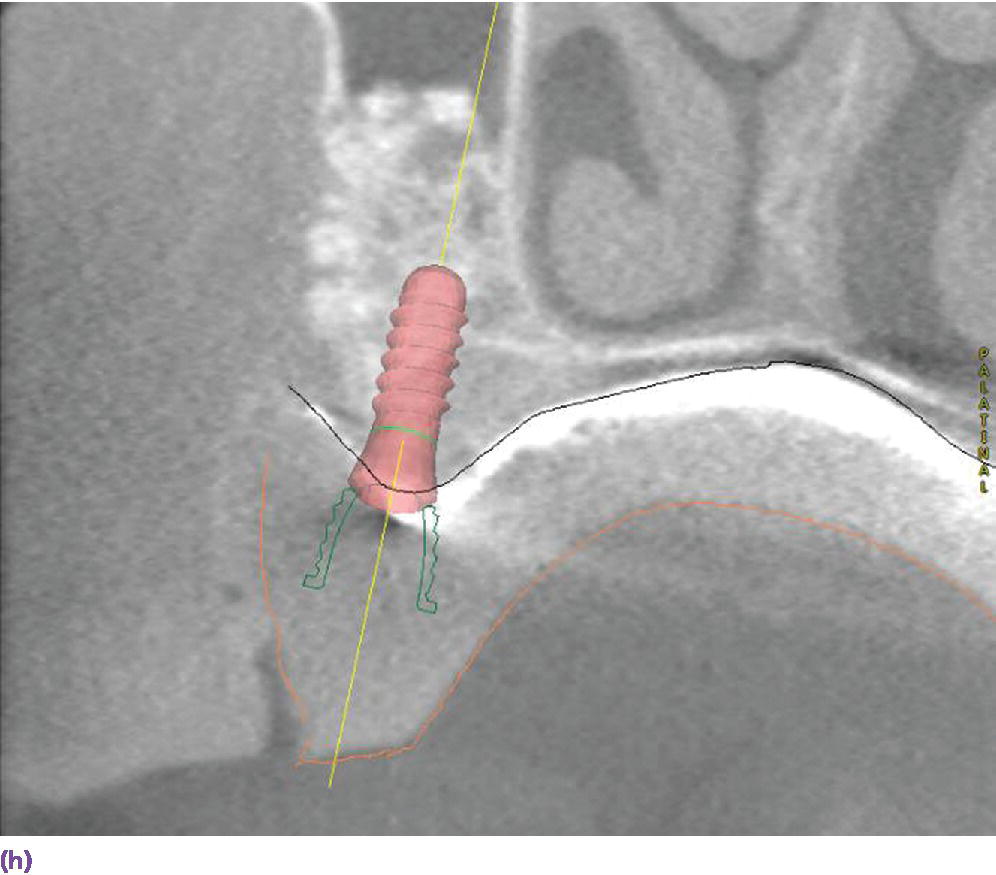
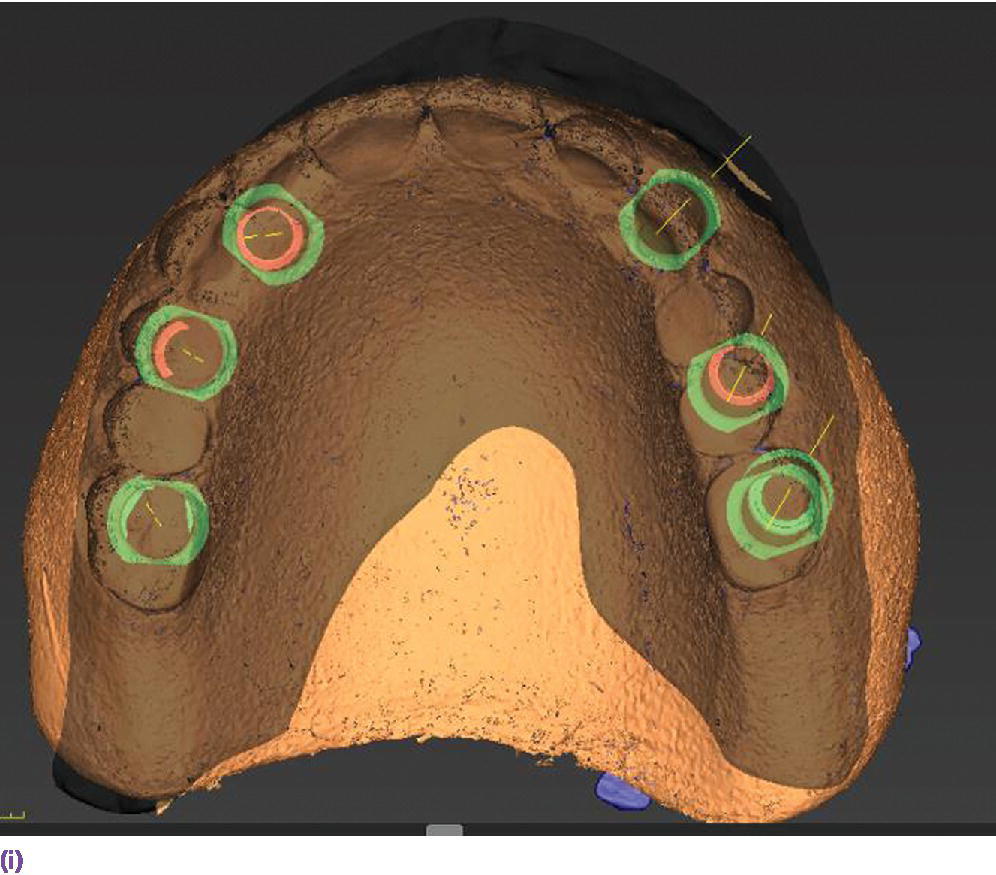
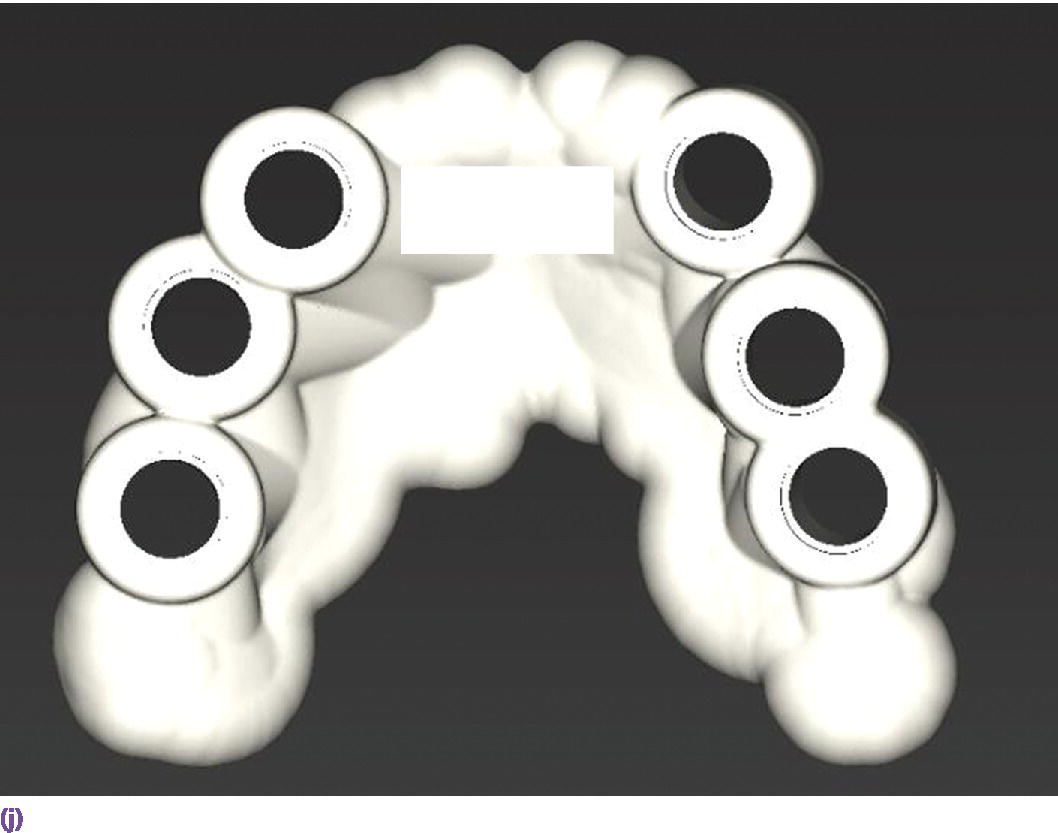

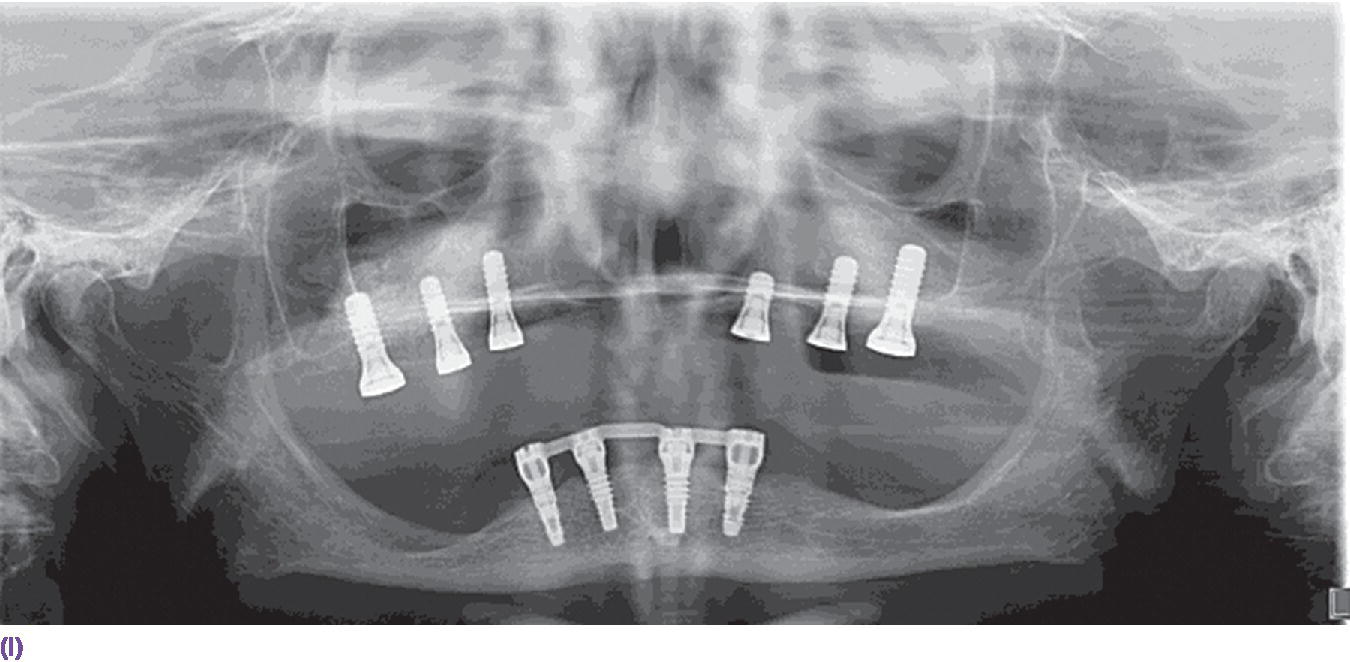
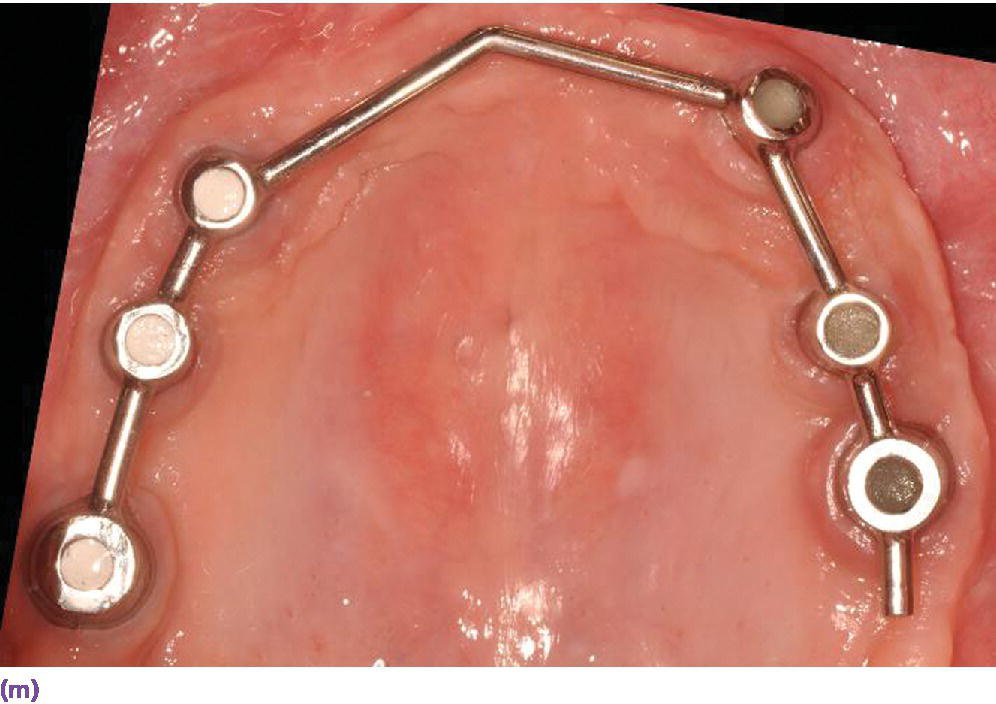

Figure 17.1 (a) Panoramic radiograph showing advanced bone resorption in both jaws with increased pneumatization of the maxillary sinuses and alveolar ridge resorption in the anterior maxilla. (b, c) Patient’s profile with and without complete dentures in place with obvious need for facial support by prosthesis flanges. (d) Clinical situation of the patient with advanced bone resorption following bilateral maxillary sinus augmentation. (e) Intraoral surface scan of the mucosal tissues (iTero, San Jose, California). (f) CBCT scan with mucosal contour displayed by using jodoform paste applied onto the prosthesis base. (g) Image created with coDiagnostiX‐software superimposing the CBCT data with the iTero‐surface‐scan (black line) and an additional surface scan of the prosthesis (Projektor MPT, Breuckmann GmbH, Meersburg, Germany; red line). (h) Prosthetically‐driven implant planning for an implant overdenture with bar retention (black line illustrates mucosal contour, red line indicates prosthesis contour). (i) Six implants planned. (j) Virtual template designed according to the determined implant positions including blueprint for the sleeves. (k) Printed template based on exported iTero data transferred as stl.‐file to a 3D‐Printer (Objet Eden, Stratasys; right). (l) Postoperative panoramic radiograph after implant placement, using the template for guided preparation of implant beds. (m) Prefabricated round Dolder bar (soldered gold bar). (n) IOD with cast framework and clips inserted (Galak, Cendres & Métaux). (Technician: Clemens Gessner, Basel.)
Source: reproduced with permission from Dr. Sebastian Kühl.
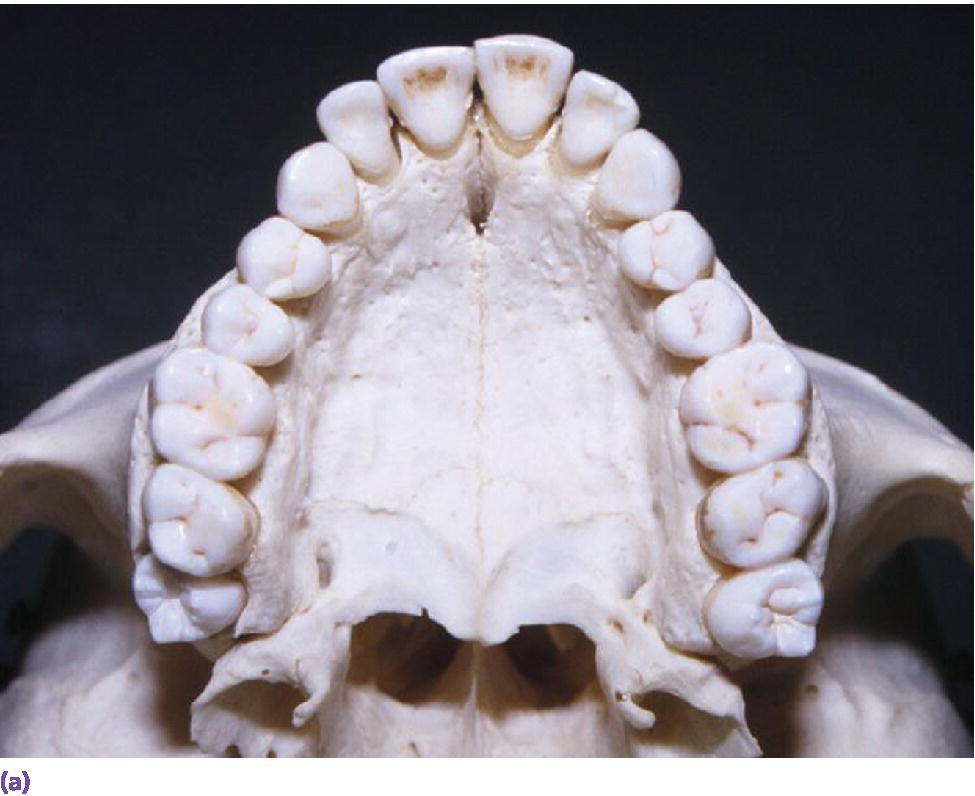

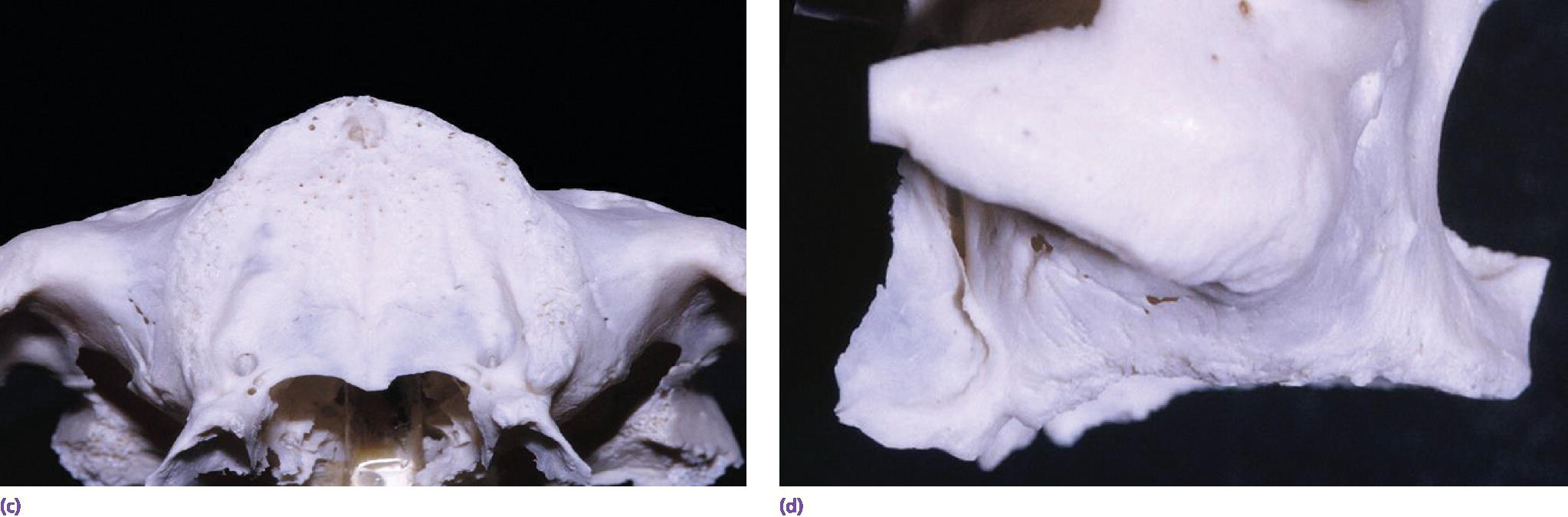
Figure 17.2 Dentate (a, b) and edentulous (c, d) maxillae (occlusal and lateral views).
Table 17.1 Diagnostic form for the edentulous maxilla (distribution of crosses indicate recommended prosthesis design).
| a) Patient factors. General risk factors for implant treatment and bone augmentation: smoking, history of aggressive periodontal disease, residual probing pocket depth of ≥5 mm at implant placement | |||||
| Patient’s request | Fixed □ | Removable □ | |||
| No palatal coverage □ | Palatal coverage accepted □ | ||||
| Reason for request | Psychological impairment □ | Poor stability and retention of CD (no CD improvement feasible) □ | |||
| Finances | Acceptance □ | Acceptance □ | Limitations □ | ||
| Oral hygiene dexterity | Excellent □ | Excellent □ | Good □ | Limitations □ | |
| b) Extraoral factors | |||||
| Smile line | Low □ | Average □ | High □ | ||
| Lip and facial support | Not required □ | Needed □ | |||
| Intermaxillary relation/skeletal class | Class I (congruent) □ Class II (retrognathic mandible) □ |
Class III (prognathic appearance), small max. arch circumference, and/or concave profile □ | |||
| c) Intraoral factors | |||||
| Degree of alveolar ridge resorption | Moderate □ | Advanced □ | Advanced to severe □ | ||
| Ridge defects | None □ | Only vertical □ | Horizontal or combined □ | ||
| Intermaxillary space (max. mucosa to mand. incisal edges) | 8–10 mm □for PFM design | ≥12 mm □for IFCD design | ≥12 mm □for bar design | ≥8 mm □for single attachments | |
| d) Recommended implant restoration | |||||
| Description | Implant‐supported fixed dental prosthesis (metal–ceramic, PFM) □ | Implant‐supported fixed complete denture □ | Implant overdenture (IOD) □ | ||
| Anchorage | Preferably screw‐retained □ | Bar splint □ | Single attachments/solitary anchors □ | ||
| Number of implants | 6–8 □ | 4–6 □ | 4–6 □ | 4 □ | |
| Implant position and angulation | In accordance with clinical crown position □ | Approximately at crown positions □ | Compensation of divergent implant angulations □ | Limited options for divergent implant angulation □ | |
| Varying implant positions requiring milled bar with overcast □ | Every 2nd tooth position for approx. 8 mm clip length of prefabricated bar □ | ||||
Diagnostic phase
An adequate existing complete denture (CD) can be used for diagnostics, and the thickness of the buccal flange can be indicative of the necessary lip and cheek support (Figure 17.1b, c).6,7 A resilient cast can be produced, which is mounted in the articulator at the appropriate occlusal vertical dimension.8 The anterior dentition is then keyed with silicone to visualize the available intermaxillary space and the thickness of the buccal prosthesis flange, which will indicate facial and lip support needs and further dictate a fixed or removable prosthesis (Figure 17.3a–c).

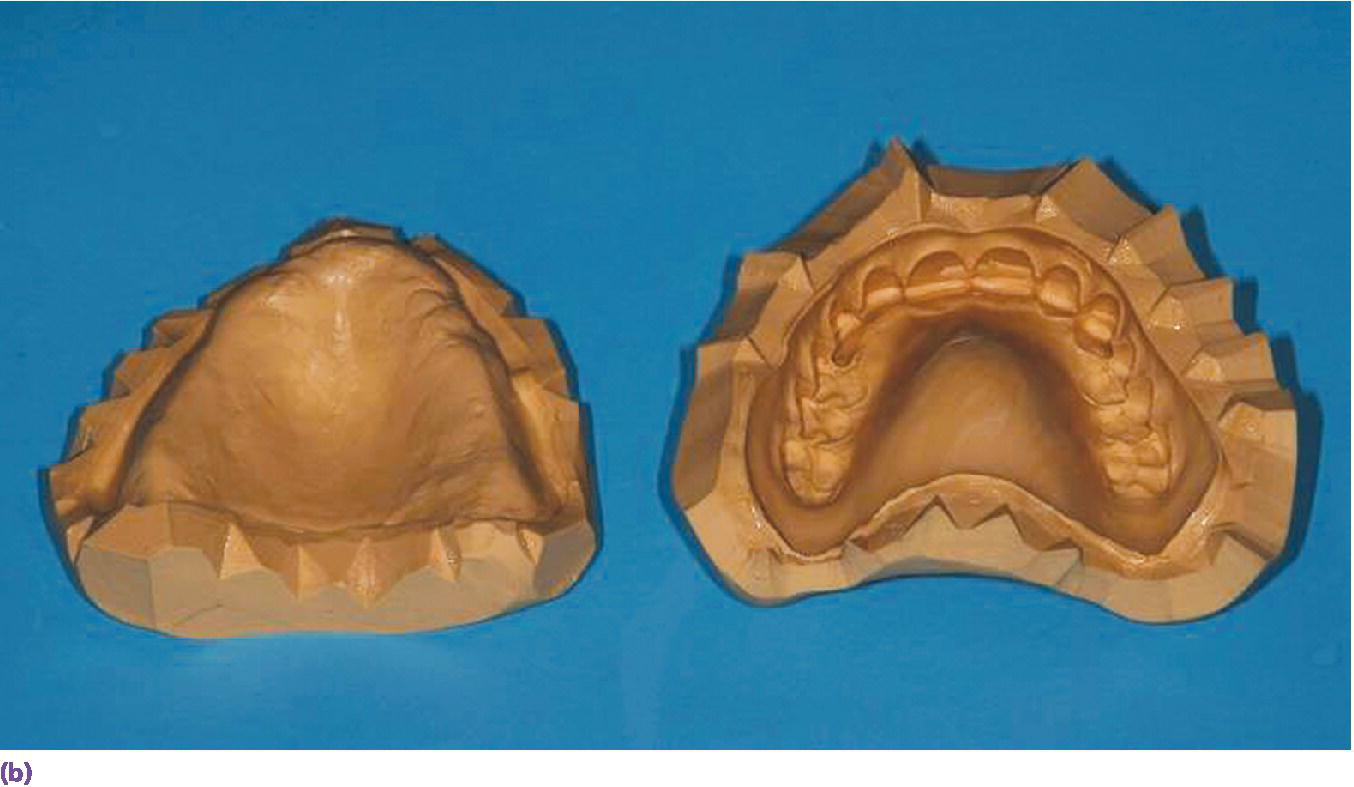
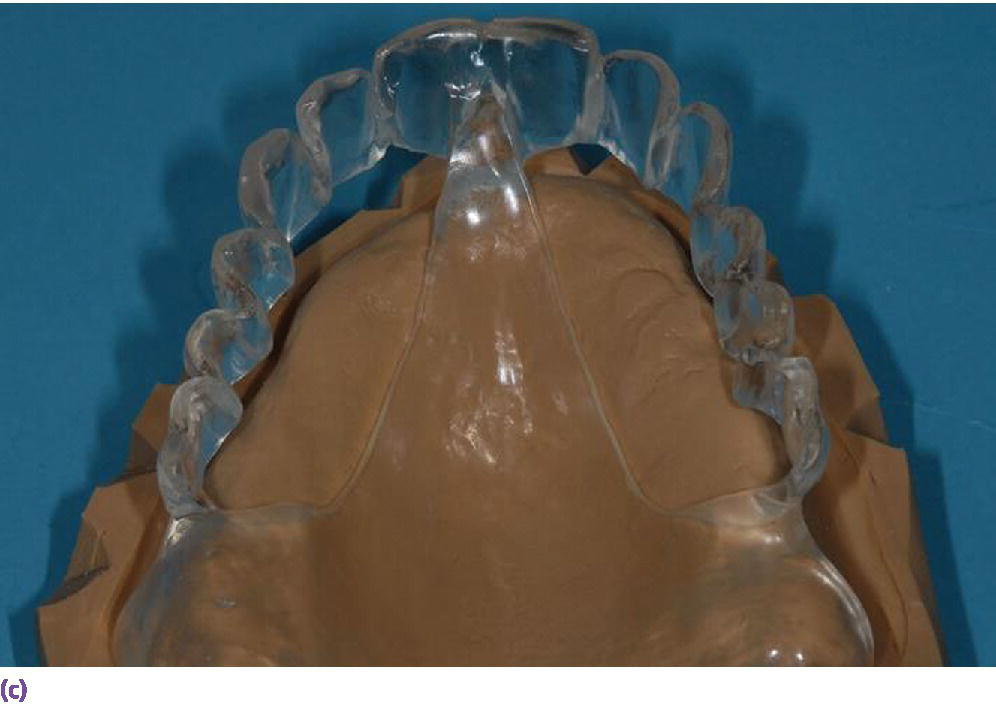





Figure 17.3 (a) Clinical situation of existing denture with adequate tooth position. (b) Denture is used to fabricate a resilient cast, which is keyed to visualize the relationship between ideal tooth position and underlying tissues. (c) Cast is used to fabricate a surgical template. (d) Set‐up made without buccal flange, clearly illustrating that soft tissue support can only be provided by an implant overdenture. (e) Clinical situation with six implants placed. (f) IOD retained at stud abutments (locators) and an anterior bar (Bredent Vario Soft) with an overcast. (g, h) Clinical situation with reduced palatal coverage and buccal flange extension. (Technician: Alwin Schönenberger, Vision Dental Chiasso.)
If the existing dentition and restoration deviate from an ideal vertical dimension of occlusion or tooth position, a new set‐up (similar to the wax trial for a complete denture) should be made to establish the occlusal plane with a correct maxillary incisal edge position and to evaluate the tooth display during smiling.9,10 This set‐up can be prepared without a buccal flange to simplify the clinical analysis of a potential need for facial and lip support during try‐in, especially when a fixed restoration is desired by the patient (Figure 17.3d). The major factors for establishing the correct anterior tooth arrangement and the occlusal plane are based on complete denture principles and are specifically elucidated in the following protocols.10,11
- Determine the incisal edge position of the central incisors, which overlap the occlusal plane about 2 mm (normal vertical overlap) and contact the vermillion border of the lower lip when an F‐sound is produced. Depending on the upper lip length (see below), 1–2 mm of the incisal edge should be displayed in repose in the average patient, while more is visible during smiling. The length of the central incisor is 10.5 mm on average,3 but may be more in elderly patients, in whom some gingival recession can be expected.
- The length of the upper lip, measured from the base of the columnella (subnasal) to the philtrum location, is related to the amount of the maxillary anterior dentition being exposed in repose and also influences the incisal edge position and the occlusal plane (Figure 17.4a, b).12
- The smile line is determined by the tonus of the orofacial muscles influencing the movement of the upper lip during speech and smiling (Table 17.1b).13 Tjan et al. described the average smile as having the position of the upper lip such that 75–100% of the upper incisors and the interproximal gingiva are displayed during smiling. This position was distinguished from the high smile line, where there is additional exposure of part of the gingiva, and from the low smile line, where less than 75% of the maxillary anterior teeth is displayed.14 In patients designated for implant treatment in the maxilla, evaluation of the smile line should be performed without the denture in place. When even the alveolar ridge is displayed during smiling, the use of a buccal flange in a removable prosthesis may be advisable to prevent esthetic problems with exposure of the prosthesis–tissue junction.15 Alternatively, a reduction of the alveolar ridge can be considered, provided that sufficient bone height exists for implant placement.16
- Vertical dimension of occlusion: for the diagnostic set‐up, the height of the lower face, ensuring harmony of the three thirds of the face, and an adequate interocclusal space for correct phonation, must be taken into account.
- Once the incisal edge position, crown length, and angulation have been determined, the relationship to the underlying soft and hard tissues is assessed for implant treatment planning (Figure 17.3c). In the dentate maxilla, lip support is primarily derived from the alveolar ridge shape and the cervical crown contour of the maxillary incisors, but in the edentulous maxilla, the alveolar ridge is frequently located posterior and cranially to the incisors. For an implant fixed dental prosthesis (implant FDP) with a porcelain‐fused‐to‐metal design (PFM), the cervical aspect of the clinical crown should ideally end at the soft tissue level of the alveolar ridge (Table 17.1c, d). In this case, only minimal bone resorption and a limited interarch space with an optimal tooth–lip relationship is present. If a large vertical distance results between the ideally positioned artificial teeth and the underlying tissues, moderate to severe resorption of the maxilla may have occurred (Table 17.1c). Depending on this discrepancy in the bucco‐oral dimension, the practitioner must assess if compensation is feasible with a gingival base of an implant FDP or with an implant fixed complete denture (IFCD) design, without causing oral hygiene constraints. If these requirements cannot be ensured, an implant overdenture (IOD) with a denture base is preferable, which also allows individual contouring on the palate to enable adequate tooth–tongue contact for T‐ and D‐sounds, and to avoid any speech disruption and S‐sound deficiencies (e.g., sigmatism, lisping). This is even more important in patients with a retrognathic appearance of the maxilla with a concave profile, or for compensation of prognathism (Table 17.1b, d; Figure 17.3e–h).10
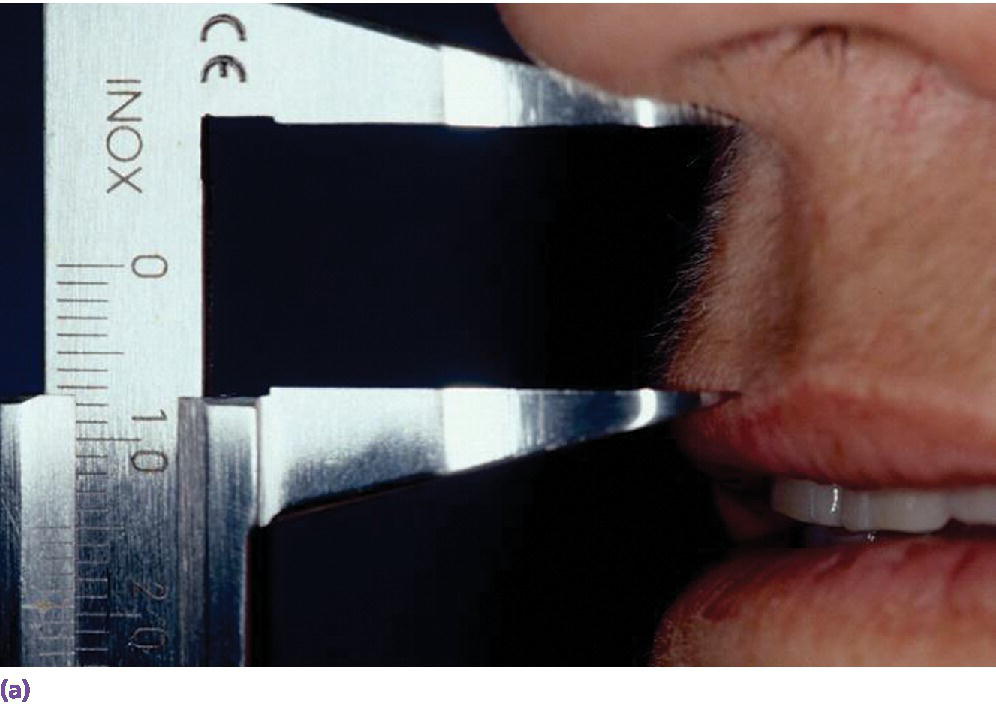
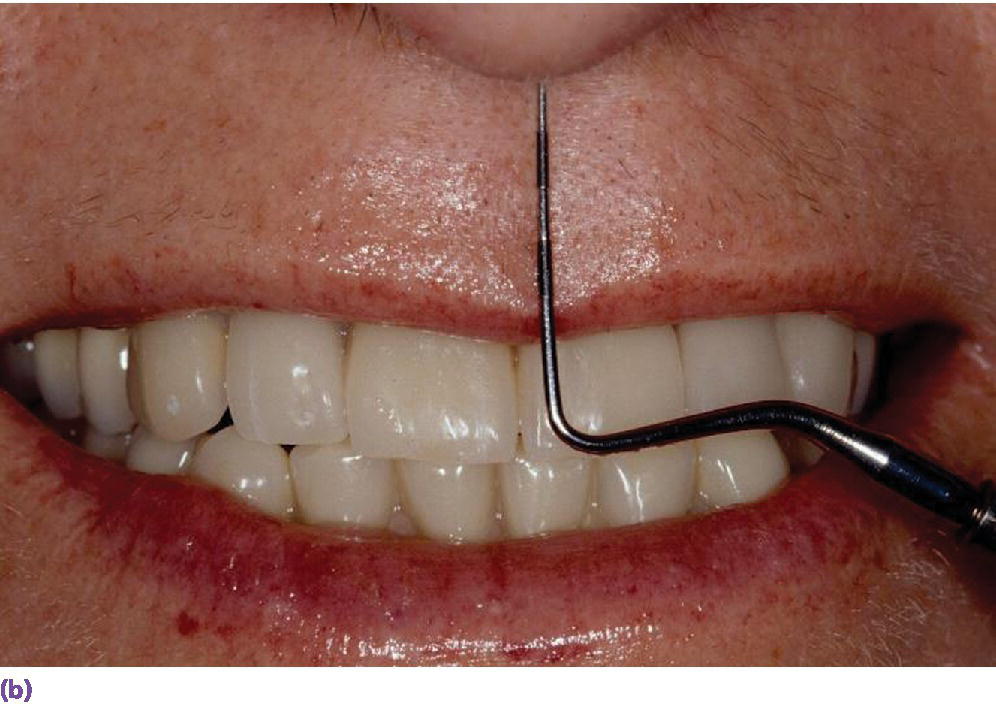
Figure 17.4 (a, b) Initial examination in a patient with a short lip line (15 mm measured from subnasal to philtrum in repose) with adequate denture or diagnostic set‐up in place. The full length of a periodontal probe serves as a reference for the average length of maxillary incisors (23.5 mm), which have to fit below the subnasal point, and helps to determine the adequate incisal edge position.
Radiologic diagnosis and treatment planning
The panoramic radiograph provides a good two‐dimensional overview of the anatomic structures and the available bone in the vertical dimension (Figure 17.1a). Due to the challenges related to the described resorption pattern in the maxilla and the need for implant positioning according to the planned prosthetic restoration, three‐dimensional (3‐D) imaging (e.g., cone beam computed tomography (CBCT) scan) is frequently indicated for thorough diagnostics. Attempts should be made to perform the 3‐D imaging in conjunction with a scan of the diagnostic set‐up (or the adequate existing denture) that allows identification of the tooth position, digital implant planning according to the clinical crown position, and subsequent transfer into a surgical template (Fig. 17.1d–g).17 In former years, radiopaque markers (e.g., titanium pins) were incorporated into a template (Figure 17.5a), depicting the ideal implant position and angulation for a screw‐retained fixed complete denture and were arranged parallel in a surveyor with a similar path of insertion (Figure 17.5b). The horizontal slices of the computed tomography were oriented perpendicular to these titanium pins and perpendicular cross‐sectional reformations were processed, which served for the detailed implant planning and identification of augmentation needs (Figure 17.5c).10 Today, selection of the implant length and diameter in an adequate position and angulation can be performed digitally with specialized software programs, and a surgical template is then printed and designed for support on the mucosa or the bone (Figure 17.1h–k).18
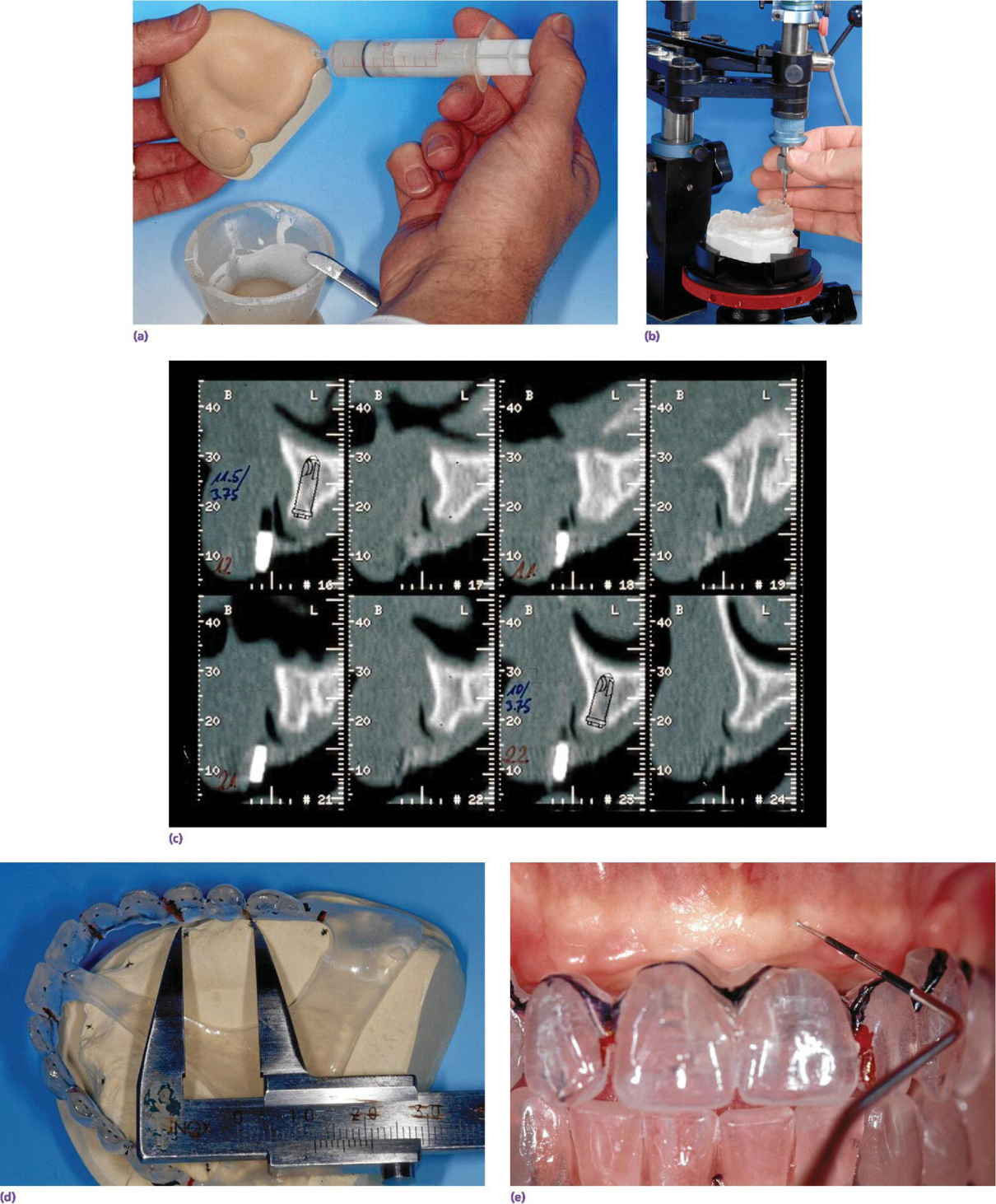

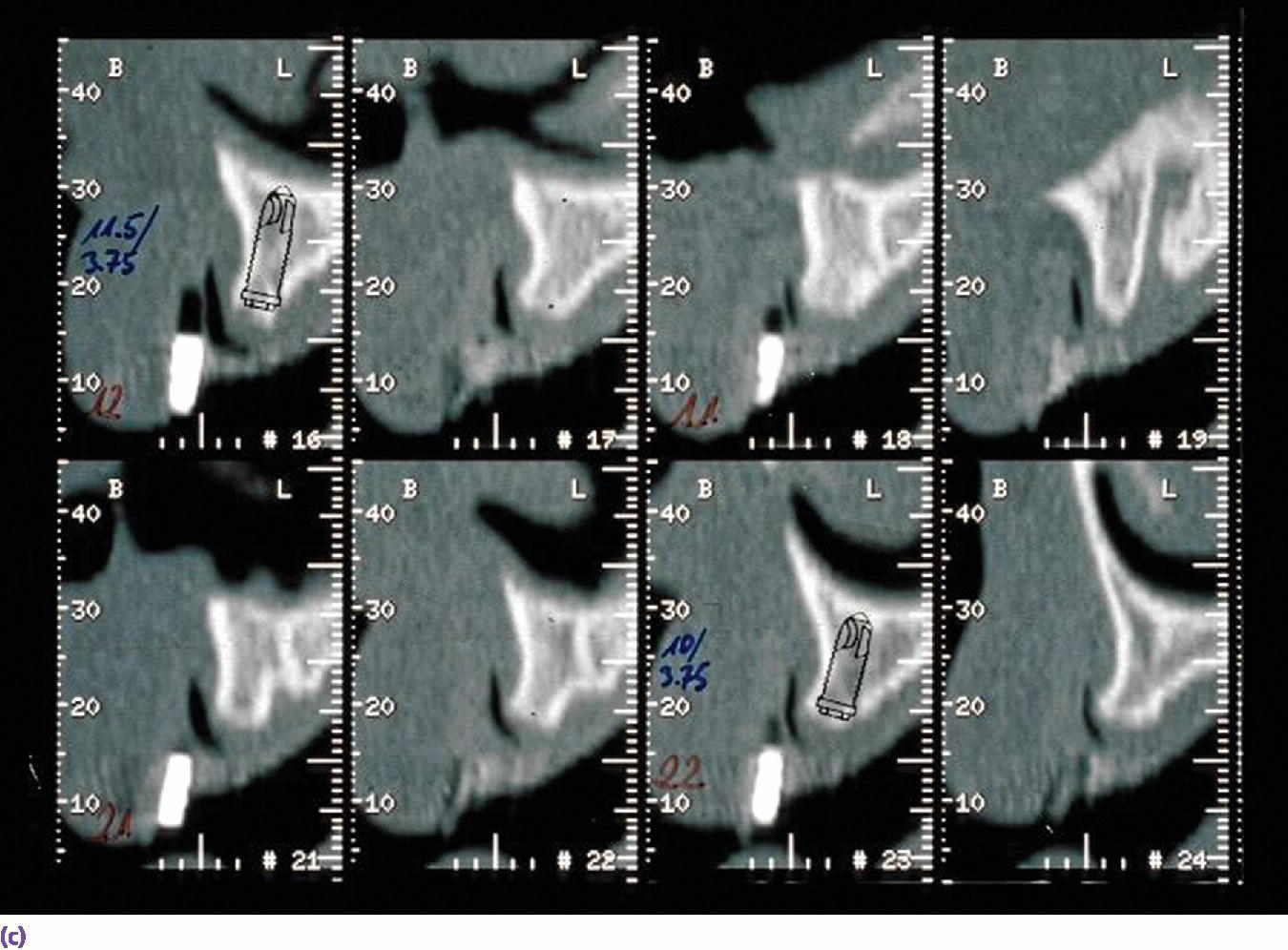
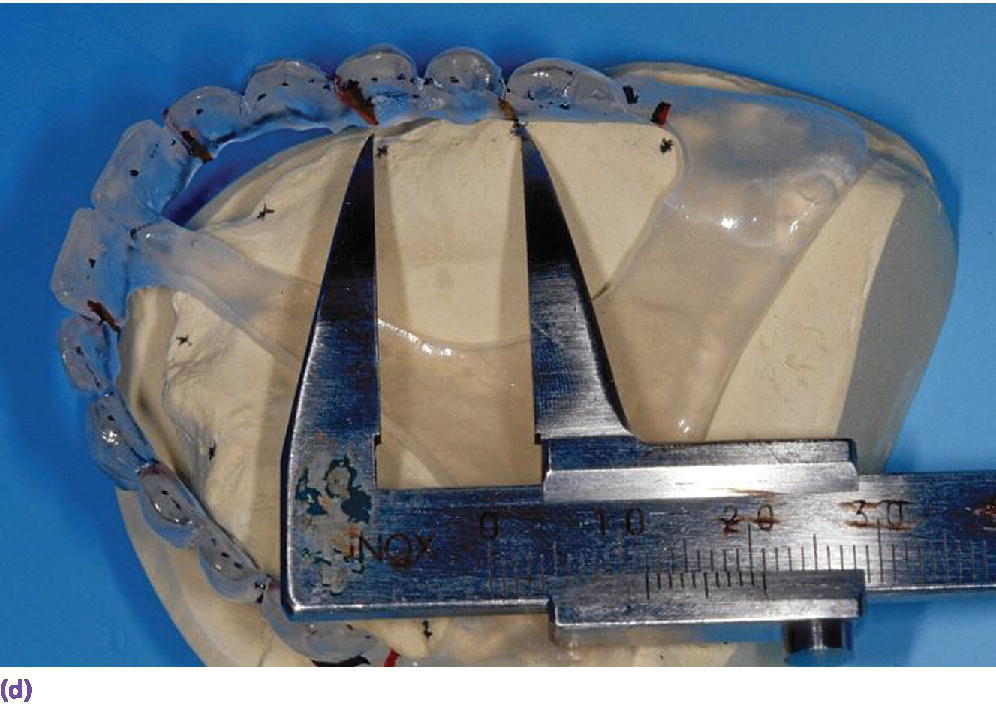
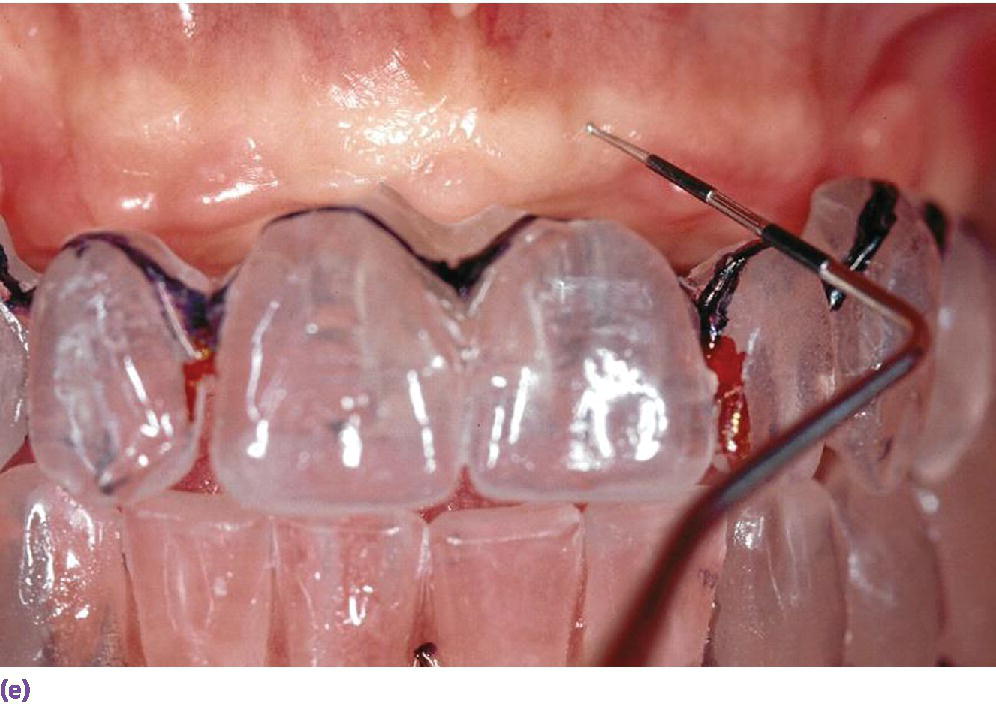
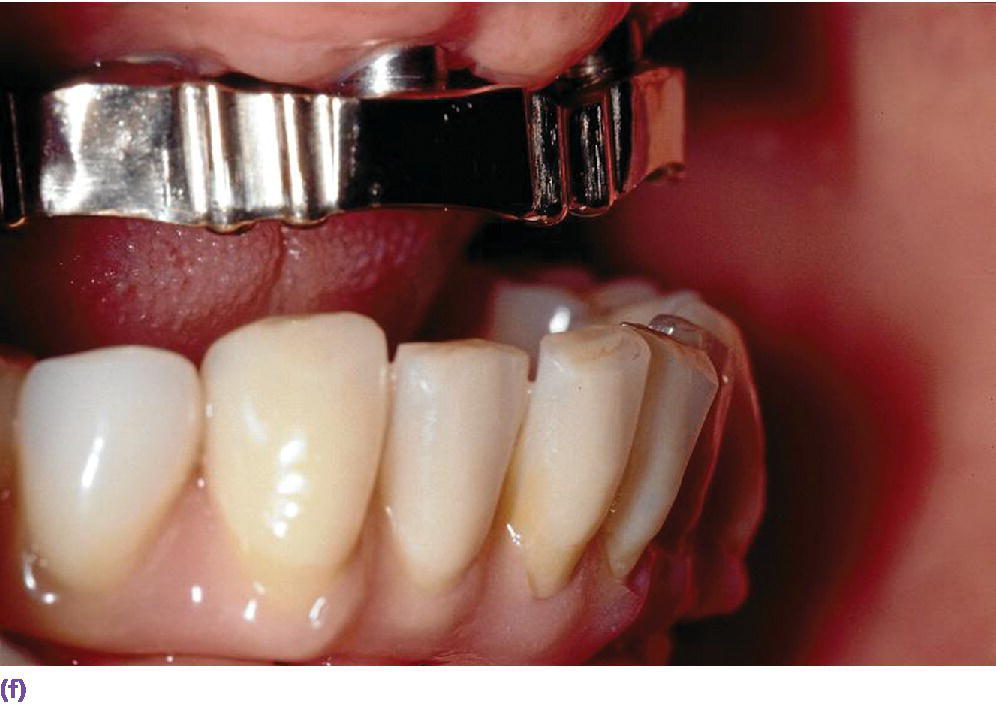


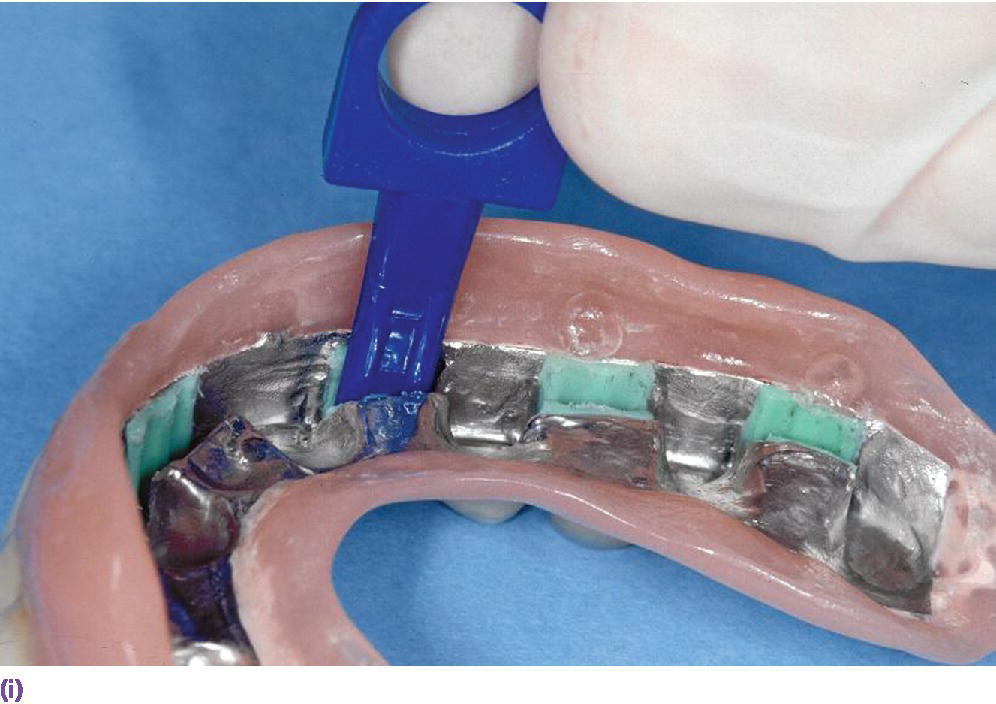
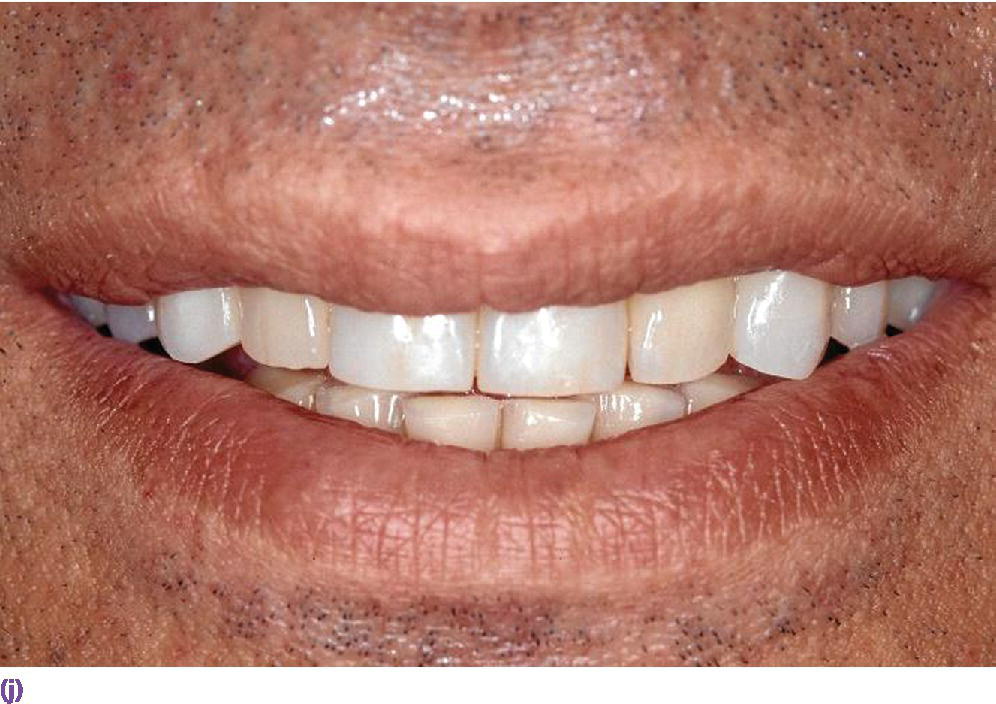
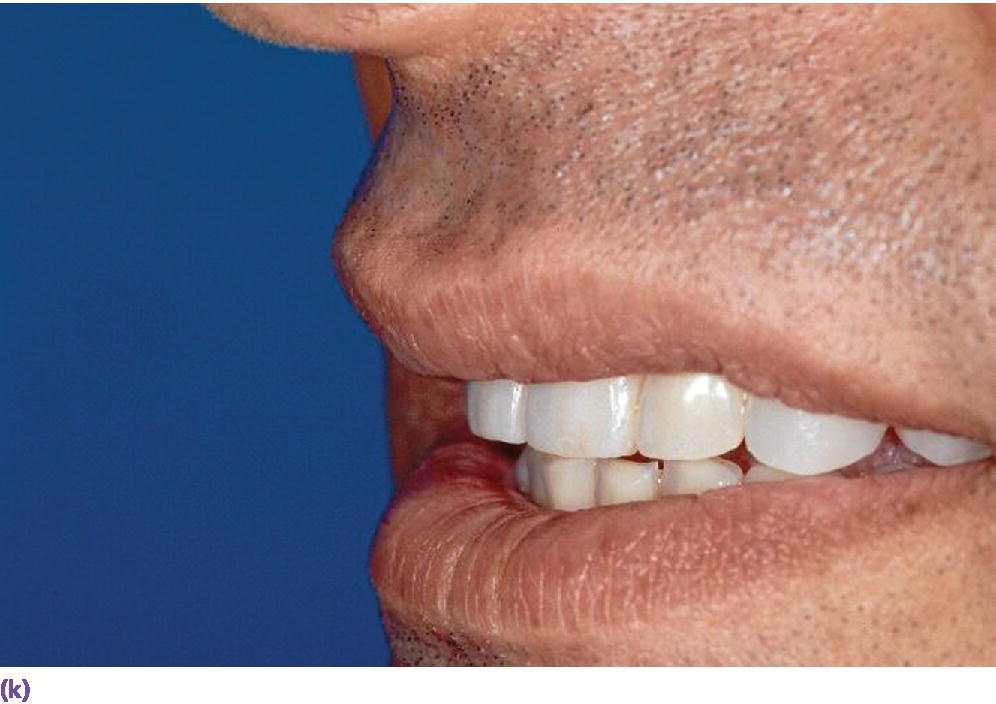
Figure 17.5 (a) Set‐up keyed to produce a transparent template. (b) Template mounted in a surveyor to determine a similar path of insertion and to mill the holes for titanium markers. (c) Reformatted CT scan illustrates large discrepancy between ideal tooth position (indicated by titanium markers) and underlying maxillary bone. (d) Radiographic template modified for application during implant placement. (e) Template try‐in illustrating discrepancy between alveolar ridge and diagnostic tooth position in the horizontal dimension. (f) IOD retention with casted gold bar with Bredent Vario soft elements. (g) IOD in place. (h) Anterior view with buccal flange. (i) Matrix exchange in the metal reinforcement. (j) Anterior view. (k) Side view. (j) and (k) illustrate adequate soft tissue support.
(Technician: Fernando Pasamontes, Zug.)
The transverse cross‐sections from the 3‐D radiographs are analyzed to determine if the available bone allows for implant placement at an ideal angulation.19
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


