Dental Caries, Pulp and Periapical Lesions
Definition and Etiology
Dental caries is derived from the Latin word caries which means decay or rotten.
Miller’s Chemicoparasitic Theory/Acidogenic Theory
Role of carbohydrates
Sucrose is readily fermented by the cariogenic bacteria (mainly Streptococcus mutans) to produce acids, which can demineralize the tooth. S. mutans use sucrose to synthesize an extracellular insoluble polysaccharide with the help of the enzyme ‘dextran’, which helps in adhering the plaque firmly on to the tooth surface.
Sucrose Chelation Theory
This theory proposes that if there is a very high concentration of sucrose in the mouth of a caries-active individual, there can be formation of complex substances like calcium saccharate and calcium complexing intermediaries by the action of phosphorelating enzymes. These complexes cause release of the calcium and phosphorus ions from the enamel and thereby resulting in tooth decay.
Contributory Factors in Dental Caries
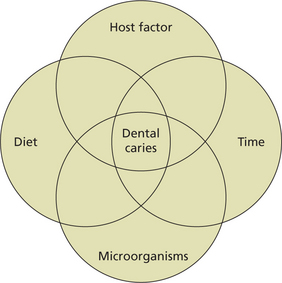
The four factors contributing to the caries process are (Figure 1):
Tooth Factor
Saliva
Salivary flow rate, pH and buffer capacity
Antibacterial activity
The primary oral innate defense factors are peroxidase systems, lysozyme, lactoferrin, and histatins. In vitro studies have shown that these proteins are known to limit bacterial or fungal growth, interfere with bacterial glucose uptake or glucose metabolism and promote aggregation and, thus eliminate bacteria. Hanstrom et al (1983) and Tenovuo and Larjava (1984) reported that the salivary peroxidase and myeloperoxidase systems eliminate H2O2, which is highly toxic for mammalian cells.
Substrate and Dietary Factors
The role of diet in the causation of dental caries has been extensively studied.
A variety of dietary factors have been implicated in the causation of dental caries.
Chemical nature of diet
Teeth may be poorly calcified in individuals exposed to low doses of calcium during intrauterine life and infancy. Such poorly calcified teeth may be susceptible to carious attack. Higher levels of selenium is known to predispose to the carious lesions affecting permanent teeth.
Role of heredity
Senpuku et al (1998) and Acton et al (1999) have correlated specific HLA-DR types with binding S. mutans antigens and S. mutans colonization.
Acton concluded that ‘genes within MHC modulate the level of oral cariogenic organisms’.
Classification of Dental Caries
According to Morphology of Teeth
i. Pit and fissure caries (also called type-1 caries): Caries occurring on anatomical pits and fissures of all the teeth. The specific areas or surfaces involved include occlusal surfaces of molars (Figure 2) and premolars, buccal and lingual surfaces of molars (Figure 3) and lingual surfaces of maxillary incisors.

Figure 2 Pit and fissure carious lesion on the occlusal surface of a mandibular molar. Courtesy: Department of Oral pathology, MCODS Mangalore
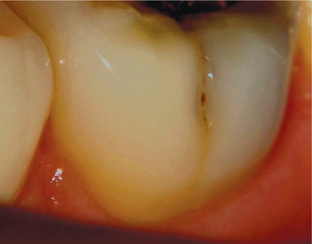
Figure 3 A carious lesion on the buccal surface of the mandibular molar. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
ii. Smooth surface caries (also known as type-2 caries): These carious lesions occur on the smooth surfaces of the teeth (e.g. proximal surfaces or gingival areas of the buccal and lingual aspect of tooth).
The white spot lesion becomes pigmented yellow or brown and it often extends buccally and lingually.
The surrounding enamel becomes bluish white as the lesion continues to progress (Figure 4). The surface of the affected enamel becomes rough and later on, there is formation of a cavity (Figure 5).

Figure 4 The early stages of a proximal carious lesion. The surface of the enamel reveals a bluish-black hue with no discontinuity of the enamel surface. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore

Figure 5 Proximal surface carious lesion. Courtesy: KLE Society’s Institute of Dental Sciences, Bangalore
iii. Root caries: Caries occurring at the cementoenamel junction or cementum. This occurs predominantly in the older age when there is gingival recession.
iv. Linear enamel caries: Caries occurring on the labial surfaces of anterior teeth. This is also known as ‘odontoclasia’. The caries occurs at neonatal zone because of trauma at birth or metabolic disturbances.
According to Severity and Progress
i. Incipient caries: Initial carious lesion limited to the teeth is called incipient caries and is characterized by a virtually intact surface but a porous subsurface (subsurface demineralization).
ii. Rampant caries: This is an acute fulminating type of carious process, which is characterized by simultaneous involvement of multiple number of teeth (may be all teeth) in multiple surfaces (Figure 6A, B).
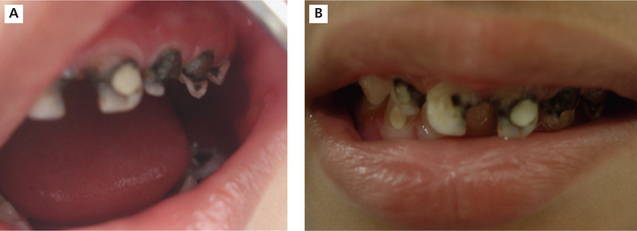
Figure 6 Extensive destruction of teeth in child suffering from rampant caries. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
• Rapid coronal destruction occurs within a short span of time, causing early involvement of the pulp.
• The common age of occurrence is 4–8 years for the deciduous teeth and 11–19 years for the permanent teeth.
• It can even occur in persons who maintain a good level of oral hygiene regularly.
• Moreover, this type of caries attacks those surfaces of teeth, which are otherwise considered immune to the disease.
• Any carious lesion usually an incipient one may become arrested, if there is a change in oral environment. Arrested caries, clinically appears as a dark brown pigmentation with smooth surface, referred to as ‘eburnation’, which is a Latin word that means arrested caries.
iv. Recurrent caries: It occurs at the interface of tooth and restorative material because of many factors such as defective cavity preparation, microleakage and combination of these (Figure 7).

Figure 7 Recurrent carious lesion beneath faulty restorations. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
v. Radiation caries: One of the complications of radiotherapy of oral cancer lesions is xerostomia, which leads to an early development of widespread caries.
According to Age Pattern
1. It has been variously attributed to prolonged use of
2. Invariably there is a prolonged habitual use of one of the above after 1 year of age, usually as an aid for sleeping at night or naptime.
3. Clinically presents as widespread destruction of deciduous teeth, most commonly the four maxillary incisors, followed by the first molars and then the cuspids if the habit is prolonged.
4. The lower teeth are not usually affected as they remain under the cover of the tongue, so the absence of caries in the mandibular incisors distinguishes this disease from ordinary rampant caries.
5. Both the nursing bottle and rampant cause early pulp involvement.
According to Rapidity
• It is a form of caries which runs a rapid clinical course and results in early pulp involvement by carious process.
• It occurs most frequently in children and young adults, presumably because the dentinal tubules are large and open and show no sclerosis.
• The process is usually so rapid that there is little time for the deposition of secondary dentin.
• Slowly progressing in nature and tends to involve the pulp much later than the acute caries.
• These caries lesions exhibit a large cavity with brownish pigmentation (Figure 8).

Figure 8 Deep occlusal caries with brownish pigmentation. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
• Pain is not a common feature of chronic caries because of the protection afforded by secondary dentin.
• The slow progression of the lesion allows sufficient time for both sclerosis of the dentinal tubules and deposition of secondary dentin in response to the adverse irritation.
Microbiology of Dental Caries
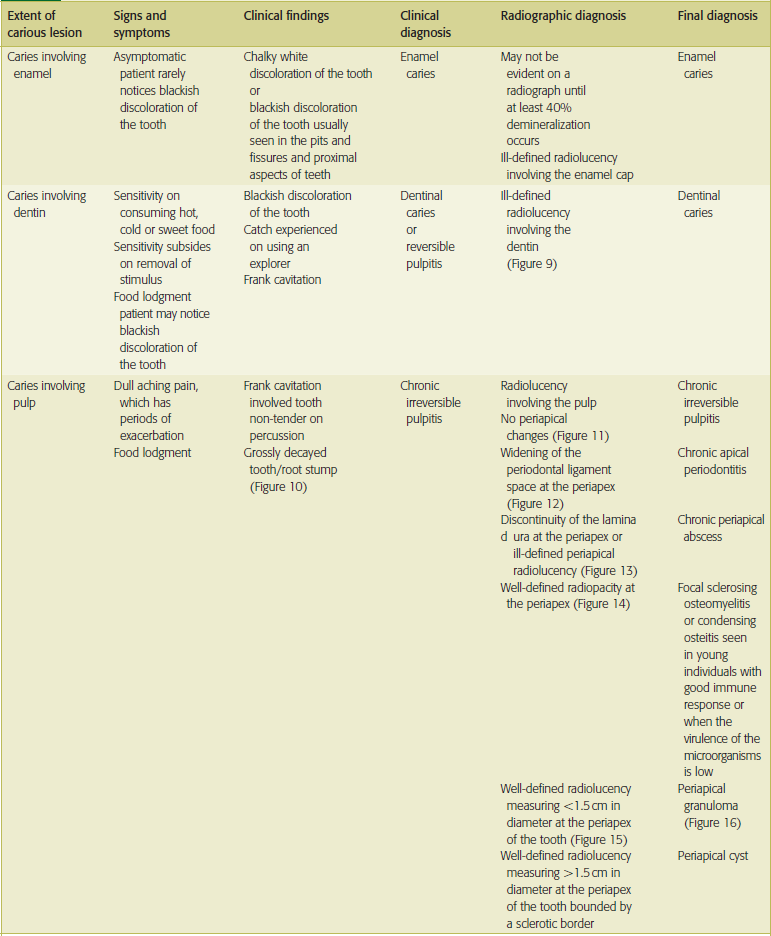
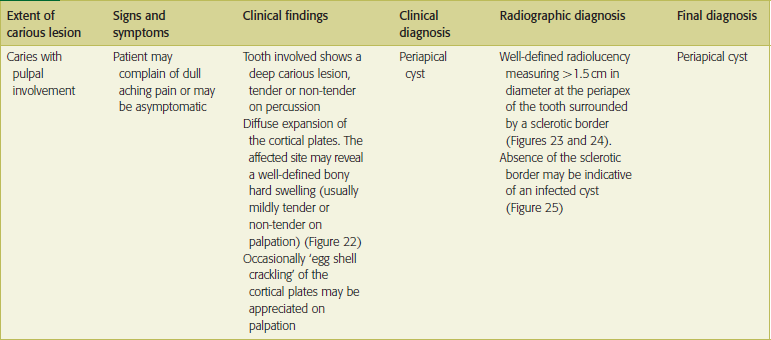
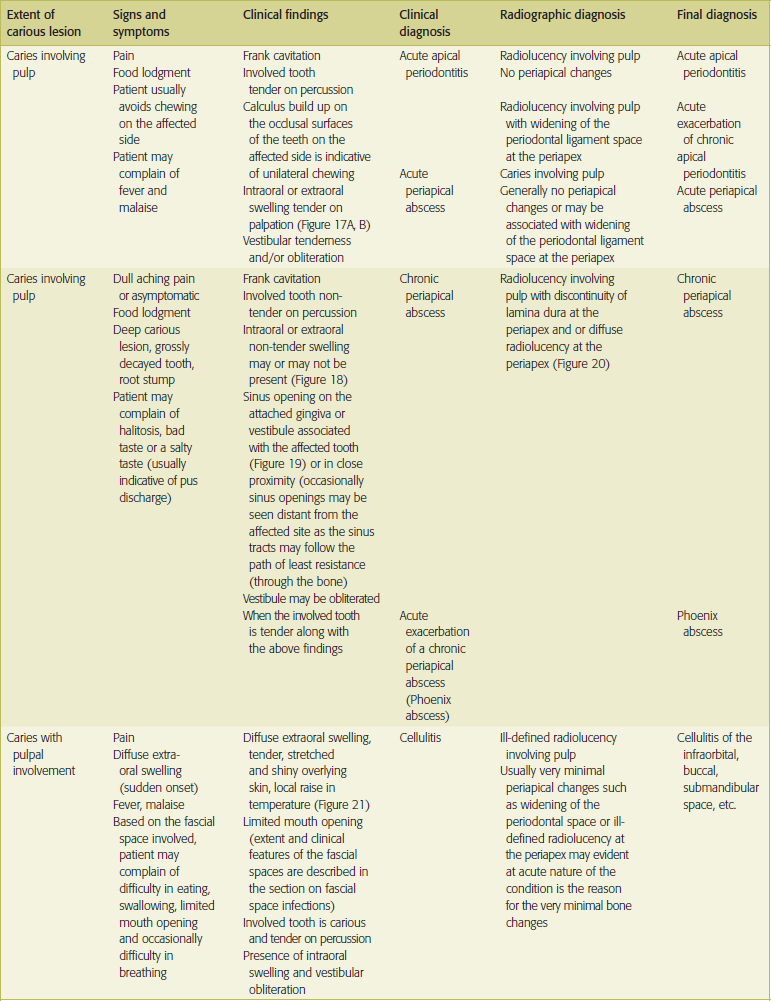
Clinical features of dental caries, pulp and periapical lesions are given in Table 1.
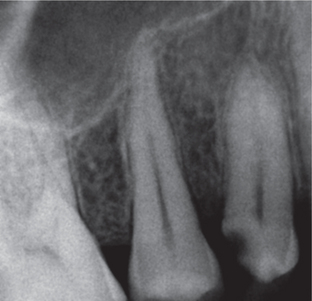
Figure 9 Radiograph showing proximal caries involving dentin suggestive of dentinal caries. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
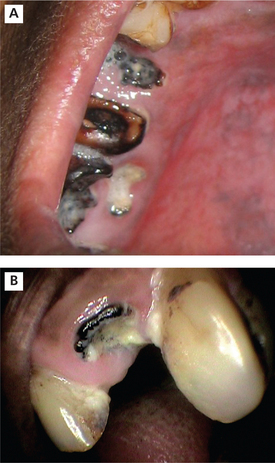
Figure 10 Grossly decayed teeth and root stumps. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
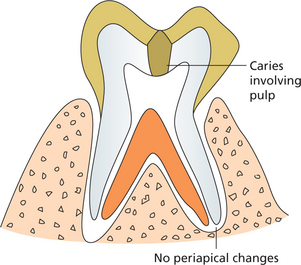
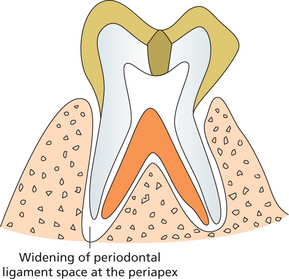
Figure 11 Illustration showing the radiographic features in chronic irreversible pulpitis. Coronal radiolucency involving pulp with no periapical changes
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses