Part 3: The Management of Malocclusion
15
Class I malocclusion
Class I malocclusion is defined as that malocclusion in which the lower incisors occlude on or directly beneath the cingulum plateau of the upper incisors (Figure 2.1). The upper incisor inclination is average and the overjet is 2–3 mm. The anteroposterior relationship is normal, but there may be vertical or transverse malrelationships of the jaws or teeth.
Houston et al.1 quoting Foster and Day (1974) give the percentages of the various malocclusions in a UK population as follows:
- Class I malocclusions – 44%
- Class II division 1 – 27%
- Class II division 2 – 17%
- Class III – 3%
- Indeterminate – 9%.
FEATURES OF CLASS I MALOCCLUSION
Occlusal Features
The incisor relationship is classed as normal (overjet 2–3 mm) although there may be localised transverse discrepancies. The commonest occlusal feature of Class I malocclusion is crowding, while spacing is less common. The canine relationship may be normal or it may be Class II or Class III. The molar relationship may be normal, Class II or Class III.
The vertical relationship may be normal or increased, and marked increase in the vertical dimension may result in an anterior open bite; if the incisor overbite is increased this, by definition, makes it a Class II incisor relationship: sometimes this may be referred to as a ‘deep bite Class I occlusion’. Transversely, there may be a unilateral or bilateral crossbite, which may be dentally related or due to a true transverse skeletal problem. Bimaxillary protrusion (where both cephalometric angles SNA and SNB are increased but ANB is within the normal range) can occur in Class I malocclusion. Bimaxillary proclination is where both the upper and lower incisors are proclined, and the proclined upper incisors will automatically have an increased overjet even if the lower incisors occlude with the middle third of the palatal surface of the upper incisors.
Skeletal Features
A Class I skeletal pattern shows upper and lower jaws of approximately the same size, with a SNA of 80°, SNB of 78°, and an ANB difference of 2°. The maxillo-mandibular planes angle (MMPA) may be increased or average (27°). If the MMPA is decreased there may an increased overbite and a tendency towards a Class II skeletal pattern.
Soft Tissues
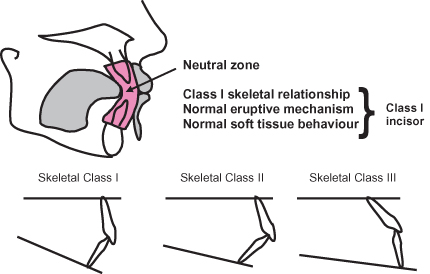
If the jaws are the same size, and there is a normal eruptive mechanism, with a normal soft tissue behaviour pattern, the upper and lower incisors will tend to erupt into a Class I relationship. If there is any change in the vertical or anteroposterior skeletal pattern, the soft tissues may compensate for this, but the dentoalveolar compensatory mechanism can compensate for mild to moderate degrees of skeletal discrepancy in order to achieve a Class I incisal relationship (Figure 15.1).2
Figure 15.1 The dentoalveolar compensatory mechanism (after Solow2).
Growth
Growth of the jaws is usually favourable, with the incisor relationship being maintained. There is a tendency for the mandible to become slightly more prognathic with age, and a mild Class II relationship will tend to improve with time.
Path of Closure
The path of closure is usually direct and unless there are premature occlusal contacts, there will be no deviations or displacements. However, these should be checked for during the clinical examination of the patient, as an apparent Class I malocclusion in centric occlusion may be very different to that in centric relation (which is the maximum retruded contact position of the teeth).
PRINCIPLES OF TREATMENT IN CLASS I MALOCCLUSIONS
The principles of treatment in class I malocclusions are:
- Relief of crowding
- Correction of canine relationships
- Alignment of the incisors
- Space closure
- Detailing of the occlusion.
Relief of Crowding
The commonest way of relieving crowding is by extraction of teeth. In Class I malocclusions, the commonest problem is crowding, and the commonest extraction pattern has traditionally involved the upper and lower first premolars. The reason for this is because these teeth are close to the site of anterior crowding, allowing easier alignment of the canines and incisors. In the past the extraction of the four first premolars (sometimes as part of a serial extraction procedure) was popular where no appliance therapy was contemplated. Spaces will close if the extractions are undertaken at an early age (say around 9–12 years) (Figure 15.2).
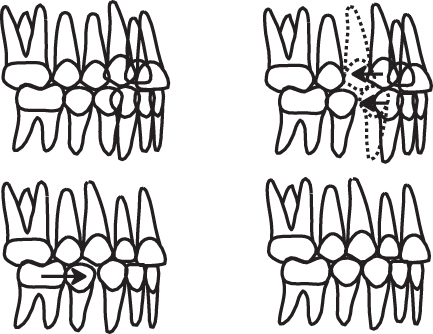
Figure 15.2 Class I malocclusion with upper and lower arch crowding. Upper and lower first premolars are extracted. With orthodontic treatment, canine relationships are then corrected, space closure accomplished, and molars should be in Class I relationship at the end of treatment. In a serial extraction procedure, a similar extraction pattern would take place but one would rely on spontaneous tooth movements to close space and align the teeth. However, complete success in extraction-only cases cannot be predicted or guaranteed.
The extraction of second premolars was undertaken in t/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


