Dental Hygiene Process of Care
The dental hygiene process—a systematic, problem-solving approach to quality oral health care—provides a framework for dental hygienists to individualize care and ensure that clients’ needs are met. This approach provides a framework for evidence-based decision making and sound clinical judgment while identifying and resolving client needs within the dental hygiene practice.1
The process is a standard of practice recognized by the American Dental Hygienists’ Association (ADHA), and an educational standard of the American Dental Association (ADA) Commission on Dental Accreditation.2,3 This chapter addresses the major components of the dental hygiene process of care: assessment, diagnosis, planning, implementation, evaluation that includes prognosis, legal–ethical considerations, and documentation.
Dental Hygiene Paradigm1
Basic Concepts
A A paradigm is composed of major concepts selected for study by a discipline
B The paradigm for the discipline of dental hygiene includes four concepts4
1. Clients—recipients of dental hygiene care; include persons, families, groups, and communities from all age, cultural, gender, and economic groups
2. Environment—external factors that affect the client’s optimal oral health; includes economic, psychological, cultural, physical, legal, educational, ethical, and geographic dimensions
3. Health and oral health—status of the overall health and the oral wellness or illness of the client
4. Dental hygiene actions—interventions that a dental hygienist initiates to promote wellness, prevent and control oral disease, and encourage active client participation and collaboration
C Dental hygiene practice—based on a systematic process of care that involves assessment, diagnosis, planning, implementation, and evaluation (Figure 15-1)
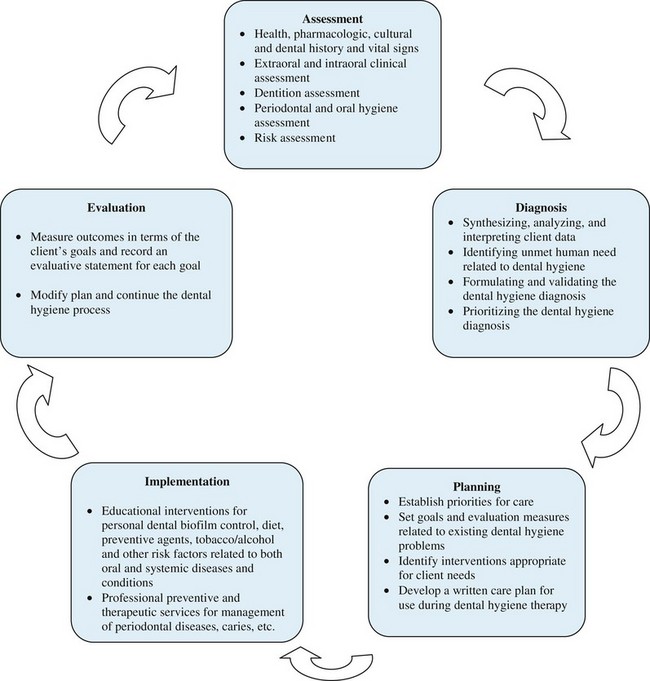
FIGURE 15-1 Dental hygiene process-of-care algorithm.
D The dental hygiene process of care provides a logical system for determining the health and disease status of the client and for selecting appropriate interventions and measuring treatment outcomes
E The dental hygiene process of care is integrated with the client’s comprehensive dental hygiene diagnosis and care plan
Human Needs Theory and Assessment1,5–7
See the section on “Human behavior principles” in Chapter 16.
Basic Concepts
A Most widely known model in the discipline of dental hygiene—human needs conceptual model; requires assessment of each client’s human needs as the framework for providing care
B Based on the theory that human activity is dominated by behaviors aimed at need fulfillment; an internal drive exists in all humans to satisfy unmet needs; unmet needs motivate specific behaviors to eliminate the perceived deficit; the model encourages establishing an environment that is more client oriented than task oriented
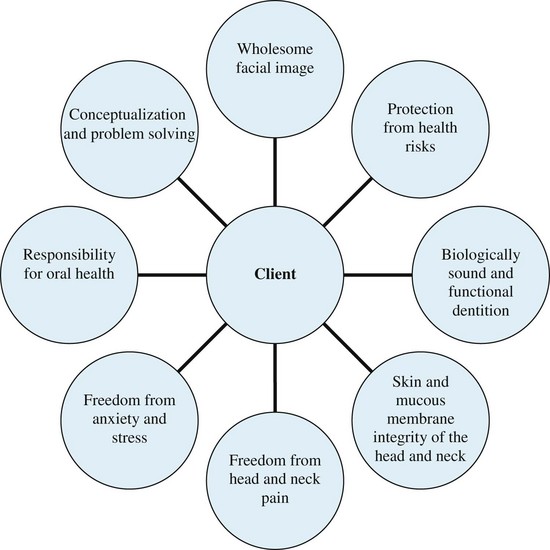
C The human needs model uses eight needs relevant to oral health that should be considered in the implementation of the dental hygiene process of care8 (Figure 15-2)
D During baseline assessment, deficits in eight human needs are identified, and the dental hygiene diagnosis is made; planning, implementation, and evaluation of dental hygiene care are carried out to address the client’s unmet needs
E Human needs assessment form—an instrument to assist in the summarization and organization of gathered assessment data; used to provide a written record of unmet needs, dental hygiene diagnoses, client goals, care plans, and outcome evaluations of dental hygiene care (see Figure 15-3)
Assessment
Basic Concepts
A Definition—comprehensive and systematic collection, analysis, and permanent documentation of data to identify the client’s needs and oral health problems
B Assessment—first phase of dental hygiene process of care
C Data collection—continuous process of collection, documentation, and analysis of objective and subjective data needed to provide comprehensive care
D Data are continuously updated and documented during the dental hygiene process of care
E Data are collected by interview, questionnaire, observation, measurement, and examination
F Data recordings are discussed with the client and other health care professionals responsible for client care
G Data collection and documentation—includes comprehensive personal, health, and dental histories; pharmacologic history; identification of the client’s chief concerns and human needs; clinical examination; periodontal examination; analysis of appropriately updated diagnostic radiographs; microbiologic or other tests for assessing the periodontal status of selected patients or sites also may be indicated9
Health History Evaluation
A Health history—taken to identify and evaluate predisposing conditions and risk factors that may affect dental hygiene care, client management, potential for an emergency, and treatment outcomes9
1. Such conditions and factors include, but are not limited to, allergies, diabetes mellitus, hypertension, osteoporosis, cardiac and pulmonary diseases, pregnancy, tobacco use, substance abuse, medications
2. In the presence of a condition that, in the judgment of the dental hygienist, requires further evaluation, consultation with an appropriate health care provider should be obtained
B Health history form—legal document that provides past and present information about the client’s health to meet the client’s human need for safety10
1. Provides baseline information about the client’s health status and assists in medical and dental diagnoses
2. Information used to assess the overall physical and emotional health of the client
a. Conditions that necessitate precautions to ensure the client’s need for safety is met during health care procedures and that medical emergencies are prevented
b. Conditions that require the client to be referred to a physician
c. Diseases, conditions, or medications that contraindicate dental or dental hygiene care
d. Previous history of reactions to medications or drugs
e. Infectious diseases that could endanger other individuals
f. Physiologic state of the client, including pregnancy, puberty, menopause, and use of hormones
3. Health history questionnaire should be completed in ink, and comprehensive information should be recorded on a questionnaire form or a summary sheet; this may also be a component of the electronic client record
4. The health history should be reviewed by the client and the dental hygienist and updated at each subsequent visit
5. The client should sign the written health history form at each appointment to confirm its accuracy; if the client is a minor, a parent or legal guardian should sign and date the health history form; electronic signatures are used in the electronic client record
6. The dental hygienist should sign the health history form at each appointment to indicate that medical and pharmacologic updates were obtained and verified; electronic signatures are used in the electronic client record
7. The health history form should be thorough but not contain redundant information and should use simple language to facilitate understanding
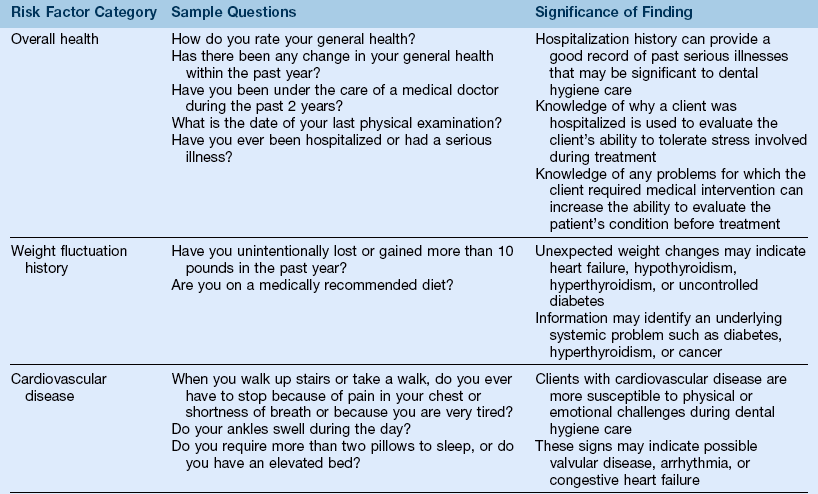
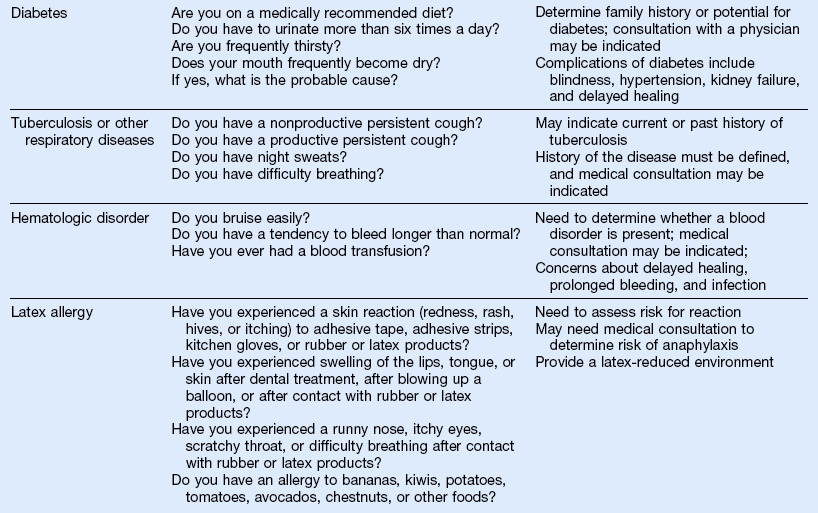
8. The health history form questions may include those shown in Figure 15-4.
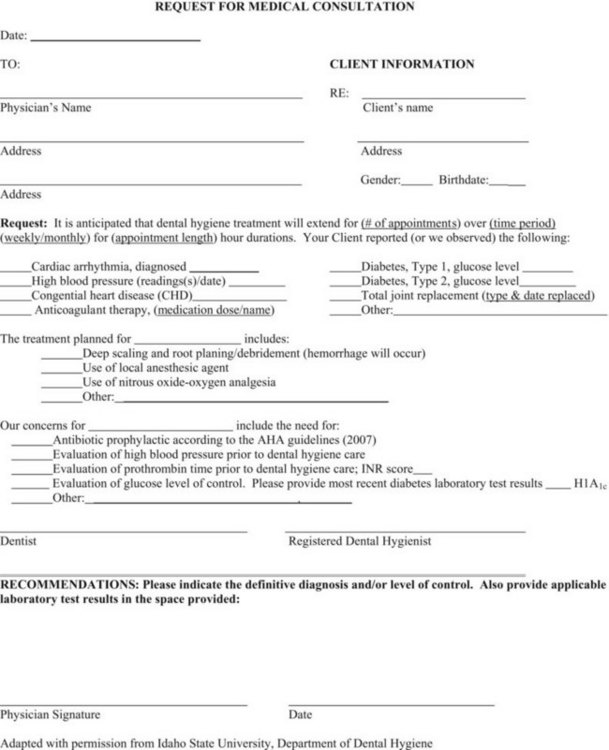
FIGURE 15-4 Request for medical consultation.
a. Personal, social, and cultural histories related to health and disease
b. Dental history information should include:
(1) Main concern—why the client is seeking dental or dental hygiene care
(2) In the case of new clients, the date of the last dental or dental hygiene care received to determine responsibility for oral health
(3) Areas of pain or discomfort identified during interviewing, but not associated with client’s main concern
(4) Nervousness or anxiety about treatment; history of an upsetting experience; the client’s need for freedom from anxiety and stress should be addressed
(5) Pain, swelling, or bleeding in gums
(6) The client’s satisfaction with his or her teeth and oral health
(7) Past or current orthodontics, periodontal surgery, extractions, temporomandibular joint (TMJ) problems, occlusal equilibration, fixed and removable dentures
(8) Oral habits such as clenching or grinding, biting lips or cheeks, mouthbreathing, and holding foreign objects between teeth
e. Radiographic history information (see the section on “Ethical considerations regarding the use of ionizing radiation” in Chapter 6)
(1) Purpose—the radiation exposure history of the client should be obtained to make safe decisions for radiographic prescriptions
f. Health history information (see Chapters 7, 8 and 19 for more detailed discussions of conditions) should include:
(1) Screening questions designed to assess risk factors or undiagnosed diseases and to enable the clinician to determine the need for a physician consultation or referral before dental hygiene care (Table 15-1)
(2) Detailed questions designed to identify diseases or conditions that a client previously had or currently has and to determine the need for precautionary measures, physician consultation before dental hygiene care, or need for antibiotic prophylaxis (Table 15-2)
TABLE 15-2
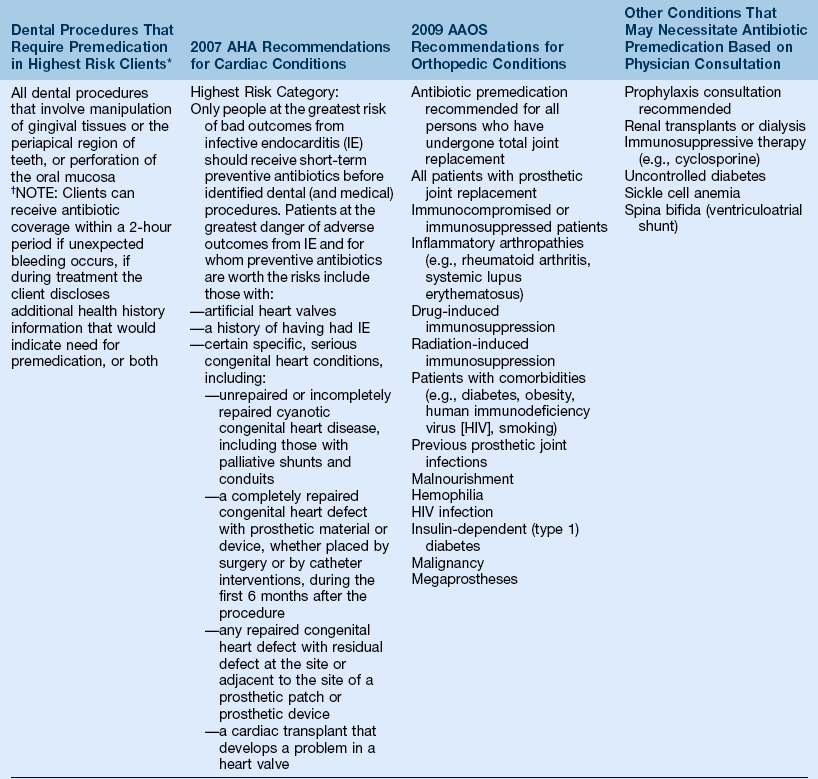
*Every attempt should be made to complete procedures and services in as few appointments as possible; follow-up appointments should be scheduled at least 9 days apart if client is premedicated.
†Clinical judgment may indicate antibiotic use in selected circumstances that may cause significant bleeding.
Adapted from Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease: Prevention of infective endocarditis: Guidelines from the American Heart Association, by the, Circulation, e-published April 19, 2007: Available at www.americanheart.org/presenter.jhtml?identifier=3004539: Accessed March 15, 2011; and from American Academy of Orthopedic Surgeons American Association of Orthopedic Surgeons: Antibiotic prophylaxis for bacteremia in patients with joint replacements, Available at http://www.aaos.org/about/papers/advistmt/1033.asp: Accessed March 15, 2011.
(a) When practitioner questions the client regarding his or her disease status, specific information should include:
[2] Treatment received in the past
[3] Severity of disease or extent of damage
[4] Type of current medical care
[5] Results of follow-up testing
[6] Classification of the client’s risk for a medical emergency using the American Society of Anesthesiologists (ASA) Physical Status Classification System (Table 15-3)
TABLE 15-3
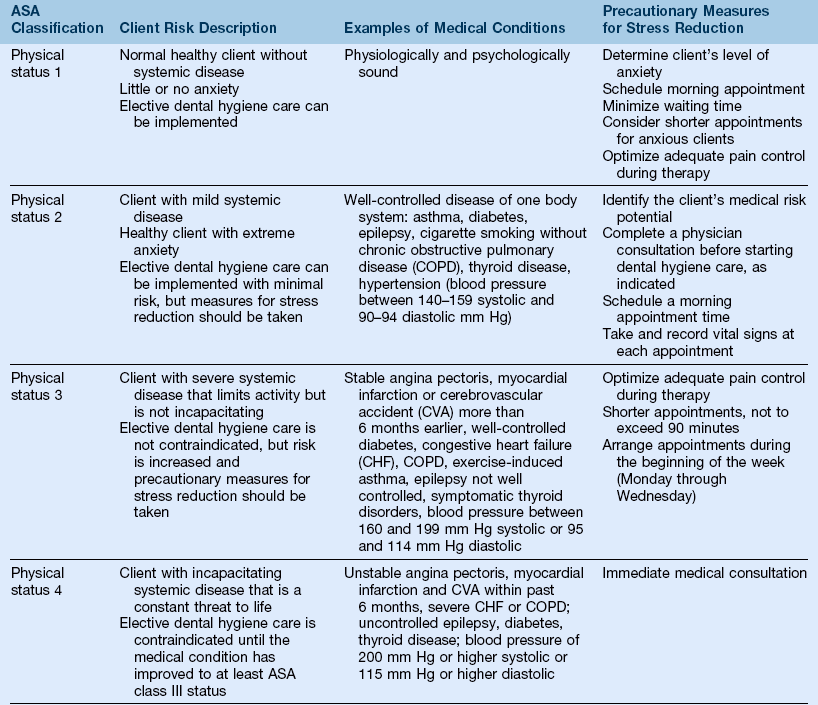
Adapted from American Society of Anesthesiologists: ASA physical status classification system: Available at www.asahq.org/clinical/physicalstatus.htm:. Accessed May 30, 2011; Malamed SF: Knowing your patients, J Am Dent Assoc 141:3S–7S, 2010. Note: Physical statuses 5 and 6 are used primarily in medical practice.
(b) Questions regarding cardiovascular disease (CVD) are significant because clients with various forms of CVD are especially vulnerable to physical or emotional challenges that may be encountered during dental hygiene care; for most CVDs, the stress-reduction protocol, based on the ASA system, is necessary (see the sections on “Vasoconstrictors” in Chapter 18; “Congenital heart disease,” “Cardiac arrhythmias/dysrhythmias,” “Hypertensive disease,” “Ischemic heart disease,” “Cerebrovascular disease,” and “Congestive heart failure” in Chapter 19; and “Vital signs,” in Chapter 21)
[1] Hypertension can result in myocardial infarction (MI) and stroke and contribute to arteriosclerosis, impaired kidney function, and cardiac enlargement; hypertension guidelines must be followed during professional care to reduce the risk of a medical emergency (Table 15-4)
TABLE 15-4
Classification of Adult Blood Pressure and Precautionary Measures
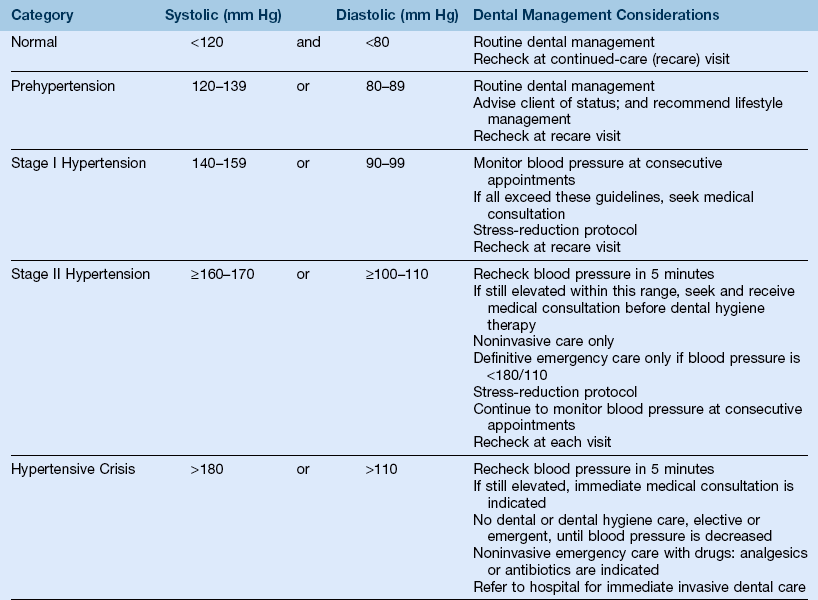
From Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., et al: Seventh Report of the Joint National Commission on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, Hypertension, 42:1206–1252, 2003; Little JW, Miller C, Rhodus NL, Falace D: Dental management of the medically compromised patient, St Louis, 2008, Mosby; Adapted from U.S. Department of Health and Human Services; National Institutes of Health; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program: JNC 7 Express. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Institutes of Health/National Heart, Lung, and Blood Institute, Bethesda, MD, NIH publication 03-5233, 2004: Available at http://www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.htm; Accessed March 15, 2011; and Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.
[2] When CVD is identified, it is important for the clinician to conduct a thorough interview to assess the severity and level of control of disease and to determine alterations in care (e.g., physician consultation, antibiotic prophylaxis, stress reduction protocol)
[a] Clients undergoing corrective surgery for congenital heart disease and have prosthetic material or device are susceptible to transient bacteremias for up to 6 months and must receive antibiotic prophylaxis; at 6 months after surgery, antibiotic prophylaxis is not usually recommended (see Table 15-2)
[b] When antibiotic prophylaxis is necessary, 9 to 10 days should be scheduled between appointments to allow oral bacteria to return to the original state; clients currently on an antibiotic regimen must use an alternative regimen of antibiotic therapy; if antibiotic medication is inadvertently missed, administer within 2 hours after the procedure
(c) Questions regarding diseases of the immune system and blood disorders assess the client’s potential risk for infection in dental hygiene care and his or her ability to handle stress through the appointment; primary concerns include prolonged bleeding, delayed healing, and secondary infections; physician consultation may be required for more chronic or involved conditions
[1] In the case of clients with diabetes, concerns about a hypoglycemic incident, susceptibility to oral infections (abscesses and periodontal diseases), impaired wound healing, and impaired glycemic control because of the presence of periodontal disease exist; consultation with a physician is indicated in most cases and referral is based on health history, dialogue, and oral conditions
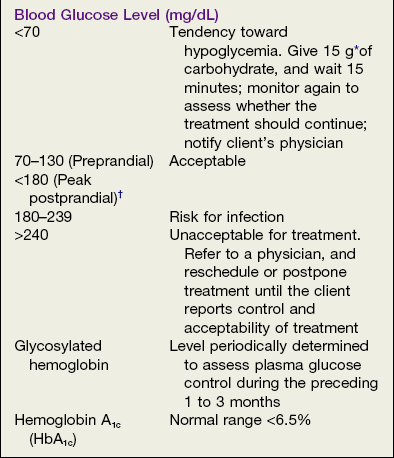
[2] Oral assessment should be initiated to determine the presence of infections and the extent of periodontal disease before consultation with the appropriate physician; glycated hemoglobin values (A1c) and blood glucose levels are requested from physician; the client should be asked to bring his or her glucometer, or a glucometer should be available in the oral care facility (Box 15-1)
[3] In clients with well-controlled diabetes, no alteration of the care plan is indicated unless complications of diabetes such as hypertension, congestive heart failure (CHF), MI, angina, or renal failure are present
[4] Clients with controlled diabetes should eat before appointments; appointments should be scheduled no later than midmorning, and a sugar source must be available in the oral care facility in case of any incidence of hypoglycemia or hyperinsulinism
(d) Metabolic syndrome (MetS) is closely associated with insulin resistance, in which the body cannot use insulin efficiently; patients with MetS are at increased risk of coronary heart disease, stroke, peripheral vascular disease, and type 2 diabetes
[1] MetS is identified by the presence of three or more components: obesity measured by waist circumference (men >40 inches and women >35 inches), fasting blood triglycerides (>150 mg/dL), blood high-density lipoprotein (HDL) cholesterol (men <40 mg/dL and women <50 mg/dL), blood pressure (>130/85 mm Hg), and fasting glucose (>100 mg/dL)
[2] Physician referral, medical consultation, or both may be required for clients who do not have regular medical care to determine the presence of associated conditions or the level of control of existing conditions
(e) Questions regarding respiratory disease or chronic obstructive pulmonary disease (COPD) assess the level of compromised respiratory function; clinicians should use precautionary measures to avoid further depression of respiration (see the section on “Chronic obstructive pulmonary disease” in Chapter 19)
(f) Musculoskeletal system disorders may be associated with chronic use of salicylates or nonsteroidal anti-inflammatory drugs (NSAIDs), which can alter blood clotting and corticosteroid therapy and increase the risk of acute adrenal insufficiency
(g) Neurologic and psychological disorders must to be identified and the degree of control determined; medications used to control seizures can cause drug-influenced gingival enlargement, and psychiatric drugs have the potential to interact adversely with the vasoconstrictors in local anesthetic agents
(h) Other disorders such as glaucoma, sexually transmitted infections (STIs), herpes, chemical dependency, and tobacco use have significant implications for treatment: in glaucoma, anticholinergics are contraindicated because they increase intraocular pressure; chemical dependency and tobacco use are risk factors for infectious diseases, malignancies, CVD, pulmonary diseases, and periodontal diseases; dental hygiene care for clients with active herpes or STIs should be postponed until the disease is no longer active
(i) The physiologic state of women identifies their status related to pregnancy and endocrine changes
(j) The identification of the risk of latex allergy is essential to reduce the chances of an allergic reaction; types of reactions include irritant contact dermatitis, allergic contact dermatitis (delayed hypersensitivity), and latex allergy
[1] Irritant contact dermatitis,—the most common reaction; causes dry, itchy areas of irritation on the skin
[2] Allergic contact dermatitis (type IV hypersensitivity reaction)—results from exposure to chemicals added to latex during harvesting of rubber, processing, or manufacturing
[3] Latex allergy, or immediate allergic urticaria (type I hypersensitivity reaction)—results from certain proteins in latex rubber; symptoms range from skin redness, rash, hives, or itching to runny nose, itchy eyes, asthma, and anaphylaxis
[4] Clients at risk for latex reaction should be treated in a latex-reduced environment; physician consultation is indicated for clients with risk of an anaphylactic reaction
(k) Listing of current medications—used to determine medications taken by the client and possible interactions with other medications; these medications may be the only clue to the client’s existing condition (Physicians’ Desk Reference or Mosby’s Dental Drug Reference can help with the identification of adverse reactions, precautions, contraindications, and dental considerations)
(l) Identification of medication allergies informs health care professionals of the client’s previous adverse reactions to medications
(m) Vital signs (see the section on “Vital signs” in Chapter 21)
[1] Vital signs are values given to measurements of blood pressure, respiration, pulse, and temperature; are important as they serve as a baseline in a medical emergency
[2] Abnormal or elevated blood pressure values should be brought to the client’s immediate attention; on the basis of the blood pressure values, monitoring of pressure at every appointment or a physician consultation may be required before initiation of dental hygiene care (see Table 15-4)
[3] Blood pressure, respirations, and pulse are measured and recorded before the administration of local anesthetic agents or nitrous oxide–oxygen analgesia
(3) Conditions being treated with medications—may influence or contraindicate certain procedures; for example, anticoagulant therapy may require a lower dose; antihypertensive drugs may alter the choice of local anesthetic; antipsychotic medications may alter the choice of nitrous oxide–oxygen analgesia (see the sections on “Anticoagulants” in Chapter 11; “Toxicity,” “Vasoconstrictors,” and “Nitrous oxide–oxygen conscious sedation” in Chapter 18; and Chapter 21)
(4) Physician consultations—may be necessary, depending on the information obtained from health history or physical examination; written documentation from the physician is necessary (Figure 15-1)
9. Health history information is gathered through interviews, written questionnaires, or a combination of both
a. The interview method allows the dental hygienist to develop client rapport and ensures that the client understands the questions
b. The self-administered written questionnaire is the most common format used to gather information pertaining to the client’s health status
c. Use of both the interview and the written questionnaire is the best approach to collect accurate and comprehensive health information
Extraoral and Intraoral Assessment
A Purpose—to assess and recognize deviations from normal conditions significant to the client’s health
B Establishment of an assessment sequence that is followed systematically
1. Skills used in performing extraoral and intraoral examination include direct observation, palpation, auscultation, and olfaction
a. Direct observation—visual inspection techniques used to examine the client’s movement, body symmetry, color, texture, contour, consistency, and form of skin and mucous membrane
b. Palpation—sense of touch used to examine for tenderness, texture, masses, and variations in structure and temperature within the head and neck region. Forms of palpation include:
(1) Digital palpation—use of single (index) finger to move or press against the tissue of the floor of the mouth or hard palate
(2) Bi-digital palpation—use of one or more fingers and thumb to move or compress the tissue of lips, tongue, cheeks, and vestibule
(3) Bimanual palpation—simultaneous use of the index finger of one hand and the fingers and thumb of the other hand to move or compress the tissue of the floor of the mouth
(4) Manual palpation—use of all the fingers of one hand to move and compress tissue to assess cervical lymph nodes
(5) Bilateral palpation—use of both hands simultaneously to move or press the tissue on the contralateral sides of the head to assess the submandibular nodes, TMJ, inferior border of mandible, and temporalis and masseter muscles
(6) Circular compression—use of fingers that move in a rotating, circular motion while slight pressure is applied
c. Auscultation—listening to and detecting sounds made by the body, for example, clicking (crepitation) of the TMJ; speech disorders; and vocal hoarseness
d. Olfaction—use of the olfactory sense to detect variations in breath odors such as alcohol breath, fruity ketosis (diabetic acidosis), and halitosis associated with dental caries, periodontitis, and necrotizing ulcerative gingivitis
2. Extraoral examination procedure (see Chapter 4)
(1) The overall appearance of client should be assessed via visual inspection
(2) The symmetry of skin, eyes, nose, and ears should be observed; areas of unusual discoloration should be inspected
(a) Skin (see the section on “Skin diseases” in Chapter 8)
[1] Normal texture is continuous, firm, and pigmented in relation to normal variations associated with race and ethnicity
[2] Abnormal textures or pigmentations should be recorded (e.g., scarring, swelling, moles, freckles, pallor, redness, severe acne, tumors, jaundice)
[3] Abnormal lesions should be measured and documented in writing, with details about color, size, shape, and surface texture
[1] Face and head should be symmetrical and have normal function
[2] Asymmetry or lack of function may be associated with injury, Bell’s palsy, tumor, abnormal growth and development, difficulty swallowing, Parkinson’s disease, Tourette’s syndrome, and abuse
[3] Facial expression can indicate the client’s general frame of mind (e.g., anxious, happy, sad, angry)
(c) Eyes (see the section on “Visual impairment” in Chapter 19)
[1] Breathing should be assessed; flared nostrils or ragged breath could indicate difficulty breathing
[2] An enlarged, bulbous, and red nose may be associated with an overgrowth of sebaceous and sweat glands from alcohol abuse (rhinophyma)
(e) Ears (see the section on “Hearing impairment” in Chapter 19)
(3) The symmetry of bones, muscles, lymph nodes, and salivary glands should be observed
(a) The inferior border of the mandible should be assessed for asymmetry by using bimanual palpation from the midline to the posterior angle
(b) The TMJ and the muscles of mastication should be inspected
[1] The TMJ should be assessed for deviation, pain, crepitus, grinding, and reduced range in opening or closing; evaluated via client interview and bilateral palpation with index fingers anterior to outer meatus; client is asked to open and close the mouth slowly several times; any deviation or symptomatology is recorded
[2] Masseter and temporalis muscles are assessed for overdevelopment, pain, swelling, and unusual hardness by using bilateral circular compression; the client is asked to clench the teeth together while the muscles are palpated
(c) The mentalis muscle is assessed for overdevelopment and smoothness of contraction during the swallowing movement; evaluated by digital palpation; tissue is moved over the mandible and he client is asked to swallow
(d) The larynx is assessed for unrestricted movement by bimanual palpation; the larynx is gently moved from side to side to check movement
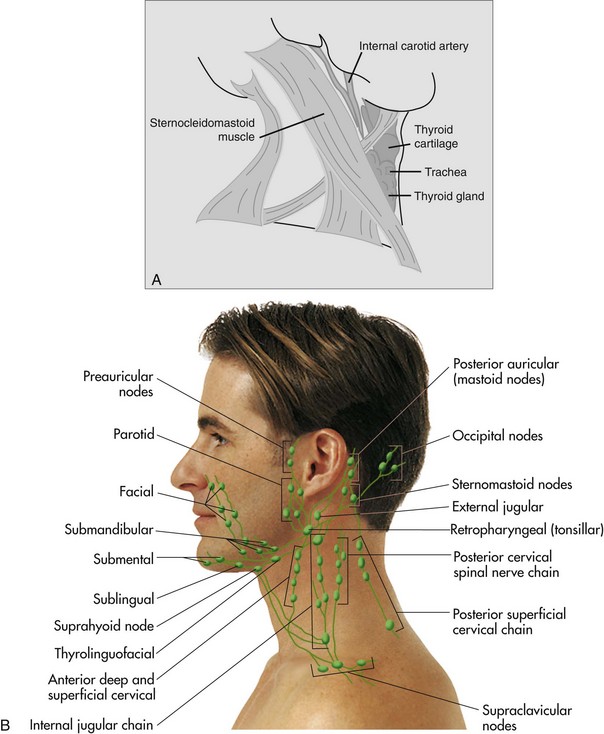
(e) Lymph node chains are assessed (Figure 4-7, Chapter 4)
[1] Occipital lymph nodes are assessed for pain, swelling, enlargement, unusual hardness, or fixed position by using bilateral palpation
[2] Auricular and parotid lymph nodes are examined for pain, swelling, enlargement, unusual hardness, or fixed position by using bilateral palpation
[3] Superficial cervical lymph nodes are assessed for pain, enlargement, unusual hardness, and fixed position by placing the client’s head to one side with the chin slightly lowered and by palpating with fingers along the sternocleidomastoid muscle
[4] Deep cervical lymph nodes are examined for pain, enlargement, unusual hardness, and fixed position by placing the client’s head upright and by palpating the deep tissues along the sternocleidomastoid muscles with the thumb and fingers
[5] Submental and submandibular glands are examined for asymmetry, noncontinuous borders, pain, tenderness, swelling, enlargement, unusual hardness, or difficulty in swallowing by bilateral digital palpation
(f ) The thyroid gland is assessed for asymmetry and enlargement by a combination of bi-digital palpation and circular compression; the client is asked to sit upright and to swallow (see Figure 4-8, Chapter 4)
(g) Parotid glands are examined for pain, swelling, enlargement, and hardness by using bilateral circular compression; salivary flow can be observed at the opening of Stensen’s duct when the gland is compressed
3. Intraoral examination procedure
a. Screen the client to detect lesions that may be pathologic, particularly lesions that may be cancerous
b. Prevent the development of advanced, irreversible, or untreatable oral disease through early recognition of initial lesions
c. Oral piercing is a popular form of body art
(1) Inspect the tongue, lips, cheeks, frenum, and uvula for piercings
(2) Barbells and rings are the most common types of jewelry
(3) Complications from piercing include excessive hemorrhage; transmission of communicable diseases; nerve damage; infection; bacteremia; Ludwig’s angina; cracked, fractured, or abraded teeth; recession; dehiscence; aspiration or ingestion of jewelry11
(4) Jewelry should be removed during the radiography procedure
d. The oral mucosa, lips, floor of the mouth, tongue, salivary ducts, hard and soft palates, and oropharynx should be examined and evaluated (see Table 5-1 and Figures 5-1 to 5-8 in Chapter 5)
(1) The lips are examined by visual inspection and palpation for:
(a) Changes in size—may be caused by swelling or allergic reaction
(b) Chapping—may be caused by mouth breathing or nutritional deficiency
(c) Blistering—may be associated with herpetic lesions
(d) Cracking—may be associated with angular cheilosis, candidiasis, or vitamin B deficiency (see the section on “Vitamins” and Table 12-4 in Chapter 12)
(e) Scar tissue or irritations—may be associated with habitual lip biting or trauma; bruising at commissures may indicate binding or gagging associated with physical abuse
(f) Abnormal texture, lack of moistness or firmness—may be associated with dehydration and excessive sun exposure
(g) Limitations of opening; muscle elasticity, and muscle tone—may be associated with stroke or TMJ dysfunction
(2) Labial and alveolar mucosa and the gingiva are examined by using bilateral and bi-digital palpation
(a) Signs of tissue trauma from biting, toothbrush abrasion, burns, or physical abuse; lacerated or torn frenum (tissue tags) may indicate binding, gagging, or forced feeding
(b) Ulcerated lesions such as herpetic lesions or aphthous ulcers
(c) Tight or low frenum attachments, which can cause gingival defects such as recession and loss of attached gingiva
(d) Spit tobacco lesion (leukoplakia), hyperkeratinized tissue; white, sometimes corrugated, in appearance; the client should be taught self-assessment techniques
(e) Amalgam tattoo, blue-and-black coloration, size variations—can be found on any area of soft tissue (see section on “Abnormalities of oral soft tissues” in Chapter 8)
(3) The buccal mucosa is assessed by using bi-digital palpation; the mouth mirror is used to reflect light and to inspect the buccal mucosa
(a) The buccal mucosa is examined for color and texture
(b) The parotid papilla and duct (Stensen’s duct) are evaluated; the duct is palpated to assess salivary function
(c) Atypical findings include traumatic lesions related to cheek biting, linea alba adjacent to occlusal plane, ectopic sebaceous glands (Fordyce granules)
(4) Hard and soft palates and alveolar ridges are examined by visual inspection; the mouth mirror is used to reflect light; digital palpation is used on the hard palate and alveolar ridges; palpation is not recommended for soft palate to avoid triggering the gag reflex
(a) The hard palate, including the incisive papilla, rugae, and palatine fovea, is examined and assessed for:
[1] Shape of the palate—low, high, narrow vault; alterations in shape may require alteration in oral radiographic techniques
[2] Petechiae, torus palatinus, trauma (food burns, denture irritation), stomatitis (nicotine, ulcerative, necrotizing, and denture), fistulas from draining abscesses, denture-related candidiasis (see Chapter 8)
(b) The soft palate is assessed for inflammation, petechiae, trauma, stomatitis, and bifid uvula
(c) Alveolar ridges are assessed for impacted third molars, scarring from third molar extractions, opercula, and exostosis
(5) The oropharynx is assessed by visual inspection with a mouth mirror
(a) The client is asked to say “Ah” to relax and lower the posterior portion of the tongue
(b) The anterior and posterior pillars are assessed for inflammation, petechiae, trauma, stomatitis, and enlarged tonsillar tissues
(6) The floor of the mouth is examined by visual inspection and bimanual palpation
(a) The function of the submandibular gland is tested by wiping each Wharton’s duct with gauze and compressing it with a gloved finger to observe salivary flow
(b) The entire floor of the mouth is palpated; the finger of one hand and the finger and thumb of the other hand are placed under the client’s chin to palpate
(c) Enlargement or masses, Wharton’s duct, sublingual caruncle, and lingual frenum are assessed
(d) Varicosities, tight frenum attachment (ankyloglossia), and blocked salivary duct are inspected
(e) Exostosis along lingual surface of mandible and mandibular tori—significant if interfering with prosthetic appliances
(7) The tongue is examined by visual inspection and digital palpation
(a) The dorsal surface is inspected; the entire tongue is palpated and the lateral borders of the tongue are examined by using gauze to gently hold the tongue
(b) The ventral surface is examined by having the client touch the palate with the tongue
(c) The tongue is assessed for:
[1] Coating on the dorsal surface and the condition of papillae; the extent is assessed
[2] Size; macroglossia associated with Down syndrome or cretinism (see the section on “Down syndrome” in Chapter 19)
[3] Lingual frenum; tight frenum restricting movement (ankyloglossia)
[4] Fissured tongue; deep grooves and crevices along the lateral borders and the dorsal surface; the lateral borders are common sites of oral cancer
[5] Geographic tongue—benign condition in which a sporadic migration of dorsal papilla occurs; tenderness is assessed
[6] Nutritional deficiencies; burning or glossy tongue (see the section on “Abnormalities affecting the tongue” in Chapter 8)
[7] Black hairy tongue related to proliferation of filiform papillae; caused by irritants such as smoking and alcohol (see the section on “Abnormalities affecting the tongue” in Chapter 8)
[8] Hairy leukoplakia caused by extensions of keratin on the lateral borders of the tongue; associated with human immunodeficiency virus (HIV) infection
[9] Atypical lesions, including aphthous ulcerations, trauma-associated fibroma, hemangiomas, and white plaque
Assessment of Dentition
A Purpose—to assess and document the exact location and condition of teeth, restorations, and dental caries, noting normal and abnormal findings on detailed dentition chart; used for care planning, communication with the client, legal documentation, forensic use, and financial audits; composed of study models, occlusion assessment, dentition charting, pulpal vitality testing, and stain determination, (see Chapter 5)
B Components of dentition assessment include:
1. Study models—impressions for study models taken to obtain visual reproduction of teeth, gingiva, and adjacent intraoral structures and to assist with dentition and periodontal charting
2. Occlusion assessment—presence of malocclusion or tooth position determined; signs of parafunctional habits resulting in occlusal traumatism noted (see the sections on “Intra-arch and interarch relationships” in Chapter 5 and “Clinical assessment of the periodontium” in Chapter 14)
3. Dentition charting—graphic representation of the client’s teeth at assessment; includes developmental anomalies and defects, condition of teeth, dental caries activity, restorative history, and other problems; a combination of radiographs and direct visual inspection is used to assist with accurate recording of tooth assessment (Box 15-2); office guides and professional organizations’ dentition charting symbols may be adopted for use; the ADA’s National Board Dental Examination (NBDE) provides a dental charting symbol key in each client case used.
a. Universal Numbering System—most widely used notation system; permanent teeth numbered from 1 to 32 and primary teeth lettered from A to T; 1 to 16 or A to J are located on the maxillary arch, moving right to left; 17 to 32 or K to T are located on the mandibular arch, moving left to right (from the client’s perspective)
b. Developmental anomalies that affect enamel and dentin, developmental defects that affect tooth shape, number of teeth, and tooth size are noted (see the section on “Abnormalities of teeth” in Chapter 8)
c. Tooth positions, eruption patterns, and missing teeth are recorded (see the sections on “Eruption” and “Intra-arch and interarch relationships” in Chapter 5)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses