Fractures of the Zygomatic Complex and Arch
Terminology and Fracture Patterns
Classification of Zygomaticomaxillary Complex Fractures
Diagnosis of Zygomaticomaxillary Complex Fractures
Treatment of Zygomaticomaxillary Complex Fractures
Determining Whether the Zygoma Has Been Properly Reduced
Need for Internal Orbital Reconstruction
Principles in the Treatment of Zygomaticomaxillary Complex Fractures
Surgical Approaches to Zygomaticomaxillary Complex Fractures
Internal Orbital Reconstruction
Zygomatic fractures are common facial injuries, representing the most common facial fracture2–14 or the second in frequency after nasal fractures.3,15–17 The high incidence of these fractures probably relates to the zygoma’s prominent position within the facial skeleton, which frequently exposes it to traumatic forces. The incidence, cause, age, and gender predilection of zygomatic injuries vary, depending largely on the social, economic, political, and educational status of the population studied. Most studies indicate a male predilection, with a ratio of approximately 4 : 1 over females.18–27 Most authors also agree that the peak incidence of such injuries occurs around the second and third decades of life.28,29 The causes of zygomatic injury in some studies are mostly altercations, whereas in others, motor vehicle accidents (MVAs) account for a more substantial number.30,30a The cause of the injuries sustained is greatly affected by the nature of the population in these studies; in the former studies, the populations were from industrialized areas with high rates of unemployment, in which interpersonal violence is very high.
In zygomatic fractures caused by altercations, the left zygoma is most commonly affected,* presumably because of the greater incidence of right-handed individuals. This predilection disappears in unilateral fractures caused by MVAs. Bilateral fractures of the zygoma are uncommon and account for approximately 4% of 2067 cases of zygomatic fracture in a 10-year review by Ellis et al.26 Bilateral fractures in that study were more commonly the result of MVAs than altercations, indicating that the trauma inflicted in MVAs is more severe than that inflicted in altercations.
Anatomy
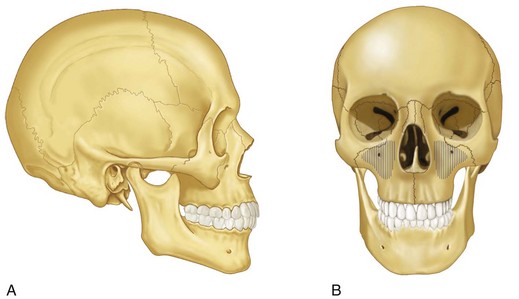
The zygoma is roughly the equivalent of a four-sided pyramid (Fig. 16-1). It has temporal, orbital, maxillary, and frontal processes, and articulates with four bones—the frontal, sphenoid, maxillary, and temporal (Fig. 16-2). The body of the zygoma extensively articulates with the maxilla along the anterior maxilla and along the orbital floor (see Fig. 16-2B). The suture between these two bones lies just lateral to the infraorbital foramen and runs laterally from the infraorbital rim to the undersurface of the zygomaticomaxillary buttress. It forms the superolateral aspect and part of the superoanterior aspect of the maxillary sinus. The zygoma also has a narrow weak articulation with the zygomatic crest of the greater wing of the sphenoid bone at the lateral aspect of the inferior orbital fissure (Fig. 16-3A). It forms a major portion of the lateral aspect and floor of the orbit. The frontal process is thick and triangular in cross section, with facial, orbital, and temporal surfaces. Because of its thickness, it is a frequent site for wire or bone-plate fixation following fracture. The temporal process is flat and projects posteriorly to articulate with the zygomatic process of the temporal bone; the combination of the two makes up the zygomatic arch. The zygomaticotemporal articulation is a thin delicate connection, which fractures frequently and with minimal force.
Terminology and Fracture Patterns
Zygomatic or malar fractures are the terms commonly used to describe fractures that involve the lateral third of the middle face. Because of the impure nature of zygomatic fractures, other terms have been adopted in describing such fractures. Zygomaticomaxillary complex, zygomaticomaxillary compound,31 zygomatico-orbital,26 zygomatic complex,32,33 malar, trimalar, and tripod fractures are terms that have been used to describe the clinical entity of fractures involving the zygoma and adjacent bones. The latter two terms are misnomers because the zygoma has not three but four processes, and their use should be condemned. Zygomatic, zygomatic complex, or zygomaticomaxillary complex (ZMC) are perhaps the most commonly used. They are used throughout this chapter because the zygoma is the major bone involved in such fractures and for the sake of simplicity. The term zygomatic or ZMC helps distinguish fractures that involve the zygoma and adjacent bones from isolated zygomatic arch fractures, and they are used when this distinction is necessary.
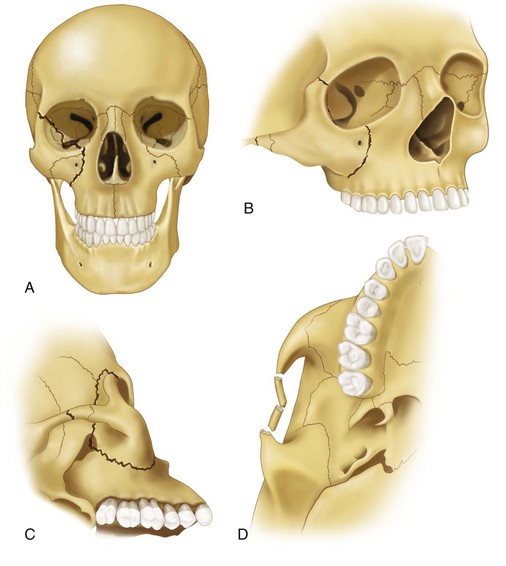
The inferior orbital fissure is the key to remembering the usual lines of ZMC fractures. Three lines of fracture extend from the inferior orbital fissure in an anteromedial, superolateral, and inferior direction (see Fig. 16-3). One fracture extends from the inferior orbital fissure anteromedially along the orbital floor, mostly through the orbital process of the maxilla toward the infraorbital rim. The orbital floor and medial wall are often comminuted, creating multiple lines of fracture within the internal orbit. The infraorbital canal is usually crossed by the fracture line(s) because the fracture frequently extends through the infraorbital rim to the facial surface of the maxilla, above or even slightly medial to the infraorbital foramen. The fracture extends from the infraorbital rim in the maxilla laterally and inferiorly under the zygomatic buttress of the maxilla. Comminution of the infraorbital rim and bone along the anterior and lateral maxilla is common, with frequent involvement of the infraorbital foramen. Therefore, the fracture rarely involves the zygomatic bone along the orbital floor and the anterior and lateral aspects of the face. The fracture lines are mostly within the maxilla.
A second line of fracture from the inferior orbital fissure runs inferiorly through the posterior (infratemporal) aspect of the maxilla and joins the fracture from the anterior aspect of the maxilla, under the zygomaticomaxillary buttress (see Fig. 16-3C).
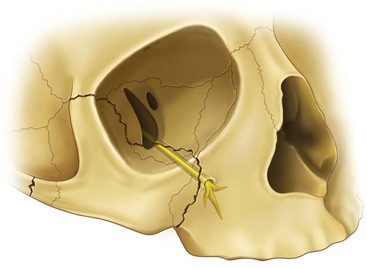
The third line of fracture extends superiorly from the inferior orbital fissure along the lateral orbital wall posterior to the rim, usually separating the zygomaticosphenoid suture (see Fig. 16-3A and C). Extending superiorly, laterally, and anteriorly toward the lateral orbital rim, the fracture frequently separates the frontozygomatic suture at the lateral orbital rim. However, the fracture through the lateral orbital rim is occasionally superior or inferior to the frontozygomatic suture.
A ZMC fracture that follows this pattern usually has one additional fracture line through the zygomatic arch. Because the point of least resistance to fracture is not at the zygomaticotemporal suture, but approximately 1.5 cm more posteriorly, the point of fracture when a single fracture exists is usually in the approximate middle of the zygomatic arch, in the zygomatic process of the temporal bone. Frequently, however, three fracture lines exist through the arch, producing two free segments when the fractures are complete (see Fig. 16-3D). These segments can be displaced by associated muscle pull or may be pushed medially into the infratemporal fossa. Often, the fractures are incomplete, or greenstick, fractures, producing a medial or lateral warping of the zygomatic arch without notable upward or downward displacement.
This description is for the common or usual ZMC fracture. However, the variability of these fractures is great because of the differences in magnitude and direction of force, amount of soft tissue covering the zygoma, and density of the adjacent bones. Frequently, the lines of fracture are in locations different from those described earlier. Using radiographs to summarize the course of fracture lines in 100 isolated zygomatic injuries, Meyer et al11 have found fractures in the body of the zygoma in almost 40% of cases, compared with the more common medial location along the anterior maxillary surface. Single or multiple lines of fracture (i.e., comminution) may exist. Gross displacement may occur, or no displacement at all. Because of the infinite number of possible variations, one must assess each zygomatic fracture independently and determine the extent and location of the fractures present.
Classification of Zygomaticomaxillary Complex Fractures
It is probably fair to say that classification of zygomatic fractures according to the individual who tries to describe them. The result has been a confusing array of classification systems that try to describe the anatomic position of the displaced bone or to classify fractures using position and criteria for postreduction stability.6,22,33–39 Whether a patient receives better treatment from being classified into one system or another is doubtful, and one should not dwell on the many classification systems available. As is true for many other aspects of surgery, it is extremely rare to find two patients who have exactly the same condition.
In 1990, Manson et al40 published a classification of midfacial fractures that was based on the amount of energy dissipated by the facial bones secondary to the traumatic force. Their classification of high-, moderate-, or low-energy fractures was based on findings on computed tomography (CT) scans. High-energy fractures had extreme displacement, comminution of the articulations, and segmentation of the bones. They noted that these required extensive exposure and fixation for a satisfactory outcome. On the other hand, lower energy fractures were characterized by displacement but without comminution of bony articulations. They noted that these could be treated by less aggressive means. Using preoperative CT findings may be the most useful way to decide how much intervention may be required before surgery.
Diagnosis of Zygomaticomaxillary Complex Fractures
Clinical Examination
After the clinician has ascertained the neurologic status of a patient with suspected ZMC fracture, the first priority is determination of the visual status of the involved eye. A thorough ocular and funduscopic examination should be performed, with complete documentation of the findings. Ocular injuries, such as vitreous hemorrhage, hyphema, globe laceration, severance of the optic nerve, and corneal abrasions, were found in 4% of patients with midfacial trauma by Turvey12 and in 5% of zygomaticoorbital fractures by Livingston et al.41 Ophthalmologic consultation was deemed necessary in approximately 5% of 2067 cases of zygomaticoorbital injuries reported by Ellis et al.26 Ioannides et al42 found significant ocular and adnexal injuries in 26% of orbital fractures. Al-Qurainy et al43 prospectively performed ophthalmologic examinations in 363 patients who had sustained midfacial fractures. Minor or transient eye injuries, such as corneal abrasion, chemosis, mild impairment of accommodation and visual acuity, and orbital emphysema, were found in 63% of patients. Moderate injuries, such as enophthalmos, conjunctival abrasion, traumatic pupillary changes, iridodialysis, lens damage, macular edema, and moderate to severe impairment of accommodation and visual acuity, were noted in 16% of patients. Severe ophthalmic disorders, such as gross proptosis, retrobulbar hemorrhage, corneal laceration, hyphema, angle recession, severe reduction or loss of vision, visual field loss, choroidal tear involving the macula, and optic nerve injuries, were found in 12% of patients. One third of all patients with comminuted ZMC fractures suffered a severe ocular disorder. Therefore, if the clinician discovers any significant or questionable findings in patients with midfacial fractures, ophthalmologic consultation should be obtained.
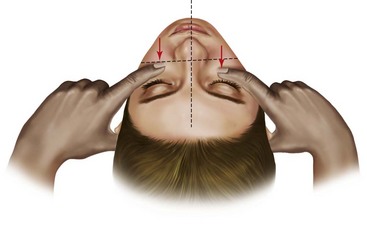
Examination of the zygoma involves inspection and palpation. Inspection is performed from the frontal, lateral, superior, and inferior views. One should note symmetry, pupillary levels, presence of orbital edema and subconjunctival ecchymosis, and anterior and lateral projection of the zygomatic bodies. The most useful method for evaluating the position of the body of the zygoma is from the superior view. The patient can be placed in a recumbent position or recline in a chair. The surgeon inspects from a superior position, evaluating how the zygomatic bodies project anteriorly and laterally to the supraorbital rims, comparing one side with the other. The surgeon should lay his or her index finger below the infraorbital margins, along the zygomatic bodies, pressing into the edematous tissue to palpate and reduce the visual effect of edema simultaneously when performing this examination (Fig. 16-4).44 The superior view is also helpful for evaluating possible depression of the zygomatic arches. One should not forget to perform an intraoral examination, because zygomatic fractures are often accompanied by ecchymosis in the superior buccal sulcus and maxillary dentoalveolar fractures.
Signs and Symptoms
Periorbital Ecchymosis and Edema.
Edema and bleeding into the loose connective tissue of the eyelids and periorbital areas is the most common sign following fracture of the orbital rim.45,46 Swelling, often massive, may be present and is most dramatic in the periorbital tissue, where the eyelids may be swollen closed. The ecchymosis may be in the inferior lid and infraorbital area only or around the entire orbital rim.
Flattening of the Malar Prominence.
A characteristic sign and striking feature of zygomatic injury is a flattening of the normal prominence in the malar area. An especially common finding in ZMC injuries, this flattening is reported in 70% to 86% of cases,22,26,29 especially those in which distraction of the frontozygomatic suture and medial rotation and/or comminution have occurred. If edema is present, flattening may be difficult to discern soon after injury; however, one can usually gain an appreciation of this sign by depressing the index fingers into the soft tissue of the zygomatic areas and comparing one side with the other from above the patient (see Fig. 16-4).
Deformity of the Orbital Margin.
Fractures running through the orbital rim often result in a gap, or step deformity, if displacement has occurred. This finding is frequently noted at the infraorbital and lateral orbital rims when zygomatic fractures are present.45,46 These areas may also be tender to touch.
Trismus.
Limitation of mouth opening frequently accompanies zygomatic injuries and is present in approximately one third of cases.26,46,47 This condition occurs with an even higher incidence in isolated fractures of the zygomatic arch (45%). The reason often cited for postfracture trismus is impingement of the translating coronoid process of the mandible on the displaced zygomatic fragments. Whether this contact actually occurs in most cases is doubtful, because the amount of displacement necessary for producing actual mechanical interference is great. A more likely explanation is muscle spasm secondary to impingement by the displaced fragments, especially on the temporal muscle (Fig. 16-5). An associated finding is deviation of the mandible toward the fractured side when the mouth is opened.
Abnormal Nerve Sensibility.
An important symptom, present in approximately 50% to 90% of ZMC injuries, is impaired sensation of the infraorbital nerve.22,26,45–52 Infraorbital nerve paresthesia is more common in fractures that are displaced than those that are not. It is difficult to differentiate true anesthesia from the altered sensation of swollen edematous tissue but, as the swelling decreases, infraorbital nerve anesthesia becomes apparent. Infraorbital anesthesia occurs when the fracture through the orbital floor and/or the anterior maxilla causes tearing, shearing, or compression of the infraorbital nerve along its canal or foramen (Fig. 16-6). Frequently, the entire orbital floor is comminuted, which results in multiple fragments of bone strung together by the infraorbital neurovascular bundle. When the line of fracture is lateral to the infraorbital groove and foramen (less common), the infraorbital nerve is spared. Disruption of the infraorbital nerve causes anesthesia of the lower eyelid, upper lip, and lateral aspect of the nose.
A related symptom may be altered sensitivity of the maxillary teeth and gingiva.53 When this altered sensitivity is present, the clinician should suspect a disruption of the infraorbital nerve within its canal, where the middle and anterior superior alveolar nerves take origin.
Epistaxis.
Whenever the sinus mucosa is disrupted, hemorrhage into the sinus is possible. Most fractures through the sinus wall that have had even a minor amount of displacement tear the lining mucosa, producing internal bleeding. Because the maxillary sinus drains into the nose via the middle meatus, unilateral hemorrhage from the nose is possible and occurs in approximately 30% to 50% of ZMC injuries.26,46
Subconjunctival Ecchymoses.
Subconjunctival hemorrhage, a frequent finding in zygomatic fractures, is present in 50% to 70% of cases.26,46 It may accompany even a hairline crack through the orbital rim if the periosteum has been torn. Its absence does not exclude an orbital rim fracture because if no disruption of the periosteum has occurred, bleeding can accumulate in a subperiosteal location and may not be visible under the conjunctiva. When present, subconjunctival ecchymoses usually have no posterior limit and will be bright red because of the ability of oxygen to diffuse through the conjunctiva to the collection of blood.
Displacement of the Palpebral Fissure.
The lateral palpebral ligament is attached to the zygomatic portion of the orbital rim. Displacement of the zygoma carries the palpebral attachment with it and thus produces a dramatic visual deformity. When the zygoma is displaced in an inferior direction, the lateral palpebral ligament is also depressed, causing a downward slope to the fissure (antimongoloid slant) (Fig. 16-7). Because the orbital septum is attached to the infraorbital rim, inferior or posterior displacement of the inferior orbital rim causes depression of the lower eyelid, giving it a shortened appearance.54 This depression may cause more sclera to be exposed below the iris and an apparent ectropion.
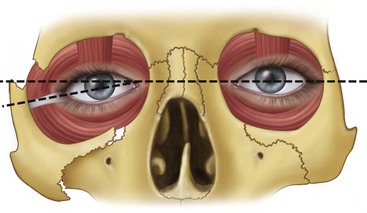
Unequal Pupillary Levels.
With the disruption of the orbital floor and lateral aspect of the orbit that frequently accompanies zygomatic fractures, loss of osseous support for the orbital contents and displacement of Tenon’s capsule and the suspensory ligaments of the globe permit depression of the globe.55 This displacement is manifested clinically as unequal pupillary levels, with the involved pupil at a level lower than that of the normal side (see Fig. 16-7).
Diplopia.
Diplopia is the name given to the symptom of blurred vision. Two varieties of diplopia exist; it is important to distinguish between them. Monocular diplopia, or blurring of vision through one eye with the other closed, requires the immediate attention of an ophthalmologist, because it usually indicates a detached lens, hyphema, or other traumatic injury to the globe. Binocular diplopia, in which the blurring of vision occurs only when the patient looks through both eyes simultaneously, is common and occurs in approximately 10% to 40% of zygomatic injuries.* Al-Qurainy et al65 have found that the severity of diplopia is associated with the severity of midfacial injuries. Almost 30% of patients with comminuted fractures of the ZMC experienced diplopia, 22% of patients with noncomminuted displaced ZMC fractures had diplopia, and only 8% of patients with minimally displaced or nondisplaced ZMC fractures had diplopia. Binocular diplopia that develops following trauma can be the result of soft tissue (muscle or periorbital) entrapment, neuromuscular injury, intraorbital or intramuscular hematoma or edema, or a change in orbital shape, with displacement of the globe causing a muscle imbalance. Enophthalmos and globe ptosis associated with marked displacement of the globe can also cause diplopia.
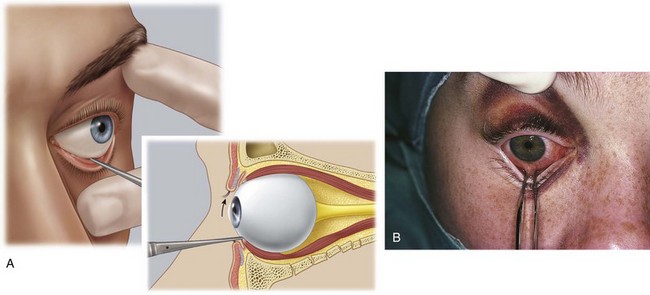
One can determine the presence of entrapment of orbital contents by the fracture through the orbital floor with a forced duction test. Small forceps are used to grasp the tendon of the inferior rectus through the conjunctiva of the inferior fornix and the globe is manipulated through its entire range of motion (Fig. 16-8). Inability to rotate the globe superiorly signifies entrapment of the muscles in the orbital floor. This test should differentiate between entrapment of orbital contents and paralysis as a result of neuromuscular injury or edema. The test should be performed routinely in those who cannot rotate the globe into an upward gaze.
Enophthalmos.
If the zygomatic injury has produced an increase in orbital volume, usually by lateral and inferior displacement of the zygoma and/or disruption of the inferior, medial, and/or lateral orbital walls, or has resulted in a decrease in orbital soft tissue volume by herniation of orbital soft tissue, enophthalmos can result. This diagnosis is difficult to make acutely unless the enophthalmos is severe because adjacent soft tissue edema always produces a relative enophthalmos. After the swelling has dissipated, enophthalmos becomes more obvious and is frequently associated with ptosis of the globe. The clinical manifestations of enophthalmos are accentuation of the sulcus of the upper lid and narrowing of the palpebral fissure, causing pseudoptosis of the upper lid. The anterior projection of the globe as viewed from above is reduced on the side of injury. Zygomatic fractures are associated with enophthalmos in approximately 5% of cases before treatment.22,26,46 If enophthalmos is present during the initial examination, it is likely that a great increase in bony orbital volume has occurred.66,67
Radiologic Evaluation
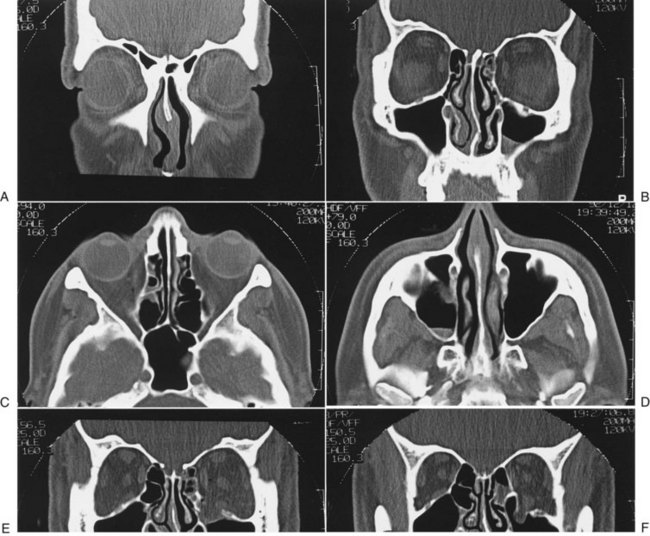
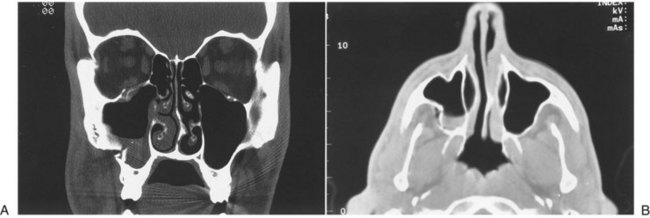
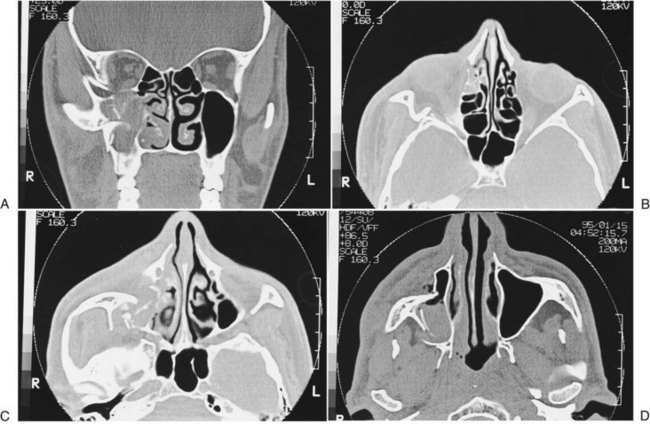
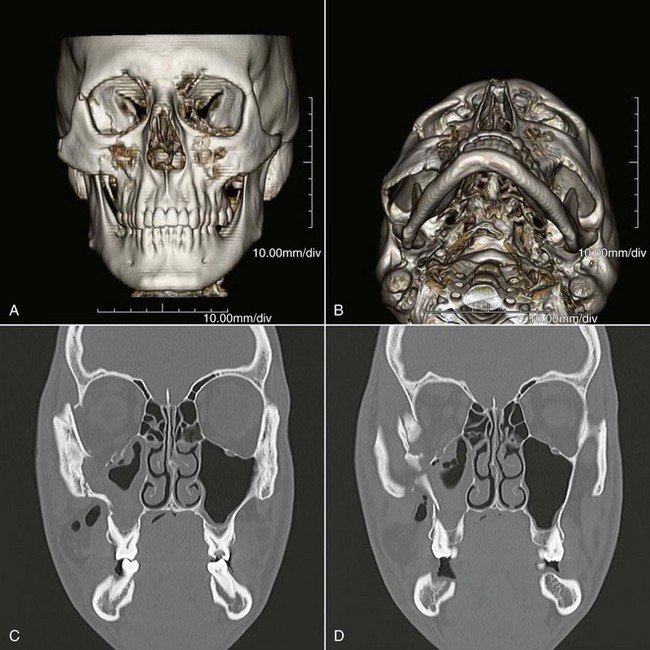
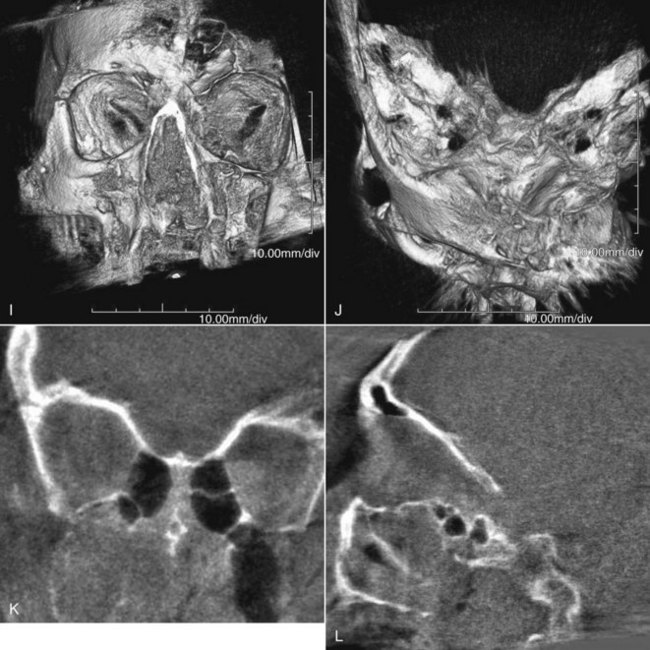
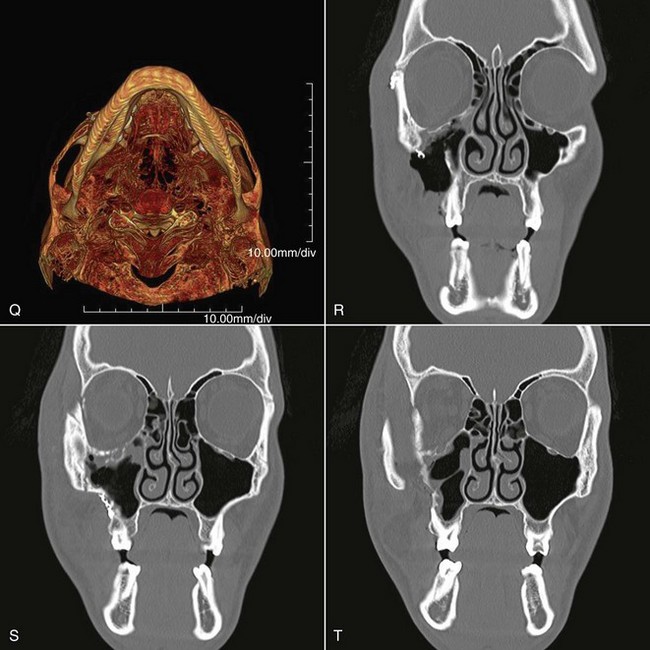
By 1992, CT essentially supplanted other radiologic methods in the assessment of patients with midfacial injuries.68 Two-dimensional CT is now considered the best and most useful means of radiologic assessment of the injured facial skeleton.69 The amount of information that can be obtained with CT is much greater than that which can be obtained from a series of plain films. CT accurately identifies lines of fracture, position and displacement of the ZMC, and status of the zygomatic arch (Fig. 16-9). CT scans are especially helpful in that they allow a complete assessment of the status of the orbital floor and walls and the depth to which one must dissect to reach stable bone. CT has eliminated the question about whether the orbit should be explored. With the accurate image of the internal orbit provided by CT, one can make a decision regarding the necessity for internal orbital reconstruction before surgery.
The status of the orbital soft tissue can also be assessed because of the great contrast provided by CT. Comparison of globe projection from one side with the other helps identify enophthalmos in unilateral injuries.66,67,70,71 Also, CT scans allow identification of associated craniofacial injuries.72 For ZMC injuries, it is optimal to obtain axial and coronal high-resolution scans. The axial scan is extremely helpful in evaluating the medial and lateral orbital walls, and the coronal scan defines the extent of injury to the orbital floor (see Fig. 16-9). Reformatted coronal views (from axial scans) are not as helpful but may be necessary if the patient cannot be properly positioned because of injury. Three-dimensional CT scans offer no additional information beyond what is already present in two-dimensional scans but are useful to understand the displacement and fracture patterns.73,74
Treatment of Zygomaticomaxillary Complex Fractures
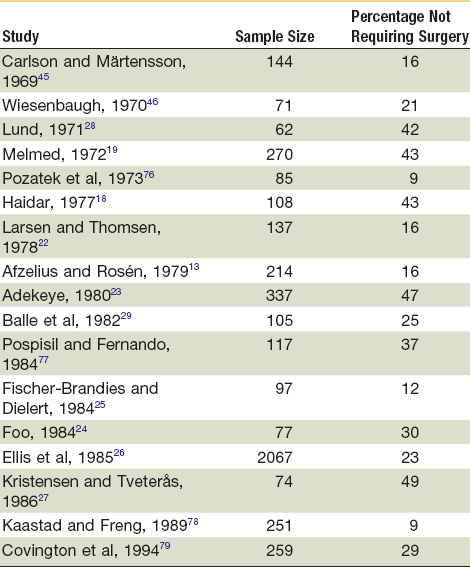
Since Duverney75 first described the fractured zygoma, numerous methods have been suggested for treating it. These range from nonintervention and observation to open reduction and internal fixation (ORIF). Because many fractures are nondisplaced or minimally displaced, intervention is not always necessary. Studies have shown that between 9% and 50% of ZMC fractures do not require operative treatment (Table 16-1).
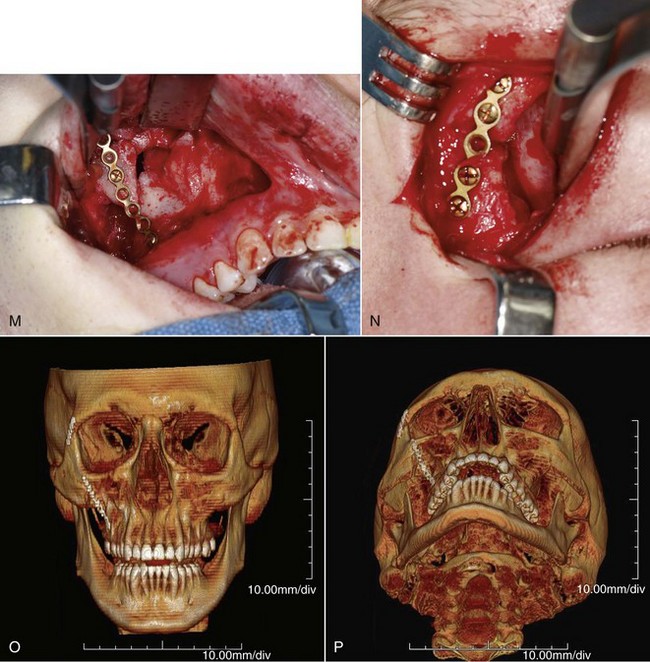
One must be aware that ZMC fractures can result from high- and low-energy injuries.40 Those resulting from altercations seem to be more linear in character and displaced en bloc (Fig. 16-10). These fractures can frequently be treated with limited exposure, simple reduction, and simple methods of fixation, if necessary. Conversely, high-energy injuries, such as those sustained in MVAs, produce more comminution, especially of the adjacent bones, where the ZMC abuts, and are much less amenable to simple methods of treatment (Fig. 16-11). These fractures usually require extended open reduction and rigid fixation techniques. The surgeon must therefore be aware of the nature and extent of the injury as treatment is planned.
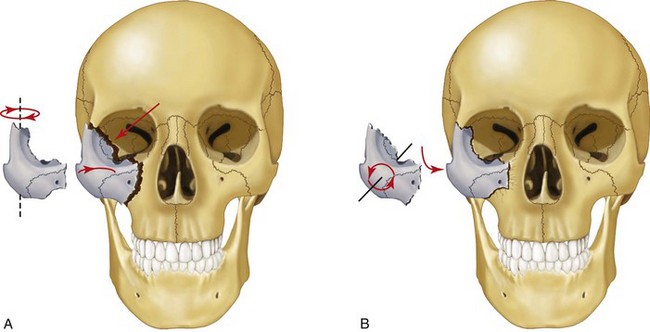
The fractured zygoma is perhaps the least understood and most frequently mistreated facial fracture. Much of the difficulty in treating these fractures stems from the complex and multiple anatomic relationships that the zygoma maintains within the facial skeleton. The most common mistake made in clinical practice is to assume that the ZMC will be in its proper position if the infraorbital and lateral orbital rims have been reduced. One must remember that the fractured ZMC has four major processes that articulate with adjacent bones. Only when three are properly positioned can one be sure of an accurate reduction. It may be more helpful to think of the zygoma as a four-legged chair. If three of the four legs are on the floor, the other must also be on the floor. On the other hand, if two legs are on the floor, two may also be off the floor. Therefore, reducing orbital rim fractures (two legs of the chair) does not guarantee that the entire complex has been properly reduced, because the zygoma can rotate inferiorly and medially (Fig. 16-12). In this case, fractures through the zygomatic buttress of the maxilla and zygomatic arch are left improperly aligned,80 producing a flattened appearance to the face in the area in which the body of the zygoma normally gives soft tissue support.
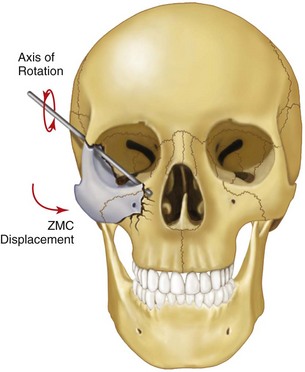
FIGURE 16-12 The ZMC can rotate inferiorly and medially, even when reduced at the frontozygomatic and infraorbital areas.
Because of the ZMC’s difficult anatomic details, and because there are no sensitive clues to accurate and stable reduction, some surgeons have suggested that each ZMC fracture be treated aggressively, with ORIF of at least two of its four major processes.17,81–85 Dingman and Natvig,81 for example, have stated that “While closed reduction techniques are popular and attractive in the management of fractures in this region, the experienced surgeon will be quick to see, in many cases, the limitations that closed methods impose.” The main controversies in the treatment of ZMC fractures are the following:
1. Should surgical exposure of the zygoma in two or three locations routinely be performed to determine whether the reduction has been adequate?
Determining Whether the Zygoma Has Been Properly Reduced
There should be no doubt that observation of the fracture in three of its four processes will allow the surgeon to determine the postreduction position accurately. Karlan and Cassisi80 have shown this to be true in a clinical review of their patients. The question therefore becomes whether this is always necessary. Recommendations in the literature for reduction of ZMC fractures range from closed reduction techniques78–79 to three- or four-point surgical exposure.89–92 Incisions used to expose the lateral orbital, infraorbital, and zygomaticomaxillary buttress (intraorally) areas not only take time but also have the potential to produce complications of their own, regardless of the zygomatic fracture for which they are being used (see later, “Complications”).
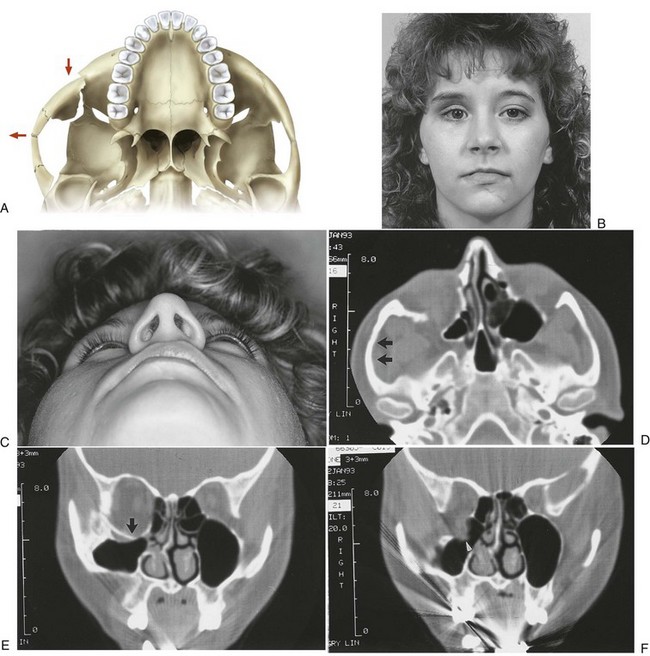
In several cases, however, surgical exposure becomes helpful. First, when preoperative signs and symptoms and/or radiographs indicate the need for internal orbital reconstruction, it is prudent to gain access to the infraorbital rim and orbital floor before elevation of the zygoma. Second, if surgery must be performed while excessive facial edema is present, surgical exposure to determine the position of the ZMC is helpful. Third, if one cannot determine whether the reduction has been adequate during the surgery, exposure will provide the necessary verification. Fourth, surgical exposure is helpful if fixation devices are deemed necessary from the preoperative assessment of the fracture. Thus, the use of surgical exposure depends on the circumstances and experience of the surgeon; however, given these examples, it will be frequently performed. If there is any doubt about the postreduction ZMC position, one should verify it with exposure, remembering that even though the orbital rims are reduced, the body of the zygoma can be rotated medially. Exposure and exploration of other areas help determine when the zygoma has been properly reduced. Fractures at the zygomatic arch and internal orbit along the greater wing of the sphenoid (Fig. 16-13A) are sensitive indicators of ZMC position. However, exposure of the zygomaticomaxillary buttress (intraorally; see Fig. 16-13B) provides one of the most valuable clues about the adequacy of ZMC position, if it is not severely comminuted. With this exposure, one will also have excellent exposure of the infraorbital rim. It should be realized that a reciprocal relationship exists between malar projection and facial width. If the zygomatic arch is bowed laterally, the malar eminence is posteriorly displaced (Fig. 16-14). Reduction of ZMC fractures should ensure that the malar eminence is properly projected anteriorly and, if the zygomatic arch is reconstructed, the procedure is done by keeping it flat.
Another important point that should be stressed in the treatment of ZMC fractures is the status of the medial orbital rim. Occasionally, a unilateral nasal-orbital-ethmoid fracture occurs on the side of the ZMC fracture, displacing the medial portion of the infraorbital rim laterally. This portion of bone may seem to be very stable and the fact that it is malpositioned may go unnoticed. If the ZMC is reduced into apposition with this laterally displaced fragment of infraorbital rim, the ZMC will be laterally positioned, increasing orbital volume and widening the face (Fig. 16-15). Because a unilateral nasal-orbital-ethmoid fracture may be difficult to diagnose clinically, preoperative CT scans are the best diagnostic tool (see Fig. 16-9A). Therefore, one should always search for fractures of the medial orbital rims when assessing preoperative scans.
Need for Fixation
One of the most controversial topics in maxillofacial surgery is the amount of fixation necessary to prevent postreduction displacement of the fractured ZMC.93–95 Some have noted that reduction, by itself, does not produce adequate stability of the fractured zygoma, claiming that the downward pull of the masseter muscle will cause a medial rotation of the zygomatic body before healing.* Albright and McFarland96 went so far as to recommend intermaxillary immobilization following fracture reduction to help reduce the pull of the masseter muscle on the repositioned ZMC. The masseter muscle has often been implicated as a primary cause of postreduction displacement of the fractured ZMC. It was assumed to be capable of exerting sufficient inferiorly directed force on the fractured ZMC to cause movement, even after surgical insertion of fixation devices. However, this contention has never been proven. There is no evidence in the literature that postreduction displacement of a ZMC fracture has occurred in patients. Previous clinical studies simply evaluated patients clinically and radiographically months after surgery and noted an occasional patient with poor ZMC position. It was assumed that because the fractures were simply elevated, or perhaps stabilized with wire fixation, postsurgical displacement had occurred. Therefore, recommendations for fixation have varied from none to the placement of three or four bone plates at different locations around the fractured ZMC.
Ellis and Kittidumkerng99 have reviewed a series of isolated ZMC fractures treated by different approaches and fixation schemes, both immediately and several weeks after repair, and found no evidence of postreduction instability in any patient. Based on their experience and the data generated from their study, various methods can be used successfully to stabilize ZMC fractures. These range from reduction without fixation to reduction with three- or four-point fixation using bone plates.
Such a diversity of treatment options should not be surprising, given the results of a study by Dal Santo et al.95 Thier study compared masseter muscle force in 10 male control subjects with that in 10 male patients who had sustained unilateral ZMC fractures. The calculation of muscle force was based on measured bite force, electromyograms, and radiographic determination of muscle vectors. It was found that the masseter muscle developed notably less force in patients with ZMC fractures than in control subjects. Following fracture, masseter muscle force slowly increased, but at 4 weeks after surgery, most patients were still well below control levels. The results of that study cast doubt on the role of the masseter muscle in postreduction displacement of the fractured ZMC and indicate that potentially minimum amounts of fixation are required for such injuries.
Most have disagreed with the concept that fixation should be routinely applied following reduction of zygomatic fractures.* These surgeons applied fixation to zygomatic fractures only where indicated. The indications for the application of fixation seem to vary with the surgeon and type of fracture, so the incidence of fixation application varies widely in the literature (8% to 100%) (Table 16-2).
TABLE 16-2
Reported Incidence of the Need for Fixation in Addition to Reduction
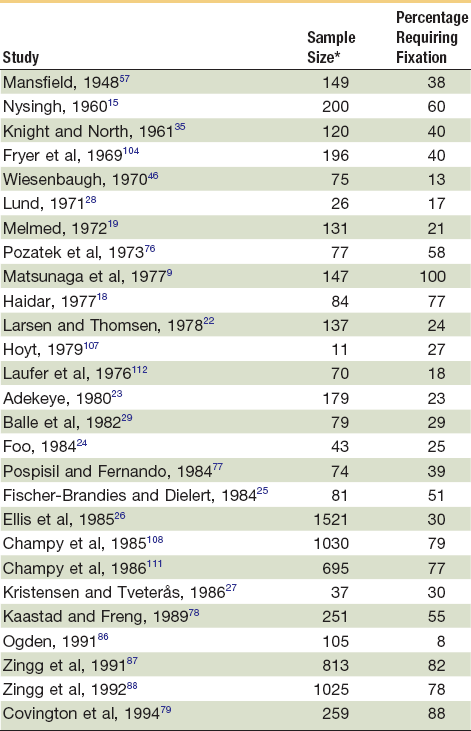
*Only those cases that were surgically treated in these studies are included in this table.
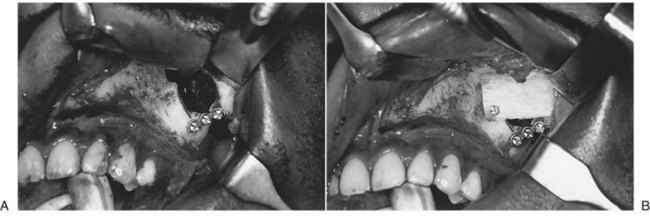
The efficacy of using simple elevation (without fixation) when indicated has been demonstrated by Larsen and Thomsen.22 They reexamined 87 patients several months to years after elevation of their fractures by the Gillies temporal approach and found only 2 patients with residual deformity. Similarly, Fischer-Brandies and Dielert25 reexamined 41 cases of zygomatic fracture treated with elevation using a hook and found no postsurgical displacement. Several other studies in the literature have used ZMC repositioning without fixation, with good results,29,78–79 verifying that fixation requirements are less than advocated by some. Fixation with one bone plate has been advocated by several surgeons in a certain percentage of ZMC fractures, either at the zygomaticomaxillary buttress* or, more commonly, at the frontozygomatic area.† Champy et al111 used a single bone plate at the frontozygomatic area in 342 isolated ZMC fractures and found that only 6 (1.8%) had an unsatisfactory result. Tarabichi100 treated 17 consecutive low-velocity ZMC fractures by a transoral open reduction and internal bone-plate fixation of the zygomaticomaxillary buttress, with excellent results in all but 2 patients, who had comminution of the orbital rim. Covington et al79 were able to stabilize 30% to 40% of ZMC fractures by one-point fixation. Ellis and Kittidumkerng99 were able to use one-point fixation in 31% of ZMC fractures reported in their study. Similar results were shown by Shumrick et al.114
Need for Internal Orbital Reconstruction
By definition, the orbital floor is fractured in ZMC fractures. However, the magnitude and extent of orbital floor disruption vary from a linear crack to fragmentation of the entire floor and medial and lateral walls. Many, perhaps most, low-energy ZMC fractures do not have herniation of periorbital contents into the sinus with entrapment of ocular muscles or enophthalmos. However, these problems do occur in a certain percentage of cases. Davies115 noted significant orbital floor disruption in 47% of patients with zygomatic fractures. Sacks and Friedland116 noted this complication in two thirds of ZMC fractures. Crewe117 noted notable disruption in most zygomatic fractures. Crumley and Leibsohn64 noted that 39% of zygomatic fractures had comminuted fractures of the orbital floor. The need for orbital floor reconstruction to support the periorbital tissue was necessary in two of three cases of orbital floor exploration performed by Pozatek et al76 and Wiesenbaugh.46 Ellis et al26 found it necessary to place implants in one of three cases on exploration of the orbital floor. The orbital floor and walls were reconstructed in 44% of isolated ZMC fractures in a study by Ellis and Kittidumkerng.99 A similar study by Shumrick et al found the necessity to reconstruct the internal orbit in only 30% of ZMC fractures.114
Although some surgeons believe that so-called exploration of the internal orbit should be performed routinely when operating on ZMC fractures,* most do not. These surgeons would argue that exploration of the orbit should depend on preoperative and intraoperative findings. Fortunately, CT scans have eliminated the debate about when an orbit should be explored. It is now possible to obtain an accurate assessment of the status of the internal orbit before surgery so that adequate treatment can be proscribed and planned.114,118 If comminution of the orbital floor and walls and/or prolapse of orbital soft tissue into the maxillary and ethmoid sinuses is noted, or if orbital volume has increased from blowout of the floor and walls, reconstruction should be performed.119,120 Using similar criteria in the preoperative CT scans, Reddy and Ellis were able to classify patients successfully into those who required and those who did not require internal orbital reconstruction.118 They showed that in those who were determined not to need internal orbital reconstruction, good radiographic and clinical results were obtained.
With the availability of intraoperative CT scanning in some operating rooms, the question about whether to reconstruct the internal orbit in those patients in whom the preoperative CT scan does not show gross disruption can be answered in the operating room. After the ZMC has been reduced, a scan is taken and an assessment of the internal orbit is made. The surgeon can then decide whether it is necessary to reconstruct the orbital walls (Fig. 16-16).
Principles in the Treatment of Zygomaticomaxillary Complex Fractures
In the treatment of any ZMC fracture that requires surgical intervention, consideration should be given to each of several steps in a sequential and orderly manner (Box 16-1).
Clinical Examination and Forced Duction Test.
Following induction of general anesthesia, the surgeon should take the opportunity to examine the patient more carefully. With the patient under anesthesia, the surgeon has more freedom in the examination and can use more digital force than is possible with the patient awake. This examination can help confirm previous diagnoses and may reveal new information. It is very important to look at the patient from the superior view and to visualize both zygomas simultaneously. Unless the swelling is marked, one should be able to determine an asymmetry. Laying the index finger across the infraorbital area or on the malar prominence should help discern the asymmetry (see Fig. 16-4). A forced duction test should also be performed at this time (see Fig. 16-8).
Protection of the Globe.
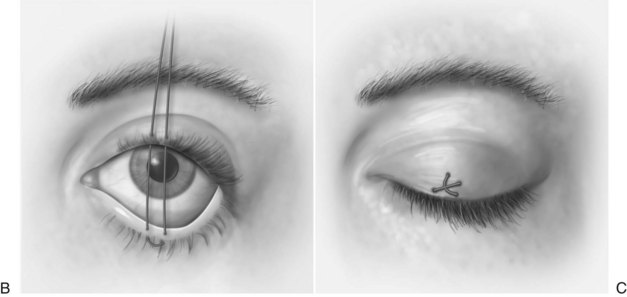
The cornea must be protected from inadvertent trauma. Of the several ways of providing this protection, perhaps the simplest is placement of a scleral shell (corneal shield) after application of an ophthalmic ointment (Fig. 16-17A). Temporary tarsorrhaphy can also be used by suturing the dermal surfaces of the upper and lower eyelids together with 5-0 nylon sutures (see Fig. 16-17B and C).
Internal Orbital Reconstruction.
In minimally displaced cases in which no ocular signs of entrapment or enophthalmos are noted preoperatively, and in which the fracture is treated by simple reduction, internal orbital exploration and/or reconstruction is unnecessary unless a postreduction forced duction test produces positive findings (rare). In most of these cases, reduction of the zygoma results in adequate alignment of the orbital floor.33,114,118 However, one should never avoid reconstructing the internal orbit for fear of causing harm to orbital tissue. This occurrence is extremely rare. For those surgeons who have intraoperative CT scanning capability, the status of the internal orbit after reduction of the ZMC is known and the decision about the need for internal orbital reconstruction can be made during the surgery.
Assessment of Ocular Motility.
Another forced duction test should be performed at the end of all active treatment, with the possible exception of suturing, to verify that the treatment did not create entrapment of orbital contents (see Fig. 16-8).
Bone Graft for Extraorbital Osseous Defects.
Consideration should be given to grafting areas of missing bone along the anterior maxilla and zygomaticomaxillary buttress. Even though bone plate fixation may provide stabilization of the ZMC by spanning such defects, it is unclear how long bone plates will provide such stability. Reconstruction of the skeleton with bone grafts prevents soft tissue prolapse from the cheek into the maxillary sinus and promotes osseous union across the defect, providing long-term stability (Fig. 16-18).
Soft Tissue Resuspension.
In 1991, Phillips et al121 described a method of soft tissue suspension of infraorbital and malar soft tissues before closing incisions after treating midfacial fractures. They hypothesized that these soft tissues droop if not resuspended; the drooping results in facial asymmetry and provides traction on the lower eyelid, causing ectropion. Yaremchuk and Kim122 have confirmed this hypothesis and found a 20% incidence of scleral show when the facial soft tissue was not resuspended but no scleral show when the tissue was resuspended. Thus, for fractures in which the soft tissue was completely stripped from the bone, sutures should be passed through the deep surface of the soft tissue of the cheek and secured to structures such as the orbital rim and temporal fascia to raise them into their proper location on the underlying bone (Fig. 16-19; see also Fig. 16-25F).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses