Gingival Enlargement
With the use of the criteria of location and distribution, gingival enlargement is designated as follows:
• Localized: Limited to the gingiva adjacent to a single tooth or group of teeth
• Generalized: Involving the gingiva throughout the mouth
• Marginal: Confined to the marginal gingiva
• Papillary: Confined to the interdental papilla
• Diffuse: Involving the marginal and attached gingivae and papillae
• Discrete: An isolated sessile or a pedunculated, tumorlike enlargement
The degree of gingival enlargement can be scored as follows16:
Inflammatory Enlargement
Chronic Inflammatory Enlargement
Clinical Features.
Chronic inflammatory gingival enlargement originates as a slight ballooning of the interdental papilla and marginal gingiva. In the early stages, it produces a life-preserver–shaped bulge around the involved teeth. This bulge can increase in size until it covers part of the crowns. The enlargement may be localized or generalized; it progresses slowly and painlessly, unless it is complicated by acute infection or trauma (Figures 16-1 and 16-2).
Gingival Changes Associated with Mouth Breathing.
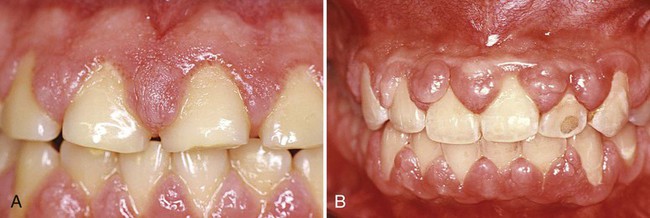
Gingivitis and gingival enlargement are often seen in patients who are mouth breathers. The gingiva appears red and edematous, with a diffuse surface shininess of the exposed area. The maxillary anterior region is the common site of such involvement. In many cases, the altered gingiva is clearly demarcated from the adjacent unexposed normal gingiva (Figure 16-4). The exact manner in which mouth breathing affects gingival changes has not been demonstrated. Its harmful effect is generally attributed to irritation from surface dehydration. However, comparable changes could not be produced by air drying the gingiva of experimental animals.66
Acute Inflammatory Enlargement
Gingival Abscess.
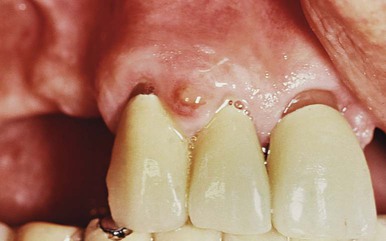
A gingival abscess is a localized, painful, rapidly expanding lesion that usually has a sudden onset (Figure 16-5). It is generally limited to the marginal gingiva or the interdental papilla. In its early stages, it appears as a red swelling with a smooth, shiny surface. Within 24 to 48 hours, the lesion usually becomes fluctuant and pointed, with a surface orifice from which a purulent exudate may be expressed. The adjacent teeth are often sensitive to percussion. If permitted to progress, the lesion generally ruptures spontaneously.
Drug-Induced Gingival Enlargement
Clinical and microscopic features of the enlargements caused by the different drugs are similar.19,86 These are presented first, followed by a description of the particular features of each drug.
General Information
Clinical Features.
The growth starts as a painless, beadlike enlargement of the interdental papilla that then extends to the facial and lingual gingival margins (Figure 16-6). As the condition progresses, the marginal and papillary enlargements unite, and they may develop into a massive tissue fold that covers a considerable portion of the crowns; this may interfere with occlusion (Figure 16-7).


The resultant enlargement then becomes a combination of the increase in size caused by the drug and the complicating inflammation caused by bacteria. Secondary inflammatory changes not only add to the size of the lesion caused by the drug but also produce a red or bluish-red discoloration, obliterate the lobulated surface demarcations, and increase bleeding tendency (Figure 16-8).

The enlargement is usually generalized throughout the mouth, but it is more severe in the maxillary and mandibular anterior regions. It occurs in areas in which teeth are present (not in edentulous spaces), and the enlargement disappears in areas from which teeth have been extracted. Hyperplasia of the mucosa in edentulous mouths has been reported but is rare.26,27
Drug-induced enlargement may occur in mouths with little or no plaque, and it may be absent in mouths with abundant deposits. However, some investigators believe that inflammation is a prerequisite for development of the enlargement, which therefore could be prevented by plaque removal and fastidious oral hygiene.22,37,78,101 Oral hygiene by means of toothbrushing or the use of a chlorhexidine toothpaste90 reduces the inflammation but does not lessen or prevent the overgrowth. Hassell and colleagues42,44 have hypothesized that, in noninflamed gingiva, fibroblasts are less active or even quiescent and do not respond to circulating phenytoin, whereas fibroblasts within inflamed tissue are in an active state as a result of the inflammatory mediators and the endogenous growth factors that are present.
A genetic predisposition is a suspected factor45,83 for determining whether a person treated with phenytoin will develop gingival enlargement.
The enlargement is chronic, and it slowly increases in size. Even if it is surgically removed, it recurs. Spontaneous disappearance occurs within a few months after the discontinuation of the drug. See Chapter 58 for more information about the treatment of gingival enlargements, including the substitution of drugs that do not induce gingival overgrowth.
Anticonvulsants
The first drug-induced gingival enlargements reported were those produced by phenytoin (Dilantin). Dilantin is a hydantoin that was introduced by Merritt and Putnam68 in 1938 for the treatment of all forms of epilepsy, except petit mal seizures. Shortly thereafter, its relationship with gingival enlargement was reported.35,57
Other hydantoins that are known to induce gingival enlargement are ethotoin (Peganone) and mephenytoin (Mesantoin). Other anticonvulsants that have the same side effect are the succinimides (ethosuximide [Zarontin], methsuximide [Celontin]) and valproic acid (Depakene).38
Gingival enlargement occurs in about 50% of patients receiving the drug,109 although different authors have reported incidences from 3% to 84.5%.2,35,79 It occurs more often in younger patients.5 Its occurrence and severity are not necessarily related to the dosage after a threshold level has been exceeded.96 Phenytoin appears in the saliva. There is no consensus, however, regarding whether the severity of the overgrowth is related to the levels of phenytoin in plasma or saliva.2,5,6,41,115 Some reports indicate a relationship between the drug dosage and the degree of gingival overgrowth.54,58
Tissue culture experiments indicate that phenytoin stimulates the proliferation of fibroblast-like cells97 and epithelium.98 Two analogs of phenytoin (1-allyl-5-phenylhydantoinate and 5-methyl 5-phenylhydantoinate) have a similar effect on fibroblast-like cells.98 Fibroblasts from a phenytoin-induced gingival overgrowth show increased synthesis of sulfated glycosaminoglycans in vitro.53 Phenytoin may induce a decrease in collagen degradation as a result of the production of an inactive fibroblastic collagenase.42
Experimental attempts to induce gingival enlargement with phenytoin administration in laboratory animals have only been successful in the cat,50 the ferret, and the Macaca speciosa monkey.103 In experimental animals, phenytoin causes gingival enlargement that is independent of local inflammation.
In cats, one of the metabolic products of phenytoin is 5-(parahydroxyphenyl)-5-phenylhydantoin; the administration of this metabolite to cats also induces gingival enlargement in some cases. This led Hassell and colleagues43 to hypothesize that gingival enlargement may result from the genetically determined ability or inability of the host to deal effectively with the prolonged administration of phenytoin.
The systemic administration of phenytoin accelerates the healing of gingival wounds in nonepileptic humans100 and increases the tensile strength of healing abdominal wounds in rats.25,99 The administration of phenytoin may precipitate megaloblastic anemia65 and folic acid deficiency.104
Immunosuppressants
Cyclosporine is a potent immunosuppressive agent that is used to prevent organ transplant rejection and to treat several diseases of autoimmune origin.20 Its exact mechanism of action is not well known, but it appears to selectively and reversibly inhibit helper T cells, which play a role in cellular and humoral immune responses. Cyclosporine A (Sandimmune, Neoral) is administered intravenously or by mouth, and dosages of more than 500 mg/day have been reported to induce gingival overgrowth.24
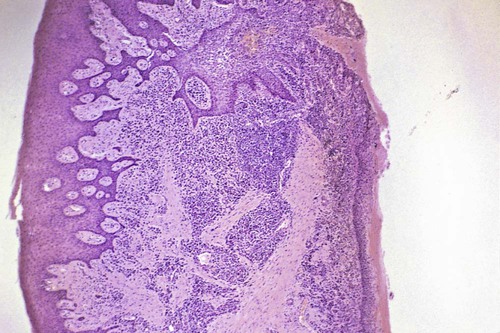
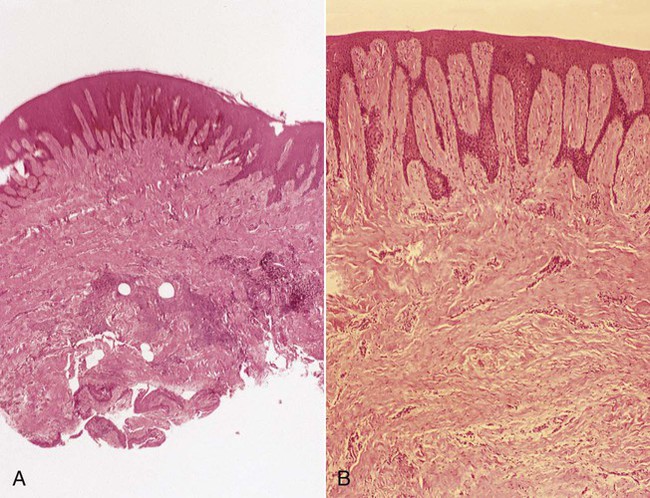
Cyclosporine-induced gingival enlargement is more vascularized than phenytoin enlargement (Figures 16-10 and 16-11).85,91,117 Its occurrence varies, according to different studies, from 25% to 70%.88 It affects children more frequently, and its magnitude appears to be related more to the plasma concentration than to the patient’s periodontal status.95 Gingival enlargement is greater in patients who are medicated with both cyclosporine and calcium channel blockers.101,111,112
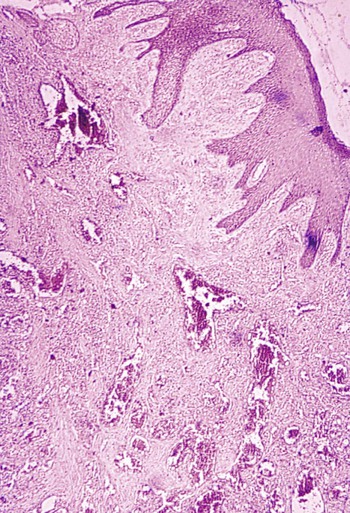
The microscopic finding of many plasma cells plus the presence of an abundant amorphous extracellular substance has suggested that the enlargement is a hypersensitivity response to the cyclosporine.67
In experimental animals (rats), the oral administration of cyclosporine was also reported to induce the abundant formation of new cementum.4
In addition to gingival enlargement, cyclosporine induces other major side effects such as nephrotoxicity, hypertension, and hypertrichosis. Another immunosuppressive drug, tacrolimus, has been used effectively; it is also nephrotoxic, but it results in much less severe hypertension, hypertrichosis, and gingival overgrowth.7,70,102
Calcium Channel Blockers
These drugs are the dihydropyridine derivatives (amlodipine [Lotrel, Norvasc], felodipine [Plendil], nicardipine [Cardene], nifedipine [Adalat, Procardia]); the benzothiazine derivatives (diltiazem [Cardizem, Dilacor XR, Tiazac]); and the phenylalkylamine derivatives (verapamil [Calan, Isoptin, Verelan, Covera HS]).38
Some of these drugs can induce gingival enlargement. Nifedipine, which is one of the most often used,39,62,64,76 induces gingival enlargement in 20% of patients.8 Diltiazem, felodipine, nitrendipine, and verapamil also induce gingival enlargement.14,46 The dihydropyridine derivative isradipine can replace nifedipine in some cases; it does not induce gingival overgrowth.114
Nifedipine is also used with cyclosporine in kidney transplant recipients, and the combined use of both drugs induces larger overgrowths.13 Nifedipine gingival enlargement has been induced experimentally in rats, where it appears to be dose dependent32; in humans, however, this dose dependency is not clear. One report indicates that nifedipine increases the risk of periodontal destruction in patients with type 2 diabetes mellitus.63
Idiopathic Gingival Enlargement
General Information
Clinical Features.
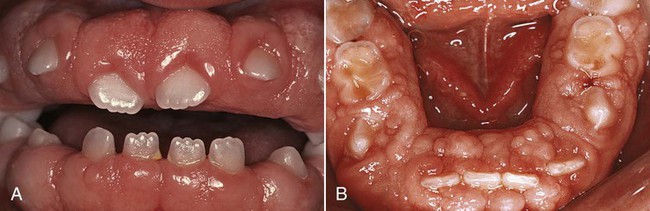
The enlargement affects the attached gingiva as well as the gingival margin and the interdental papillae. This is in contrast with phenytoin-induced overgrowth, which is often limited to the gingival margin and the interdental papillae (see Figure 16-6). The facial and lingual surfaces of the mandible and maxilla are generally affected, but the involvement may be limited to either jaw. The enlarged gingiva is pink, firm, and almost leathery in consistency, and it has a characteristic minutely pebbled surface (Figure 16-12). In severe cases, the teeth are almost completely covered, and the enlargement projects into the oral vestibule. The jaws appear distorted as a result of the bulbous enlargement of the gingiva. Secondary inflammatory changes are common at the gingival margin.
Etiology.
The cause is unknown, and thus the condition is designated as “idiopathic.” Some cases have a hereditary basis,28,118,119 but the genetic mechanisms involved are not well understood. A study of several families found the mode of inheritance to be autosomal recessive in some cases and autosomal dominant in others.52,83 In some families, the gingival enlargement may be linked to the impairment of physical development.56 The enlargement usually begins with the eruption of the primary or secondary dentition, and it may regress after extraction, which suggests that the teeth (or the plaque attached to them) may be initiating factors. The presence of bacterial plaque is a complicating factor.
Gingival enlargement has been described in tuberous sclerosis, which is an inherited condition characterized by a triad of epilepsy, mental deficiency, and cutaneous angiofibromas.106,110
/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses