Chapter 15. Restoration of endodontically treated teeth
F. Mannocci and M. Giovarruscio
CHAPTER CONTENTS
Summary269
Introduction269
Effects of endodontic treatment on the tooth270
Survival of the endodontically treated tooth270
Timing the restorative procedure270
Learning outcomes285
References285
SUMMARY
There have been many recent advances in the methods available for restoring endodontically treated teeth. Most are related to adhesive techniques and as a result, composite resin/ceramic materials and non-metallic posts have become popular. These techniques, including the choice of restoration, are discussed in this chapter. However, regardless of the technique or the type of restoration, the survival of endodontically treated teeth may be improved by preserving as much useful tooth structure as possible and ensuring that the stress within the tooth and restoration is kept to a minimum.
INTRODUCTION
The completion of root canal treatment does not signal the end of patient management. The endodontically treated tooth has to be restored to both form and function. In addition, there is now a greater appreciation that coronal leakage may cause failure. Therefore, the quality of the coronal restoration has an influence on treatment outcome. The restoration of endodontically treated teeth has changed considerably in recent years. The availability of adhesive techniques has expanded treatment modalities. Amalgam cores and cast metal posts are being replaced by adhesive techniques and fibre posts; all-ceramic and composite resin crowns are chosen for better aesthetics. Non-adhesive techniques and restorations are still practised. However, in this chapter, the emphasis will be on adhesive restorations for endodontically treated teeth. Consequently, other restorative techniques have not been covered in any detail. The techniques suggested in this chapter are a matter of preference for the authors.
EFFECTS OF ENDODONTIC TREATMENT ON THE TOOTH
The fracture of endodontically treated teeth can have dire consequences1 and, in some cases, extraction is the only possible option. The loss of tooth substance as a result of endodontic and restorative procedures may be one of the reasons for the increased number of crown/root fractures that was observed in endodontically treated teeth compared to vital teeth with similar restorations. 2 The loss of the marginal ridge/s in particular, has been found to increase cuspal flexure in vitro. 3 The physical properties of the remaining dentine may also be altered by the effect of medicaments and irrigants. 4 In addition, there is loss of proprioception when the pulp tissue is removed; non-vital teeth have a higher load perception and can withstand up to twice the amount of loading compared with vital teeth before registering discomfort. 5 Other potential reasons for the increased susceptibility to fracture of endodontically treated teeth include changes in the chemical composition of coronal and root dentine as a result of moisture loss and alterations in collagen alignment. 2 However, apart from perhaps a very small increase in the modulus of elasticity, 6 which could be interpreted to be consistent with making the tooth more brittle, most other research has failed to show any change in the inherent physical properties of dentine. 7
In a recent study on the impact of endodontic treatment on tooth rigidity, 8 access cavity and post space preparations resulted in a significant reduction in root rigidity. In a micro-computed tomography study on extracted premolar teeth, the amount of hard tooth tissue structure lost due to caries removal, access cavity preparation, root canal preparation and post (fibre and cast) space preparation were investigated. 9 Access cavity and post space preparation caused the greatest loss of hard tooth tissue; the loss of coronal tooth structure caused by cast post space preparation was greater than that caused by fibre post preparation. 9 From the available evidence, mostly related to premolar teeth, the loss of tooth structure is the most significant factor in the weakening of endodontically treated teeth. Since adhesive restorative techniques do not require the creation of macromechanical retention, there is, consequently, a reduction in hard tooth structure loss.
SURVIVAL OF THE ENDODONTICALLY TREATED TOOTH
The failure rate of endodontically treated teeth restored with metal-ceramic crowns were reported to be significantly higher than that of vital teeth. 10 However, a recent systematic review11 showed that endodontically treated teeth restored with crowns have a higher long-term survival rate (81 ± 12% after 10 years) compared with teeth without crown coverage (63 ± 15% after 10 years). Interestingly, in the first 3 years, the survival rate of teeth without crown coverage was found to be satisfactory (84 ± 9%) but there was a significant decrease in survival rate after this period. 11 These results are in agreement with those of two randomized clinical trials on endodontically treated premolars restored without crown coverage. 12,13 Teeth restored with fibre posts and direct composite resin were found to be more effective than amalgam in preventing root fractures but less effective in preventing secondary caries. 13 Therefore, an adequate assessment of the tooth prognosis is essential14 (see Chapter 3). It was shown that endodontically treated teeth are more often extracted as a result of restorative rather than endodontic failures. It is generally acknowledged that such failures are the result of mistakes made in the treatment planning phase. 15
TIMING THE RESTORATIVE PROCEDURE
Some patients are willing to go to almost any length to try and hold on to a tooth, even if the prognosis is acknowledged to be guarded. Others may be unmotivated to embark on any complex treatment, or may wish only to invest in options they consider entirely predictable. Therefore, it is essential that endodontic treatment is part of an overall strategic patient management plan. It would be better to consider extraction and construction of a fixed prosthesis supported by a tooth or implant if the restorability is questionable (see Chapter 3). Although finance should never dictate treatment planning, in reality it remains a factor to consider when decision-making. In certain circumstances, after considering the costs of the endodontic treatment and restoration, and reviewed in the light of the prognosis for the tooth, extraction and replacement may be preferable to preservation. If tooth retention is desired, often a combination of endodontic, periodontal and restorative treatment may be necessary to rescue a tooth (Figs. 15.1& 15.2).
 |
 |
 |
 |
 |
 |
 |
| Figure 15.1
A badly broken down maxillary first molar (A) requiring crown lengthening (B) before being restored with a fibre post and composite core (C, D) followed by a metal-ceramic crown (E-G).
From Mannocci et al 200814 with permission of Quintessence Publishing Co. Ltd.
|
 |
 |
 |
| Figure 15.2
A broken down maxillary second premolar (A). Following root canal treatment and crown lengthening, the tooth was restored using a fibre post and composite core (B) followed by a metal-ceramic crown (C).
|
However, once the decision to root treat and restore has been taken, the next decision will be how long to wait after root canal treatment before placing the final restoration. There is no set answer but the following factors should be considered:
• pre-existing endodontic status
• quality of the root canal filling
• position of the tooth in the mouth
• type of restoration planned.
Following completion of root canal treatment, if the result is technically satisfactory and the tooth is symptom-free, it would be reasonable to proceed immediately to placement of the final restoration, especially when dealing with a previously vital, uninfected tooth. Although previously vital, if the tooth is tender to biting or lateral pressure after satisfactory completion of root canal treatment, it should be put on probation for 2 to 3 weeks. Hopefully, at the end of this period, the tooth is more comfortable and the final restoration can then proceed. If not, then an extended period of monitoring or a review of the possible causes for continuing symptoms including the need for retreatment should be considered.
If there was apical periodontitis prior to treatment but the periapical radiolucency is less than 2 mm in diameter and the root filling is satisfactory, then if symptom-free, the tooth should be treated in the same way as for vital teeth and restored without delay. In contrast, if the periapical radiolucency is greater than 2 mm in diameter, the root filling is technical satisfactory and the tooth is symptom-free, a short probationary period may be necessary. Regardless of whether a tooth is vital or non-vital, if the quality of the root filling is unsatisfactory, root canal retreatment should be considered prior to placement of the final restoration. Similarly, in cases where the prognosis is in doubt for whatever reason, it is prudent to delay the final restoration until there is clinical evidence, and in some cases, radiological evidence, of healing. If the decision is taken to wait for evidence of healing, it is imperative that the remaining tooth structure is protected by an adequate interim restoration, which also prevents coronal leakage. If adequate cusp coverage is difficult to achieve with interim plastic restorations, the placement of an orthodontic band is indicated to prevent tooth/root fracture.
RESTORATION CHOICE
The choice of restoration for an endodontically treated tooth is dependent on the amount of coronal tooth tissue left. In fact, this single most important factor will dictate the retention of the restoration and the fracture susceptibility of the tooth. Most randomized clinical trials on the restoration of endodontically treated teeth are focused on posterior teeth. The data on the survival of anterior teeth are only available from studies in which both anterior and posterior teeth have been included. 16,17 The suggestion from existing literature is there is a relationship between the fracture resistance of endodontically treated teeth and the residual amount of tooth structure. Hence, the life expectancy of endodontically treated teeth may not necessarily be increased by the choice of restoration but rather by the amount of tooth structure preserved. Anterior and posterior endodontically treated teeth present differing restorative demands. Anterior teeth may be less prone to fracture but compared with posterior teeth, aesthetics is a major consideration.
Anterior teeth
Composite resin restoration
In anterior teeth where there has been little previous restoration, a combination of composite resin placed over a base of glass ionomer cement may suffice. Composite resin is the most appropriate material for restoring the access cavity given its physical properties, high quality surface finish and the good seal achieved with bonding. Where an eugenol-containing root canal sealer has been used, care should be taken to ensure that the root canal filling is removed to the level of the cervical neck of the tooth if potential discoloration of the dentine is to be avoided. If the tooth is discoloured, bleaching techniques may be used, particularly, if the discolouration is mild (Fig.15.3). Internal and external bleaching techniques may be applied.
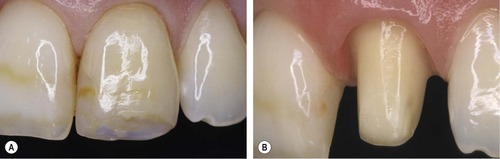
 |
 |
| Figure 15.3
A discoloured maxillary right central incisor due to trauma (A) following internal bleaching, an aesthetically improved result was obtained (B) without the need for a cosmetic restoration.
Reproduced courtesy of R Moazzez.
|
Ceramic or composite resin veneers
If the coronal tooth tissue loss is less than one-third, the palatal aspect of the tooth is to be preserved but it is impossible to obtain a good aesthetic result using a direct restoration, then a ceramic or composite resin veneer may be placed. Veneers normally cover the entire labial surface of the tooth including the incisal edge and through to the proximal contacts (Fig.15.4). Ceramic or composite resin veneers are seldom recommended for endodontically treated anterior teeth as it is not easy to incorporate the access cavity within such restorations.
 |
 |
 |
 |
 |
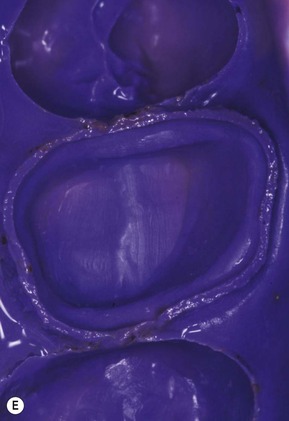
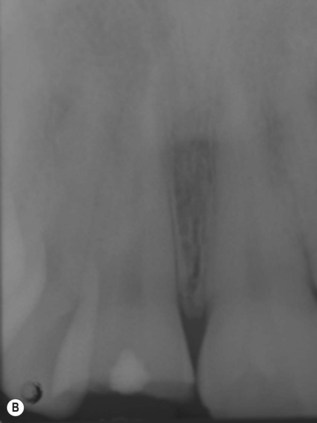
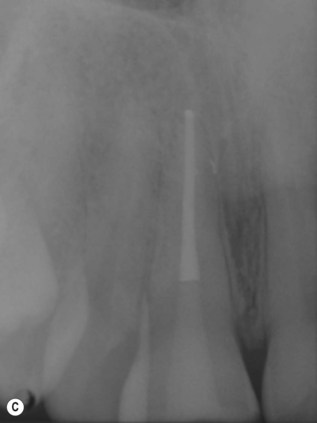
 |
| Figure 15.4
Traumatized maxillary central incisors (A) Radiograph showing crown fracture involving the pulp (B) and root canal treatment was needed (C). Ceramic veneers were then made for both teeth (D). These were cemented with composite resin under rubber dam isolation (E). An excellent aesthetic result was achieved (F) and the supragingival margins ensure good periodontal health.
|
Metal-ceramic crowns
Amongst non-adhesive techniques, metal-ceramic crowns have become the most commonly prescribed indirect restoration for endodontically treated anterior teeth. A reduction of the labial surface of approximately 1.8–2 mm is necessary. The extent of tooth reduction may compromise the strength of the remaining tooth tissue; so caution should be exercised before prescribing such a restoration. Far from preserving residual tooth structure, it may actually promote its loss. In general, crowning of anterior teeth is indicated if the amount of tooth structure left is not sufficient for a direct restoration and for aesthetic reasons.
Gold-porcelain infusion crowns
They offer two main advantages. The labial tooth reduction required (1–1.2 mm) is less extensive compared with that for a metal-ceramic crown; this is of potential benefit in terms of strength and tooth preservation. In addition, the colour of the underlying gold allows for a better aesthetic result, especially at the cervical area (Fig.15.5).
 |
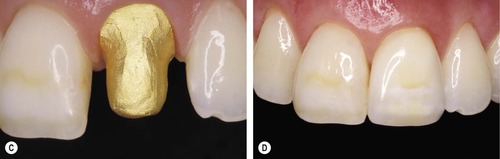 |
| Figure 15.5
A maxillary left central incisor is restored with a gold-porcelain infusion crown.
From Mannocci et al 200814 with permission of Quintessence Publishing Co. Ltd.
|
All-ceramic crowns
All ceramic crowns are more fragile than metal-ceramic crowns. However, the advantages of all-ceramic crowns are:
• labial tooth reduction required is, again, less than that for metal-ceramic crowns;
• absence of a metallic substructure allows a better aesthetic result, especially in areas close to the soft tissues.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


