15
Neurodevelopmental and Psychiatric Disorders
Neurodevelopmental and psychiatric disorders of particular importance to dentistry are discussed in this chapter.
Section 1. Neurodevelopmental Disorders
I. Background
Description of Disorder
Intellectual Disabilities (IDs)/Mental Retardation
ID is a disability with onset before age 18 years that is characterized by significant limitations both in intellectual functioning and in adaptive behavior, affecting many everyday social and practical skills.1
Down Syndrome (DS)
DS (Trisomy 21) is a congenital chromosomal abnormality characterized by systemic anomalies, ID, and a recognizable craniofacial appearance.2
Cerebral Palsy (CP)
CP is a general term used to describe a number of neuromuscular disorders that are present at birth or are acquired during infancy. CP affects muscle movement as a result of structural abnormalities or trauma to parts of the brain that control this function.
An International Workshop on the Definition and Classification of Cerebral Palsy, held in 2004, developed the following definition3:
Cerebral palsy (CP) describes a group of disorders of the development of movement and posture, causing activity limitation, that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain. The motor disorders of CP are often accompanied by disturbances of sensation, cognition, communication, perception, and/or behavior, and/or by a seizure disorder.
Autistic Spectrum Disorder (ASD)
ASD includes “classic” autism, Asperger syndrome, and atypical autism or pervasive developmental disorders (PDDs) not otherwise specified. ASDs are characterized by deficits in three major areas4:
- social interaction/relatedness;
- verbal/nonverbal communication;
- restricted interests, repetitive/stereotyped behaviors, and resistance to change.
Individuals can present with a wide variety of behavioral characteristics, ranging from mild to very severe involvement. However, these behaviors may change with the acquisition of other developmental skills. Asperger syndrome is a high-functioning form of autism with impaired social interactions, limited repetitive patterns of behavior, and delayed motor milestones and clumsiness. Common comorbidities include mental retardation (intelligence quotient [IQ] <70) in 70% and epilepsy in 25% of cases.5
Attention Deficit Hyperactivity Disorder (ADHD)
ADHD is a neurodevelopmental disorder that is characterized by an inability to regulate attention, often with displays of hyperactivity and impulsivity.4,6,7
Pathogenesis/Etiology
IDs/Mental Retardation
Genetic disorders are a leading cause of ID. There are over 800 syndromes associated with ID.8 Intrauterine exposure to toxins (e.g., fetal alcohol syndrome, anticonvulsant medications), intrauterine infections (e.g., cytomegalovirus, rubella, toxoplasmosis), metabolic disorders and neurodegenerative disorders can also cause ID in a child. Other etiologies include perinatal/postnatal conditions such as extreme premature birth, intraventricular hemorrhage, hypoxic–ischemic encephalopathy, traumatic brain injury, and meningitis.
DS
The genetic basis for DS is a mutation resulting in an extra copy of chromosome 21 (seen in 95% of cases). A much smaller number of cases (up to 5%) involve translocation or mosaicism of chromosome 21.
CP
CP may be attributed to structural abnormalities in the brain as well as the central nervous system (CNS) vascular insufficiency resulting in hypoxia to the developing brain. Risk factors for CP include:9,10
- intrauterine exposure to toxins or infections,
- preterm birth and low birth weight,
- multiple gestation,
- intrauterine growth retardation,
- maternal thyroid disorders,
- maternal seizure disorder,
- birth asphyxia,
- infections in postnatal period (meningitis, encephalitis),
- intracranial hemorrhage (postnatal),
- kernicterus (postnatal).
ASD
There is no known single cause of autism; etiologies are likely multifactorial. Current research is focusing on factors that could influence the development of the embryonic brain11:
- Genetics: High concordance in identical twins and first-degree relatives.
- Environmental and other possible factors:
- impaired methylation and gene mutations involving metabolism of vitamin D12;
- maternally derived antibodies, maternal infection, maternal teratogen exposure, heavy metal exposure, and folic acid supplementation12;
- paternal age at time of conception13;
- measles, mumps, rubella (MMR) vaccine has been implicated but rejected as a causative factor.14
ADHD
A precise etiology for ADHD has not been established. Studies of families with the disorder suggest a strong genetic component, possibly with altered function of neurotransmitters and structural abnormalities in the brain.6,7
Epidemiology
IDs/Mental Retardation
- Prevalence of ID is estimated at 1–3% in developed countries.
- Prevalence of severe ID in the United States is estimated at 3–4 per 1000 children and adults, while mild ID is much more common.15
Approximately 85% of people with ID are in the mild range with an IQ of 50–70, academically at the level of a sixth grader, and functionally able to live in the community with minimal support.16 ID itself is not associated with a shortened life span. However, life span may be decreased due to the underlying etiology for the ID. Higher rates of seizure disorders, gastrointestinal complications including feeding dysfunction and gastroesophageal reflux, and respiratory disease are common.
DS
- This occurs in 11.8/10,000 live births in the United States, with a higher rate associated with mothers who are ≥35 years old.17
- Approximately 400,000 people with DS currently reside in the United States.18
CP
- This is the most common congenital neuromuscular disorder.19
- Overall prevalence in developed countries is estimated at 2–3 per 1000 live births, with the rate holding steady for more than 30 years.10
- A higher prevalence exists in children born preterm.
Classification
CP can be classified according to the nature of the motor disorder19:
- spastic (70–80%),
- dyskinetic (10–15%),
- ataxic (5%).
CP can also be classified topographically, according to which parts of the body are affected:
- quadriplegia (all four extremities, trunk, and oromotor musculature),
- hemiplegia (one side of the body),
- diplegia (legs either solely or more than the arms),
- monoplegia (one limb—very rare).
Patients will often present with a diagnosis encompassing both type and location of disorder, that is, “spastic diplegia.”
ASD
- This occurs in between 1 in 80 and 1 in 240, with an average of 1 in 110 children in the United States.20
- Boys are four to five times more likely to have an ASD than girls.
- Prevalence has not been linked to social factors such as race, ethnicity, parental education, or socioeconomic status.
ADHD
U.S. prevalence rates of ADHD in school-age children range from 5.6% to 15.9%, with pronounced state-by-state variation, possibly due to differences in diagnostic testing. Boys are almost three times more likely to be diagnosed with ADHD than girls, although it is thought that some of this difference may be attributed to the fact that more boys display hyperactive/impulsive behaviors than girls.21
 Coordination of Care between Dentist and Physician
Coordination of Care between Dentist and Physician
Physicians may be the first to notice oral trauma or oral neglect and related infections in patients with neurodevelopmental disorders and should refer the patient to a dental provider for prevention and care. The dentist may require consultation with the physician for patients with complicated medical and behavioral issues.
 II. Medical Management
II. Medical Management
Identification/Medical History/Physical and Laboratory Examination
IDs/Mental Retardation
Individuals who are considered to be “intellectually disabled” must show deficits not only in cognitive functioning, but also in adaptive functioning (i.e., communication, self-care, home living, and social and interpersonal skills). Cognitive functioning refers to IQ levels, with an IQ below 70 indicating an ID (mean IQ = 100; 70 is 2 standard deviations below the mean).4
DS
Systemic anomalies commonly associated with DS include:2,22
- congenital cardiac anomalies (40–50% of infants),
- immune deficiencies (T- and B-cell defects, impaired cell, and humoral immune systems),
- overall hypotonicity,
- atlantoaxial instability (12–20%),
- intellectual disability (usually in the range of mild-to-moderate disability),
- increased risk for leukemia,
- increased risk for early-onset Alzheimer’s disease.
CP
The clinical picture of CP can vary greatly from mild to severe functional and systemic involvement. In addition to various medical specialists, a team of health-care professionals, including physical, occupational, and speech therapists may be required to optimize the individual’s quality of life. Medical complications associated with CP include but are not limited to:23
- intellectual disability (seen in 30–50%),
- seizures,
- gastroesophageal reflux,
- dysphagia,
- spinal disorders (scoliosis or kyphosis),
- joint contractures (secondary to spasticity).
ASD
The diagnosis of ASD is behaviorally based. There are no specific genetic, medical, or laboratory tests that are diagnostic for ASD. Deficiency in at least one of the areas of communication, socialization, or restricted behavior must be present before the age of 3. Formal diagnosis requires a two-stage process: developmental screening during “well child” checkups and if problems are detected, then the child should be referred for the second stage, which is a comprehensive evaluation by a multidisciplinary team.24
ADHD
Diagnostic criteria require characteristics to be evident by age 7 and must have had duration of at least 6 months. The disorder is classified into three distinct subtypes4:
- predominantly inattentive,
- predominantly hyperactive-impulsive,
- combined type.
Comorbidities include anxiety and depression. Adults with inadequately treated ADHD show a high incidence of illicit drug use, which may indicate an attempt to self-medicate.7
Medical Treatment
Table 15.1. Oral Side Effects and Interactions of Drugs Used in Neurodevelopmental Disorder (and Some Overlap with Psychiatric and Neurological Disorders)
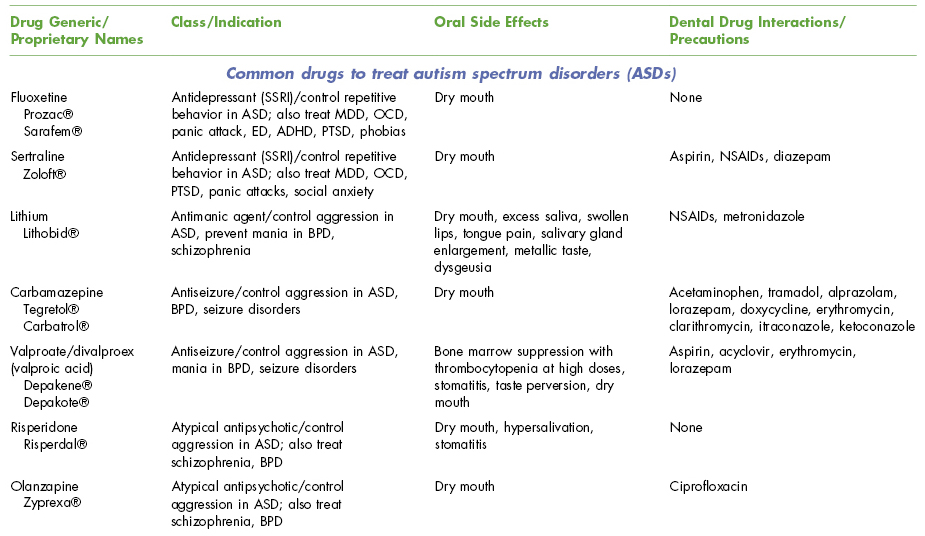
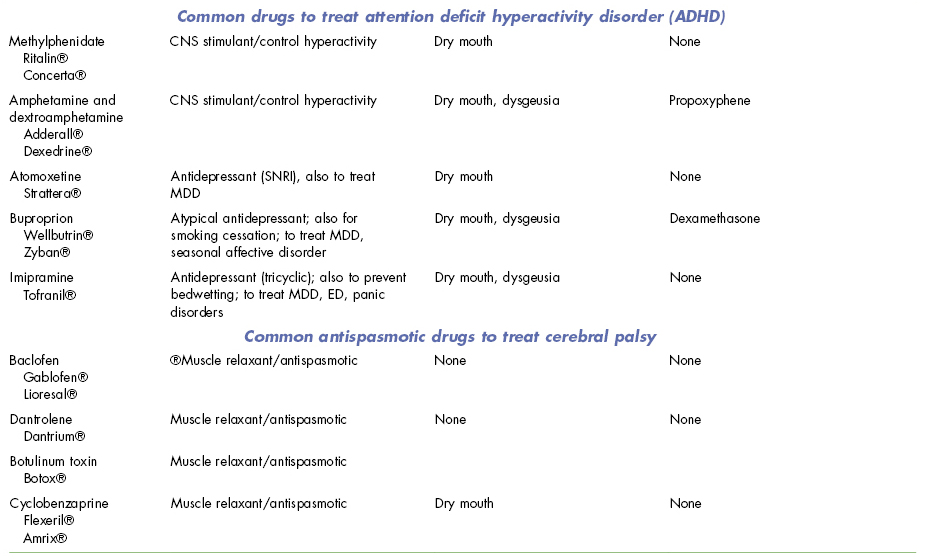
BPD, bipolar disease; CNS, central nervous system; ED, eating disorder; MDD, major depression; NSAIDs, nonsteroidal anti-inflammatory drugs; OCD, obsessive–compulsive disorder; PTSD, posttraumatic stress disorder; SNRI, serotonin–norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor.
 III. Dental Management
III. Dental Management
Evaluation
Important aspects of dental history include ascertainment of legal guardianship status for the patient, assessment of type and adequacy of patient oral hygiene and need for caregiver supportive oral care, past abilities to tolerate dental treatment in the dental office setting, need for anxiety management, sedation or general anesthesia to accomplish treatment, current oral health status, and ability to make improvements in oral health with coaching. The caregiver and legal guardian should be present and participate in interpreting or clarifying the patient’s unique communication style or to report on past dental history and challenges with patient communication and cooperation with dental care.
 Key questions to ask the patient (caregiver) with neurodevelopmental disorders
Key questions to ask the patient (caregiver) with neurodevelopmental disorders- What type of disorder does the patient have?
- What type of behaviors/symptoms does the patient have?
- Who is the patient’s legal guardian?
- How is oral hygiene accomplished? Does the patient receive assistance? What type, how often, and how well accepted is the assistance? Is there gum bleeding on assisted brushing?
- What attempts have been used to improve oral hygiene and how successful have they been?
- What is the patient’s diet and eating habits (sugar content and contact duration with teeth)?
- How has past dental treatment in the dental office setting been managed? Does the patient benefit from tell–show–do or special communication or relaxation/cooperation techniques?
- Does the patient benefit from previsit antianxiety medication use? What dose has been used? Has nitrous oxide/oxygen analgesia been tried? If so, was it successful?
- Do you feel medical stabilization (use of papoose board), conscious sedation, or general anesthesia will be needed to accomplish treatment?
- Has the (nonverbal) patient demonstrated any signs that he or she might be in pain?
- Can the patient indicate he or she is having pain? How is pain demonstrated?
 Key questions to ask the physician for the patient with neurodevelopmental disorders
Key questions to ask the physician for the patient with neurodevelopmental disorders- What has the patient’s behavior been like for office procedures such as blood draws and vaccinations?
- If general anesthesia is required, does the patient require other medical procedures that can be done at the same time as the dental care under general anesthesia if done in a hospital setting, for example, gynecological exam and Pap smear, blood draw for laboratory testing, and removal of impacted ear cerumen?
Oral Manifestations
DS
Orofacial features characteristic of individuals with DS, as seen in Fig. 15.1, include:2,22
- midface hypoplasia;
- underdeveloped palate with high palatal vault (results in relative Class III malocclusion);
- macroglossia (either true or relative due to small oral cavity) with subsequent strong gag reflex;
- fissured tongue that may protrude and contribute to halitosis (possibly secondary to chronic mouth breathing);
- large thick lips with hypotonia causing mouth drop and the lower lip to protrude;
- dental findings including microdontia, hypodontia, supernumerary teeth, morphological variants, delayed eruption, and maxillary impactions (secondary to underdeveloped palate).
Figure 15.1 Young lady with Down syndrome ready for her high school prom.

CP
As with medical issues, there is great variation in oral conditions associated with CP. Some of those seen most frequently include:26,27
- malocclusions (most frequently Class II, anterior open bite);
- bruxism (more prevalent in individuals with severe intellectual disability);
- persistent sialorrhea (hypersalivation with drooling; seen in individuals with dysphagia);
- extensive calculus deposits (associated with dysphagia, pooling saliva, possible gastrostomy tube feeding).
Dental Treatment Modifications
Traditional behavior management techniques such as tell–show–do are often successful. Direct uncomplicated language should be used, being mindful of the person’s biological age and being sure to maintain the person’s dignity by not talking “baby talk.” It is equally important to address the patient and not just the caregiver or guardian while explaining treatment and options. Issues of guardianship should be determined, and only legal guardians should sign consent if the patient is unable to do so. Treatment planning should be based on the principle of patient-centered care. Plans should start at ideal, and then be adapted or modified after considering the patient’s abilities, wants, and needs, as well as his or her ability to tolerate the treatment and maintain restorations.28
Oral hygiene and routine preventive care should be emphasized. For patients who cannot reliably swish and spit, chlorhexidine applied to the toothbrush with assisted brushing may be beneficial. Oral hygiene techniques for patients who resist caregiver help may need to be demonstrated to the caregiver. As shown in Fig. 15.2, a useful approach to assisted brushing (after the patient has made an attempt to brush his or her own teeth, if possible) is from behind the patient’s head, with the head supported.
Figure 15.2 Positioning for providing oral hygiene for a patient in a wheelchair.
From the Practical Oral Care for People with Cerebral Palsy. NIH publication No. 09-5192. Available at: http://www.nidcr.nih.gov/OralHealth/Topics/DevelopmentalDisabilities/PracticalOralCarePeopleCerebralPalsy.htm.

IDs/Mental Retardation
A number of factors can complicate oral health maintenance for individuals with ID. Patients may exhibit oral habits such as bruxism or other self-injurious behaviors, which are seen more frequently in individuals with low cognitive function and sensory impairments.
DS
Individuals with DS are at higher risk than the general public for the development and early onset of periodontal disease.2,22,29 Rates of periodontal disease have been reported as high as 90–96% in adults22 and may be due to the compromised immune response and abnormalities in capillary morphology and connective tissue.29
Although dental caries incidence in institutionalized children with DS whose diets are closely monitored is low, they maintain caries risk and should receive the same preventive considerations as other children. The deinstitutionalization of individuals with DS and subsequent “normalization” of their diets has led to a caries rate closer to that of the general population.22
 Risks of Dental Care
Risks of Dental Care
Hemostasis and Susceptibility to Infection
DS: Patients are more susceptible to infections due to immune compromise (lymphopenia and defects in neutrophil chemotaxis).30
Drug Actions/Interactions
ASD and ADHD: Common medications to treat ASD and ADHD may have interactions and side effects, particularly dry mouth that may require caries-preventive approaches with use of topical fluorides (see Table 15.1).
Patient’s Ability to Tolerate Dental Care
It is important from the start to determine each individual’s ability to communicate and cooperate.2,22 Cognition, communication, and behavior should be kept in mind when planning dental treatment. An awareness of each individual’s physical and behavioral limitations should guide the oral health professional when providing care. The goal should be to provide optimal oral care while using the least restrictive techniques.
The majority with mild-to-moderate behavioral concerns can be managed within the routine dental setting. For some individuals who have extensive treatment needs or difficult behaviors, it may be necessary to consider sedation or general anesthesia.
DS and CP: The combination of hypotonia and upper airway anomalies may increase risk for adverse events during sedation, factors that should be weighed when planning treatment modalities.
ASD: Patients often present behavioral challenges such as short attention span, rigidity of routines, hyperactivity, easy frustration, tantrums, and echolalia.31 Standard behavior management techniques such as tell–show–do, and immediate positive and negative reinforcement (paired with firmness, if necessary/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


