N2O/O2 Sedation in Pediatric Dentistry
CHAPTER OBJECTIVES
Upon completion of this chapter, the reader should be able to:
1. Recognize stages of child development according to Piaget.
2. Appreciate the guidance from the American Academy of Pediatrics (AAP) and the American Academy of Pediatric Dentistry (AAPD) regarding nitrous oxide/oxygen administration.
3. Understand the steps for administration of nitrous oxide/oxygen sedation in pediatric dentistry.
4. Appreciate how nitrous oxide/oxygen sedation is used with a variety of disciplines in children.
5. Recognize patient considerations related to working with children.
6. Understand the difference between rapid induction vs. the titration method for administration of nitrous oxide/oxygen sedation in children.
7. Understand safety considerations associated with pediatric patients and nitrous oxide/oxygen sedation.
1 Introduction and Background
Besides the use of N2O in general anesthesia, analgosedation produced by inhalation of a nitrous oxide/oxygen mixture is widely used in dentistry and medicine in a broad range of clinical outpatient settings to alleviate fear and anxiety associated with invasive and/or painful dental and medical procedures. Its excellent safety record, rapid onset of action, short duration of action, and ease of use contribute to its popularity not only in the United States but also in many other countries worldwide. 1–3 Because of its relative weakness as an anxiolytic, nitrous oxide is often combined with other volatile anesthetic gases,4,5 topical anesthetics, or various medications delivered by the enteral/parenteral route to enhance its effectiveness. All pediatric dentistry residency programs in the United States are teaching nitrous oxide inhalation analgesia as a behavior management technique.6
1. Training does improve safety and success rates. Although there was no difference in the overall success rates of both newly trained dentists and experts alike when they used a fixed 50% nitrous oxide/50% oxygen mixture in a variety of anxious adults, preschoolers, and patients with intellectual disability (N = 862 sessions in 662 patients), new trainees had a higher degree of failures when treating patients with intellectual disability as well as more minor adverse events such as respiratory, behavioral, and vasovagal effects.7
2. A 1993 survey of the membership of the AAPD8 found that 89% of the 1758 respondents used N2O to treat pediatric patients. Of those who used N2O/O2, most practitioners (87%) used the titration method of administration. The percentage of N2O administered varied, but rarely did concentrations exceed 50%. Most respondents indicated that 20% or fewer of their patients required either N2O/O2 alone or N2O/O2 in combination with other sedatives.
a. Seventy-four percent of the respondents did not use any monitors when N2O/O2 was used alone. However, when it was used in combination with other sedatives, the pulse oximeter was the single most frequently used monitoring device. A blood pressure cuff and precordial stethoscope were also used when N2O was combined with other sedatives.
b. When N2O/O2 was used alone, only 2% of the respondents experienced a compromised airway. This value increased to 33% when deeper sedation levels were achieved by combining N2O with other sedatives.
3. A 15-year follow-up survey9 of all 3315 active AAPD members (response rate 54%) about the use of sedative agents by pediatric dentists determined wide variation among practitioners regarding the use of sedation agents and their frequency of use. The results reflect that N2O alone or in combination with other agents is still used by many practitioners.
4. N2O/O2 significantly modifies uncooperative behaviors10 but not physiologic parameters in sedated children.11,12
5. Internationally, N2O/O2 sedation is being used successfully13,14 during extraction of first permanent molars15 or as a potential alternative to general anesthesia when treating children.15–17
6. Delivery of a 40% N2O/60% O2 combination significantly improved patient behavior without significantly affecting hemoglobin saturation or type of breath sound.18
2 Child Development
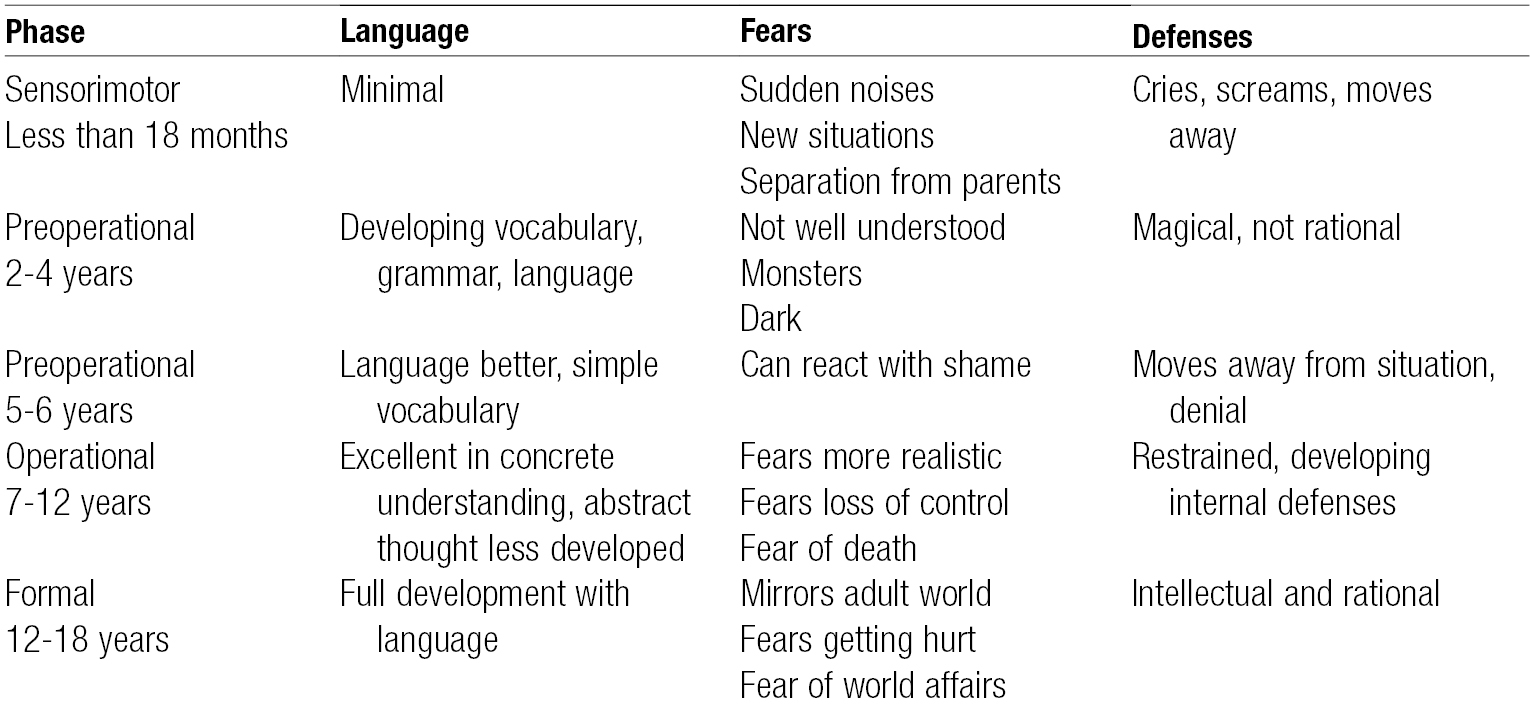
A. Piaget proposed a model for child development19 that addresses cognitive function (i.e., how a child thinks). According to this model, children move through four stages of development: sensorimotor, preoperational, concrete operational, and formal operational. He proposed that for cognitive development, the movement among stages is universal and invariant and proceeds in a fixed order (Table 15-1).
B. These stages indicate how normally developing children should be approached. Similar to adults, it is common for pediatric patients to have some anxiety regarding medical or dental treatment.
C. There are additional significant factors that affect the development of a child today. Changing patterns of child rearing, parental interactions and attitudes toward professionals, and individual child temperament and personality affect the way a child acts and reacts in any given setting.
D. It is important for health professionals and office staff to be educated about these factors, because understanding the pediatric patient’s needs and desires and those of the parents is imperative.
3 AAP and AAPD Guidelines
The American Academy of Pediatrics (AAP) and the American Academy of Pediatric Dentistry (AAPD) have jointly published guidelines20,21 intended for those practitioners who deliver sedation to children. These guidelines were developed in response to the increase in invasive diagnostic and minor surgical procedures being completed on either an elective or an emergent basis in settings outside of the operating room. They describe a unified approach regarding sedation for both dental and medical providers. The guidelines underscore the importance of careful preprocedural evaluation, appropriate fasting guidelines, airway evaluation, and use of appropriately trained individuals capable of monitoring the patient, as well as knowledge of associated risks, because sedation is different for children than it is for adults. They also reinforce safety as a primary concern and emphasize the fact that the provider must be able to rescue a child from a level of sedation deeper than that intended.
A. Terminology
1. The American Society of Anesthesiologists, The Joint Commission, the AAP, and the AAPD all use similar language with regard to the definitions of sedation categories.
2. The definitions of minimal, moderate, and deep sedation as well as general anesthesia can be found in Chapter 3.
B. Goals of Sedation
1. The goals of sedation as listed in these guidelines include (1) guarding the patient’s safety and welfare, (2) minimizing physical discomfort and pain, (3) controlling anxiety and maximizing amnestic potential, (4) controlling behavior and movement, and (5) returning the patient to a state where discharge is safe.
2. Selecting the lowest dose of drug, the fewest number of drugs, and the correct drug to meet the intended goal of accomplishing the procedure is recommended.
C. General Guidelines
1. The AAP/AAPD considers children who fall in ASA classes 1 and 2 appropriate for all levels of sedation. However, children in ASA classes 3 and 4 or those with special healthcare needs or abnormal airways require special consideration and medical advice.
2. A responsible adult should accompany a child to and from an appointment and care should be taken to ensure adequate monitoring of those who need to travel in a car seat. Caution for this situation corresponds to the potential for a child’s head to fall forward and obstruct the airway. When additional sedative medications have been administered to achieve moderate or deep sedation, two adults must be present to accompany the child home.
3. The guidelines state that the facilities and personnel must be able to manage all emergency and rescue situations. Appropriate training is necessary and emergency equipment must be available at the facility and able to be appropriately used if needed.
4. Informed consent from the responsible accompanying adult must be obtained and all instructions regarding the procedure should be completed while giving the adult ample opportunity to ask questions.
5. If immobilization devices are used, they are to be carefully positioned so that airway obstruction or chest restriction is avoided.
6. Administration of nitrous oxide (50% or less) with the balance as oxygen, without any other sedative, narcotic, or other depressant drugs before or concurrent with nitrous oxide, to an otherwise healthy patient in ASA classes 1 or 2 is considered minimal sedation.
7. If nitrous oxide is used in concentrations > 50% or combined with other sedative drugs, the likelihood for moderate or deep sedation increases and the care provider must be prepared to follow the appropriate guidelines for these deeper levels of sedations. Local anesthetics are not considered sedatives in the context of this guideline.
D. Guideline on Behavior Guidance for the Pediatric Dental Patient
1. This guideline22 describes 10 currently approved techniques ranging from tell-show-do to treatment under general anesthesia. They are divided into seven basic and three advanced techniques. On this continuum, nitrous oxide/oxygen administration is the last basic technique and represents the threshold to advanced modalities. It is described as a safe and effective technique to reduce anxiety and enhance effective communication.
E. Guideline on Use of Nitrous Oxide for Pediatric Dental Patients
1. This guideline23 summarizes the background and parameters of nitrous oxide/oxygen administration in dentistry. Its intent is to assist practitioners in developing appropriate modalities in its use for pediatric patients.
2. Nitrous oxide concentrations should not routinely exceed 50% and should be adjusted to correspond with the difficulty of the procedure.
3. Visual monitoring is recommended to assess the patient’s respiration and level of consciousness. If any other pharmacologic agent (except local anesthetics) is used in addition to N2O/O2, the monitoring guidelines for moderate/deep sedation must be met.
4. Fasting is not required for patients undergoing nitrous oxide analgesia/anxiolysis.
F. Parents’ and Providers’ Views
1. Among the various behavior guidance modalities, nitrous oxide/oxygen sedation ranks in the United States consistently high in parental acceptance, only second after tell-show-do.24,25 In Spain it trails tell-show-do, voice control, and active restraint,26 whereas parents in Arab countries rated it among the least approved techniques.27,28
2. Among pediatric dentists in Britain nitrous oxide inhalation sedation (NOIS) is the most popular form of sedation.2 In a survey they indicated that NOIS should be universally available to all children in both practice and hospital settings. However, they also cautioned that both parents and patients overestimate the help NOIS provides for local anesthesia administration and dental treatment. Significantly more dentists than parents believe that the child could have been managed without sedation and would not require it for further dental treatment.29
G. Nasal Mask vs. Endotracheal Delivery
1. Publications reporting nitrous oxide concentrations do not take into account the significant difference in end-expired nitrous oxide concentrations with each delivery system. As a result of air entrainment that is inevitable during delivery with a nasal mask, end-expired alveolar N2O concentrations are, on average, 63% below flowmeter settings.30 When volatile anesthetic gases are delivered with an endotracheal tube, such dilution with ambient air obviously does not occur.
2. It is therefore impossible to compare the effects of 50% nitrous oxide delivered during general anesthesia with the effects resulting from delivery of the same concentration from a flowmeter that feeds the typical nasal mask used in dentistry. Although both operators (anesthesiologist and dentist) state that they deliver a nitrous oxide concentration of 50%, end-expired alveolar N2O concentrations associated with nasal mask delivery are approximately half of those delivered with an endotracheal tube.31
H. Ethical Considerations
Nitrous oxide should complement, but not substitute, traditional basic behavior guidance methods for children. Thoughtless routine use without considering risks, benefits, and alternatives may lead to complacency and overuse whereas its particular convenience may lead to reduced attention to potential dangers and best practice methods.32,33
1. Practitioners should not yield to parents’ requests for N2O if the clinical situation does not justify it. Only a patient’s needs in a specific situation must justify its use, not parents’ or dentists’ desires for convenience or expediency.
2. Indiscriminate nitrous oxide application may result in its becoming a crutch for both the dentist and the patient.34 Enabling patients to routinely avoid fear and anxiety associated with dental treatment may do them a disservice because it prevents them from developing appropriate coping mechanisms.
3. Alternative nonpharmacologic modalities (such as communicative behavior guidance techniques) should always be considered first and discussed as part of obtaining parental consent.
4. Oral consent for nitrous oxide/oxygen sedation is acceptable as long as it is recorded in the progress notes, although written consent may foster increased attention and ultimately a better understanding.
4 Advantages/Disadvantages of Nitrous Oxide
A. Advantages
Nitrous oxide has an excellent safety record when used as a sole agent in subanesthetic concentrations. Unless used in situations where it is contraindicated, nitrous oxide/oxygen sedation lacks serious side effects.
1. Advantages of N2O/O2 sedation include a high success rate if the appropriate patient and situation are chosen. Its low blood solubility allows for rapid onset and recovery. Because gas concentrations are easily titratable, depth and duration of the desired effects can be varied quickly.
2. Nitrous oxide/oxygen sedation helps to calm patients and reduce their anxiety as well as aid in their ability to forget unpleasant memories to which they may have been exposed during treatment. As a result, the dentist may be able to accomplish more difficult procedures on young patients by working more efficiently, and delivering a higher quality of work because the patient moves less.
3. The number of appointments for a given treatment plan is often reduced because longer treatment times are tolerated since the passage of time becomes unclear to patients.
B. Disadvantages
1. The main disadvantage of nitrous oxide/oxygen is related to its relative weakness as an analgesic/anxiolytic: it requires some cooperation from the start. The more potent volatile anesthetic agents will render even the most uncooperative patient unconscious within 5 to 20 seconds, which is impossible with nitrous oxide without a hyperbaric chamber and a full face mask. In contrast, N2O/O2 sedation requires a patient who is capable (age, cognition, mental state) and willing to cooperate.
2. Because of its lack of potency, and also to reduce the need for deeper systemic sedation, topical and/or local anesthetics for additional pain control are still required.
3. From a practical standpoint, particularly in younger and/or smaller children, even a small-sized and properly placed nasal hood sometimes extends to the upper lip, making access to the anterior maxillary region difficult.
C. Efficacy and Safety
Nitrous oxide analgosedation has an excellent safety record for patients of virtually all ages.
1. No adverse events were recorded in a prospective study in 95.7% of 7802 cases of nitrous oxide administration for non–dental procedures by specifically trained registered nurses in patients between ages 33 days and 18 years.35 In 90.8% of applications, the [N2O] was > 50% and the typical duration was < 15 minutes (89.3%). Duration of N2O application rather than age or [N2O] delivered had the largest impact on adverse events. Compared to nitrous oxide applications less than 15 minutes, a 4.2 times greater likelihood of an adverse event was found for applications lasting between 15 and 30 minutes with the probability increasing 4.9-fold for durations > 30 minutes. The most frequent adverse events were vomiting (2.2%) and nausea (1.6%).
2. Stand-alone delivery of 50% to 70% N2O for non–dental procedural sedation in 762 patients ages 1 to 17 years resulted in 8.3% mild (vomiting and agitation) and 0.2% serious (chest pain and desaturation) adverse events. Mean preprocedural fasting time was 4.3 hours. The authors presented no data on the duration of nitrous oxide application and found no association between adverse event rates and the level of [N2O] administered. Sedation depth did not vary between children who were younger or older than 3 years of age, but was slightly increased with 70% N2O, although the difference was considered clinically insignificant.36
3. A French study reported on 638 nitrous-only sedations for dental treatment provided by 33 dentists in 549 patients with a median age of 15 years. Mean duration of administration of the 50% N2O/50% O2 Kalinox® premix was 22 minutes. The total rate of minor adverse events was 10% (e.g., nausea and vomiting 2.8%, euphoria 3.5%). They rated 93.7% of the sessions as successful. Most failures occurred in patients with intellectual disabilities.37
4. During laceration repair, continuous-flow N2O/O2 provided pain and anxiety relief with minimal adverse effects and shorter recovery than when midazolam was used.47
D. Potency
1. The authors of a systematic review of 36 studies (N = 2810 children) that compared 2 or more drugs/techniques/placebo that were used for sedation for dental treatment concluded that there is only very weak evidence that inhalational nitrous oxide is more effective than placebo,38 whereas for midazolam, the evidence was considered weak.
2. In a double-blind randomized controlled trial (RCT) of 50 patients ages 1 to 18 years who received either 50% N2O/O2 or placebo via full face mask for short painful procedures on skin, muscles, or bones/joints, pain scores in the placebo group were significantly higher and more rescue analgesia was required in patients not receiving nitrous oxide.39
3. A comparison of 50% to 70% nitrous oxide vs. IV ketamine (2 mg/kg) for laceration repair in 32 children (ages 3 to 10 years) found deeper sedation levels for the ketamine group, but comparable pain scores in patients and no significant difference in satisfaction scores of physicians, parents, and nurses.40 For very painful procedures (e.g., fracture reduction) sedation with N2O/O2 alone provided only limited success.41
5 Patient Assessment/Selection, Age Threshold, Indications
A. Patient Assessment
1. N2O/O2 sedation does not require an extensive physical evaluation of the child; however, both the AAP and the AAPD recommend a comprehensive health evaluation.
2. Patient assessment should focus on the following factors:
a. Medical conditions that constitute contraindications to nitrous oxide delivery
b. Previous sedation or anesthesia-related experiences
c. Allergies and adverse drug reactions
d. Medications that the patient is currently taking
e. Diseases and abnormalities
f. Pregnancy status
g. Hospitalizations
3. Anatomic factors that affect the respiratory system, such as anatomic airway anomalies or extremely enlarged tonsils and adenoids, are of relative importance because they can cause increased resistance to ventilation and N2O movement.
B. Patient Selection
1. In mild to moderately apprehensive children or adolescents whose cognition is developed enough that they are able or willing to interact with the care provider, N2O/O2 will generally produce a state of mild to moderate sedation. Therefore, best results are achieved in patients who are capable of understanding and following instructions.
2. It is important to remember that N2O/O2 should always be used in conjunction with—not as replacement for—other behavior guidance methods. When used in this manner, N2O/O2 can facilitate learning how to effectively cope with stress and anxiety associated with dental treatment.
3. Weight is usually a very important factor in the administration of proper medication dosages for patients, particularly children. However, weight is not a consideration for N2O/O2 administration when it is used as the sole agent.
C. Age Threshold
The customary age threshold in pediatric dentistry at which limited cooperation can be expected is around 3 years. At that time, normally developed children will have reached a level of cognitive development that will enable them to understand age-appropriate explanations and subsequently accept the nasal mask in a voluntary fashion during uncomplicated dental treatment of short duration and without restraint.
1. Children who do require significant physical restraint are generally so agitated that a nasal mask will not stay in place. Crying that occurs at the same time makes their breathing very irregular and increases the flow of nasal secretions.
2. The summary of these aforementioned factors makes it impossible in most cases to deliver with the typical nasal mask a flow of N2O/O2 that is steady and sufficient enough for effective sedation during dental treatment.
3. In medicine, N2O/O2 sedation is used for a variety of painful procedures including but not limited to venous cannulation, lumbar puncture, bone marrow aspiration, laceration repair, minor surgery, dressing changes in burn patients, or urinary catheterization. For such situations, the frequent and successful use of N2O/O2 sedation in patients younger than 3 years of age, some as young as 33 days, has been reported.35,39,41,42
4. However, the salient difference to dentistry is that all these medical applications do not require access to the oral cavity. Therefore providers are able to use a full face mask covering the nose and mouth to deliver N2O/O2, apply restraint, and/or maintain inhalation against a child’s will.
D. Typical Indications in Pediatric Dentistry
1. Characteristic indications in pediatric dentistry include easing a patient’s anxiety, raising the pain threshold, suppressing the gag reflex, and increasing tolerance to longer appointments because the passage of time becomes unclear to patients.
2. In young or borderline cooperative children, N2O/O2 sedation may make limited dental treatment possible that could not be accomplished without its sedative effects.
3. In older children, a care provider may be able to provide more difficult or extensive treatment utilizing N2O/O2 sedation.
6 Contraindications
A. Relative
It is imperative that dentists consult with the patient’s physician for all patients who present with significant underlying medical conditions and when the assessment is beyond their expertise. As a general rule, dentists should confer with the patient’s physician if the patient’s medical condition results in the patient being categorized as ASA 3 or 4.
1. Because nitrous oxide is a relatively weak anxiolytic and analgesic and requires patient compliance, it is ill suited to overcome the challenges posed by severe pain or moderate to severe anxiety and/or phobia associated with significant mental health problems.
2. Patients who resist mask placement and do not want to lose control because of a compulsive personality or patients with drug dependencies, claustrophobia, and defiant or hysterical behaviors are poor candidates for nitrous oxide application.
3.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses