16
Medical emergencies and their management
- Avoidance of a medical emergency
- The ABCDE approach to management of the sick patient
- Medical emergencies and their management
- Basic life support in adults and children
Introduction
Medical emergencies by their very nature can occur at any time, without warning and not necessarily in the clinical environment. It is therefore essential to be able to recognise the nature of an emergency as soon as it occurs and to have the knowledge, proficiency and confidence to be able to undertake the appropriate remedial action.
The General Dental Council (GDC, 2009) state that hygienists and dental therapists must:
- Be competent at carrying out resuscitation techniques.
- Have knowledge of how to identify medical emergencies and provide immediate management of anaphylactic reaction, hypoglycaemia, upper respiratory obstruction, cardiac arrest, fits, vasovagal attack, inhalation or ingestion of foreign bodies, and haemorrhage.
Management considerations
Dental therapists and hygienists treat patients of all ages and it is inevitable that some of these patients will have significant medical conditions and take medication, both of which may necessitate a modification to dental treatment. In addition many patients will experience anxiety associated with their treatment. It is to be expected that acute medical conditions will occur in a dental practice, albeit rarely. It is worth remembering that friends or family who often accompany patients, other visitors to the practice and staff may become unwell and require urgent attention. Medical emergencies can therefore occur anywhere on the premises, not just in the surgery. It is essential that all dental health care workers should have the knowledge and skills to recognise and provide appropriate immediate medical care for emergencies that might present in dental practice. In some instances this will require the provision of life saving measures prior to the arrival of specialist help.
A medical emergency can be described as a situation in which a patient’s life may be at risk. The medical emergencies that are likely to be encountered in dental practice are shown in Table 16.1. This list is not exhaustive but it represents the commonly accepted conditions for which the dental team should be prepared. The individual management strategies used for these conditions are discussed in more detail later in this chapter.
Table 16.1 Medical emergencies that can occur in the dental surgery.
| • Vasovagal attack (faint/syncope) | • Myocardial infarction |
| • Hyperventilation (panic attack) | • Anaphylaxis |
| • Epileptic seizures | • Airway obstruction (including chocking) |
| • Hypoglycaemia | • Respiratory arrest |
| • Asthma attack | • Cardiac arrest |
| • Angina | • Adrenal crisis |
Table 16.2 Emergency equipment and drugs required in the dental surgerya.
| Equipment | Drugs |
| Pocket mask with one-way valve and oxygen inlet Self inflating 1 litre bag, valve and mask with reservoir in various sizes with appropriate tubing to connect to the oxygen (face masks should be in variety of sizes for children and adults) Oropharyngeal airwaysb (sizes 1,2,3,4) Oxygen therapy masks with tubing and appropriate connectors for oxygen cylinder Sterile syringes and needles to deliver emergency drugs by IM routes Independently powered portable suction apparatus with wide bore aspiration tips. Spacer device for inhaled bronchodilators (eg salbutamol) Automated blood glucose measurement device Automated external defibrillator Additional equipment and emergency drugs Pulse oximeterc Blood pressure monitorc |
Oxygen (portable) with pressure reduction valve and flowmeter Epinephrine (adrenaline) Glyceryl trinitrate (GTN) Aspirin Glucose Glucagon Salbutamol inhaler Midazolam |
a Equipment should be free from natural rubber latex and resuscitation equipment must be available in suitable sizes for children. Drugs must be available in preparations free from natural rubber latex, whenever possible.
b These are also referred to as Guedel’s airway.
c Essential in a practice that carries out IV sedation. (Adapted from the Resuscitation Council (UK) Guidance www.resus.org.uk 2010.)
It is the professional responsibility of hygienists and therapists to ensure that:
- They know the location of, and have easy and prompt access to, all emergency equipment and drugs (see Table 16.2).
- The equipment and drugs conform to contemporaneous standards recommended by respected bodies.
- All equipment is well maintained and all drugs are checked regularly and replaced prior to their expiry date.
- They are trained regularly in the use of the above.
- Regular ‘in-practice’ simulation of the management of medical problems including the preparation and administration of emergency drugs. This is in addition to training in cardiopulmonary resuscitation (CPR).
Regular in-house training in cardiopulmonary resuscitation is mandatory for the dental team. These sessions can be easily modified to include a rehearsal of managing other acute medical emergencies that do not necessarily need to progress to a cardiorespiratory arrest, although this remains a possible outcome. Several scenarios can be devised around an unwell patient who has the potential to progressively deteriorate; such as a patient with angina who may develop severe chest pains or a patient who experiences breathing problems. Regular rehearsal identifies problems that can then be rectified in a non-judgemental and constructive manner. Simulation training undertaken in a familiar working environment allows staff to clearly understand their role and the role of other members of the team, so helping to reduce confusion and panic when faced with a real emergency.
It is also important for members of the team to be cognisant with the different methods of preparation of the emergency drugs. This extends from turning on the oxygen supply and attaching the different types of face masks, to the opening of drug ampoules, and the drawing up and mixing of medications presented as powders with solvents (e.g. glucagon). Epinephrine (adrenaline) is available in several presentations from glass ampoules to preloaded syringes and staff should be confident in preparing the drugs available in their workplace. Preloaded syringes are more user friendly, although there are still training issues to be addressed in assembling many of these presentations. It is not unusual for hygienists and therapists to work in more than one practice and therefore they may need to be familiar with a wider range of drug presentations.
It is imperative that training exercises are aimed at team building and therefore should be non-threatening. Consideration should be given to the management of patients who have collapsed in areas other than the dental chair or surgery. Toilets, with their confined space can be particularly awkward and problematic. Locked toilet doors should be able to be opened from the outside so that emergency access can be obtained. Formal courses using scenario training for medical emergencies are provided by some postgraduate Deaneries. Immediate life support (ILS) courses are organised by the Resuscitation Council (UK). The authors consider it best practice for all clinical members of the dental team to receive annual training to ILS standards.
When first commencing work in a new practice it should be standard protocol to identify where the emergency drugs and equipment are kept. You should be satisfied that these are adequate and comply with current guidance. Participation in team training for emergencies should ideally be part of the induction process when starting in a new place of work.
The role of the hygienist/therapist
The General Dental Council (GDC) states that dental hygienists and therapists should:
- Be competent at carrying out resuscitation techniques.
- Have knowledge of how to identify medical emergencies and provide immediate management of anaphylactic reaction, hypoglycaemia, upper respiratory tract obstruction, cardiac arrest, fits, vasovagal attack, inhalation or ingestion of foreign bodies, and haemorrhage (GDC, 2009).
Hygienists and therapists are capable of independent practice. When the dentist is present it is probable that he or she will assume the role of team leader in a medical emergency; although another more experienced clinical member of the team may assume this role. In the event of an emergency it is hoped that those present would work as a team, with many of the staff making valuable contributions to the management of the patient. However, a dentist may not be on the premises and a therapist/hygienist may be the most senior person and lead the team, in fact you may be the only staff member present. It is therefore important that the hygienist/therapist understands their role fully in a medical crisis and has a clear idea of what actions they would be prepared to carry out. The guidance given by the GDC clearly indicates that you would be expected to perform CPR; it would be unacceptable for any clinical member of the dental team not to attempt CPR on a patient in cardiorespiratory arrest. There remains some uncertainty from the guidance given by the GDC as to what would be expected from a therapist/hygienist with regard to the administration of drugs. Does how to provide mean that you should provide? It is the authors’ opinion that hygienists and therapists should be able to administer first line drugs for the patient provided that they have received appropriate training. Therefore in this chapter it is assumed that the hygienist or therapist would carry out essential primary treatment in a medical emergency. This includes the use of the following drugs: oxygen, epinephrine (adrenaline), glucose, glucagon, midazolam, glyceryl trinitrate, aspirin and salbutamol. Further post-qualification training may result in new drugs being added to this list.
It must be appreciated that the overwhelming majority of clinical dental personnel are uncomfortable in managing a medical emergency and are unlikely to feel confident in administering emergency drugs, other than oxygen. This is because their experience is likely to be based solely upon their academic knowledge and clinical skills acquired during simulation training (hence its importance). Other than the management of faints, most dental staff will have little (if any) experience of managing medical emergencies for real.
Avoidance of a medical emergency
Whilst it is accepted that all members of the dental team should be prepared to manage a medical crisis, steps should always be taken to try and prevent an acute condition from arising. In essence this involves:
- Having an accurate contemporaneous record of the patient’s medical and drug history.
- Having a realistic and appropriate treatment plan.
- Identifying potential medical problems.
- Observing the patient.
- Rehearsing the systematic approach used for the assessment of the sick patient; as described by the Resuscitation Council (UK).
Prior to treating any patient a detailed medical and drug history is essential, and this should be updated at each treatment session. Knowledge of a patient’s medical status is part of risk assessment. Details of any medical history previously recorded in the clinical records should be read thoroughly and evaluated before the patient enters the surgery. When treating a patient with a significant medical and drug history all staff involved in the care of the patient should know of, and understand, the relevance (if any) of the patient’s current and past medical conditions. It is always prudent to ask patients if they have taken their medication as usual. Occasionally a patient will have the misconception that they should stop their regular medication on the day of dental treatment. When this occurs the therapist/hygienist should seek advice from the dentist to see if it is safe to proceed with operative treatment. In the absence of any dentists, a member of The Medicines Information Service, who advise on drug therapy relating to dentistry, can be obtained by telephoning 0151 794 8206 (in the UK).
Patients (and sometimes guardians or carers) do not always disclose an accurate medical and drug history. When important questions remain unanswered or there appears to be inconsistencies or conflicting information then clarification should be sought from the patient’s medical practitioner. Operative treatment should not be undertaken in the absence of a reliable medical history.
When a patient declares a significant medical condition it is often necessary to ask further in depth questions in order to assess potential risks. An example of this is in patients who have epilepsy – it is essential to know how well their epilepsy is controlled and when they had their last seizure. The type of epilepsy should be documented and the patient asked for a description of their seizures, it is also helpful to know if they have warnings prior to a seizure. It is important to identify if they have ever gone into status epilepticus, and if so, how often. Any triggers that have been identified as precipitating a seizure should be documented in the records. Whilst all types of epilepsy should be recorded, a generalised seizure generates most concern due to the greatest possibility of injury and post-seizure complications. Patients who have frequent seizures should be asked for details about their recovery, for example some patients sleep after a seizure. Ask this group of patients how they would like to be managed post-seizure.
Treatment planning should be sensible, realistic and the medical and social needs of each patient should be taken into account. The timing and duration of appointments are important when treating patients with chronic disease. Table 16.3 highlights some factors that will influence treatment planning. Patients with diabetes should not be kept waiting and ideally treatment should not interfere with the timing of the patient’s carbohydrate intake or administration of their medication. Patients who have debilitating illnesses and who get tired easily should have their dental appointments at a time that is most suited to their lifestyle. Sometimes carers and patients who have severe disabilities are unable to attend for early morning appointments. Patients who receive kidney dialysis should usually be treated on a day when they are not dialysed. A patient who has had a myocardial infarction within the last 6 months should only undergo simple emergency dental treatment due to an increased risk of dysrhythmias; routine, elective treatment should be deferred.
Table 16.3 Considerations when treating patients with a medical history.
When assessing a patient’s health record it is helpful to consider the following possibilities:
|
It is important that therapists and hygienists recognise dental anxiety in their patients. This is of paramount importance in those who have serious medical conditions that are exacerbated by stress (for example angina, hypertension or epilepsy). This group of patients should be asked if they are made anxious by any aspect of dental treatment because pain and effective anxiety control is essential to avoid a crisis. It may be safer to treat this cohort of anxious patients under sedation. Not all patients are suitable for dental treatment in primary care. It is often necessary to refer patients who have severe unstable medical conditions to a specialist unit when operative dental treatment is required. If there is uncertainty about the safety of managing a patient in primary care advice should be sought.
It is always necessary to clinically observe a patient during dental treatment; careful observation will allow early recognition and prompt management of the unwell or deteriorating patient. Table 16.4 lists sored.
Table 16.4 Clinical monitoring.
| Level of consciousness – Assess the patient’s response to questions and commands and also their level of co-operation. |
| Respiration – At rest, respiration should be regular, effortless and quiet; breath sounds should not be obvious. When there is obstruction on inspiration, increased respiratory signs are seen such as excessive abdominal movement. The number of breaths can be counted over a 30 second period and the rate calculated for 1 minute. The respiration rate should be around 14–20 breaths per minute for an adult, but may be as high as 30 in a child. |
| Pulse – Assess the rate, regularity and quality. A pulse results from the intra-arterial pressure transmitted to arteries by the contraction of the left ventricle. A pulse represents the heart rate. The radial and brachial are the commonly used superficial pulses but the carotid and femoral pulses are the major pulses used in the assessment of an unconscious patient. In a baby, however, the brachial pulse is used because the neck is poorly developed making the carotid pulse difficult to feel. An average resting pulse rate for an adult is around 80 bpm (range 60–100). Children’s pulse rates are faster. When taking a radial pulse you should place your 2nd and 3rd fingers in the hollow immediately above the wrist creases at the base of the thumb, and press lightly. You should not use your thumb to record a pulse because it has a pulse of its own. Assess the rate (over a minimum period of 30 seconds) and calculate the value for 1 minute. |
| Colour of the patient – Assess the pallor of the face, the colour of the fingers. Visual signs of central cyanosis will only be detected by a skilled operator when the arterial oxygen saturation falls to below 85%. Hypoxia is therefore not clinically noticeable in the early stages and if hypoxia is a concern then the use of a pulse oximeter may be advisable. Patients will normally have oxygen saturation levels of 97–100%. |
| General mood, demeanour, composure and body language – Ascertain if the patient is relaxed or agitated. When a patient is receiving dental treatment the operator and nurse should be aware of how comfortable or restless the patient is. A restless patient may fidget and appear tense. |
It is rare for a medical emergency to occur without warning. When treating a patient there will usually be signs and/or symptoms, which indicate a deteriorating condition. When a patient looks unduly pale, flushed or ill ask them if they are feeling unwell. It may just be that they had a disturbed sleep, have missed a meal or are recovering from an illness. Such information is helpful in evaluating the patient. Patients who are clearly unwell should have their dental treatment deferred. Early recognition of a distressed or unwell patient can sometimes prevent an acute incident or prepare the dental team for prompt action in the early stages of a crisis. Knowing when to summon expert assistance is also important. A structured and logical approach to assessing a sick patient is invaluable in the early recognition and management of an unwell patient and one such approach is described in the next section.
Assessment of the sick patient using the ‘ABCDE’ approach
It is helpful to take an overview of the assessment and management of the unwell patient because early recognition of a sick patient may prevent an emergency. The Resuscitation Council (UK) have issued guidance that provides the dental team with a systematic and rational approach to managing the unwell patient, The principles employed can also be used in all medical emergencies that may be encountered in the dental surgery and is equally applicable if the patient is conscious or unconscious. The ‘ABCDE’approach is summarised in Table 16.5. The acronym is an aide-mémoire for Airway, Breathing, Circulation, Disability, Exposure. Information obtained during this assessment will assist you in deciding whether or not to call the emergency services. If any life threatening problems are identified they are treated immediately before moving onto the next part of the assessment. A brief description of the methodology will be given below, but more detail relating it to specific medical emergencies can be found under each condition.
Table 16.5 The ‘ABCDE’ approach to assessing the sick patient.
| Assess | Consider |
| Airway patency of the airway |
Removing debris Improving airway with head tilt/chin lift, jaw thrust Airway adjuncts Oxygen |
| Breathing rate and depth of respiration associated sounds/noises use of accessory muscles |
Oxygen Chair position Salbutamol for asthma Re-breathing if hyperventilation |
| Circulation rate, strength, regularity of pulse capillary refill and blood pressure |
Chair position GTN if you suspect angina Aspirin if you suspect an MI |
| Disability level of consciousness (AVPU) response of pupils to light blood glucose levels |
if unconscious lie them flat, consider the recovery position if they are breathing spontaneously Glucose/glucagon for hypoglycaemia |
| Exposure skin rashes ankle oedema |
Adrenaline if anaphylaxis Placing a blanket around the patient |
When you have recognised that a patient appears to be unwell you should stop all dental treatment, stay calm and ensure that you and the dental team are safe. You then want to assess the level of consciousness of the patient; this can be done simply by asking them ‘if they feel ok’. Depending on their response you may wish to call for a colleague to help you.
Airway
A person must have an open airway to allow oxygen to enter the lungs, so the first step in effective management is to assess the patency of the upper airway – the patency is obvious if the patient is talking, however, if the patient is unconscious, are there any obvious obstructions such as fluid, vomit or the tongue?
Breathing
Look, listen and feel for signs of respiratory distress. Is breathing noisy, are accessory muscles (neck and abdominal muscles) being used? Is the patient blue? What is the rate of respiration? A breathing rate of 12–20 breaths per minute is a reasonable range for an adult. Are both right and left sides of the chest rising and falling with every breath? Patients having an asthma attack (recognised by an expiratory wheeze) require a bronchodilator such as salbutamol.
Patients who have respiratory distress that is not relieved by airway manoeuvres, oxygen or bronchodilators need urgent medical help.
If there is no breathing then you proceed to the algorithm for respiratory arrest.
Circulation
An efficient circulation is essential to distribute oxygenated blood from the lungs to the vital organs, thus maintaining the cardiac output. Circulation can be assessed by looking at the colour of the patient, by feeling the pulse and noting if the extremities, such as the hands, are cold or warm to touch. The pulse may be more easily detected if a central point is used. A simple and quick test, the capillary refill time, gives an indication of how good the blood supply is to the peripheral tissues. This test consist of applying pressure for around 5 seconds to a finger tip (positioned at heart level or just above) in order to cause blanching. The pressure is then released and the time taken for the colour of the surrounding skin to return to normal is recorded. The normal capillary refill time is less than 2 seconds; a longer time suggests poor peripheral circulation.
If a patient has a low pulse rate they should be placed flat, preferably with the legs raised to improve venous return. If the pulse rate remains weak, slow or irregular then further medical help is needed. Patients with breathing and cardiac problems may not feel comfortable or well when they are put in a supine position as it may compromise their cardiorespiratory function. It is essential that these patients, when conscious, are put in a position in which they feel comfortable. Poor pulse rates are suggestive of a low blood pressure and it would be helpful to measure blood pressure if equipment is available.
Disability
Under disability the clinician should assess the patient’s level of consciousness, see if their pupils are equally responsive to light and measure blood glucose. Unconscious patients should be monitored in the recovery position whenever possible.
A quick method of assessing a person’s level of consciousness is the AVPU system, where:
A = Alert.
V = response to Vocal stimuli.
P = response to Painful stimuli.
U = Unresponsive to stimuli.
The level of consciousness may be assessed at the start of the assessment when you are assessing the airway.
Exposure
It is helpful to quickly check if the patient has a rash or swollen ankles. A patient in shock will quickly feel cold so a blanket should be placed around them to minimise heat loss.
The unwell patient should be continually monitored using the above approach until help arrives.
Medical emergencies
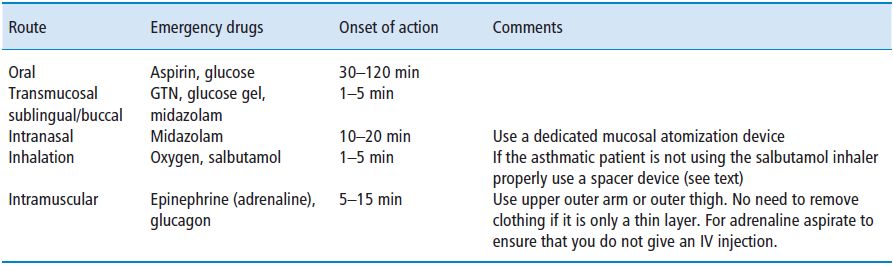
A summary of the use of emergency drugs is given in Table 16.6 and a separate chart for the administration routes for emergency drugs is given in Table 16.7.
Table 16.6 Indications and mechanism of action of drugs used in medical emergenciesa.
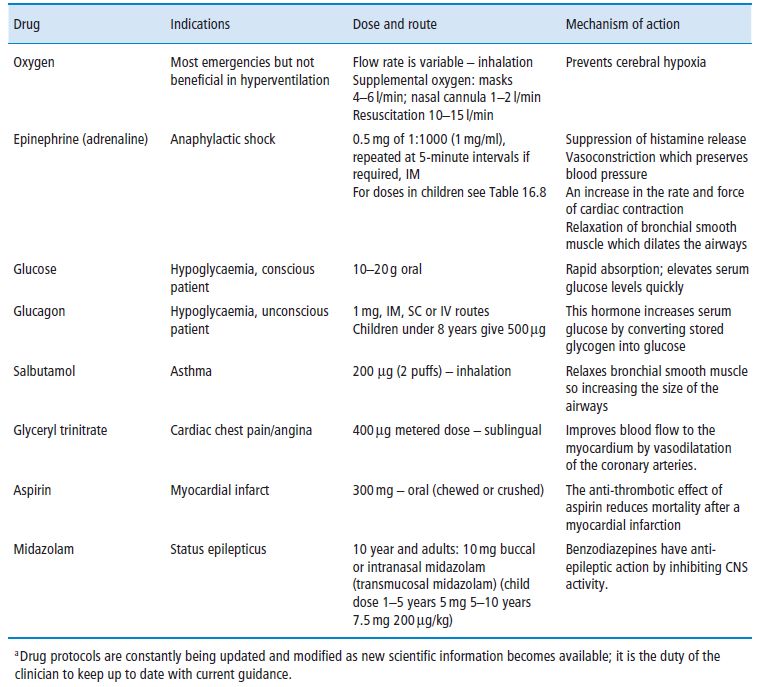
Table 16.7 Routes of drug administration important in medical emergencies.
Airway obstruction
The airway may be obstructed by a foreign body (e.g. a tooth, food or denture), blood, vomitus, oropharyngeal oedema, laryngospasm and bronchospasm.
Inhaled foreign body
In dental practice there is always a risk of foreign bodies such as pieces of tooth or parts of restorations being dislodged into the oropharynx and then being inhaled or ingested. If the foreign body has been ingested, it will usually travel through the gastrointestinal tract and be passed normally. If it is inhaled it may stimulate a cough reflex, or indeed choking if it is large enough. A small object can pass directly into the lower airway where it can cause a lung abscess if not retrieved. The best treatment is prevention, and the use of dental dam for restorative treatment is advised. Should an object be lost and the patient is not coughing or choking then the appropriate management is as follows:
- Check the patient’s mouth and clothing thoroughly and the filter/trap of the aspirator.
- If the patient is lying flat ask them to turn onto their side and lower the chair to a ‘head down’ position; this encourages gravity to bring the object back into the mouth.
If the object cannot be located, inform the patient and contact the nearest A&E department for chest and abdominal X-rays. If the object is located in the respiratory tract the hospital will arrange removal as necessary.
Choking
The conscious patient
Airway obstruction in a conscious patient is easily diagnosed. Typically the person will appear distressed, coughing and have difficulty in breathing. They will usually point towards their neck or throat region to indicate the source of the problem. Choking can occur in the dental c/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


